A Cadaveric Exploration for Variations in the Popliteal Fossa Venous Anatomy
Received: 03-Apr-2023, Manuscript No. ijav-23-6356; Editor assigned: 05-Apr-2023, Pre QC No. ijav-23-6356 (PQ); Accepted Date: Apr 21, 2023; Reviewed: 19-Apr-2023 QC No. ijav-23-6356; Revised: 21-Apr-2023, Manuscript No. ijav-23-6356 (R); Published: 28-Apr-2023, DOI: 10.37532/1308-4038.16(4).256
Citation: Newell S, Gay MK. A Cadaveric Exploration for Variations in the Popliteal Fossa Venous Anatomy Popliteal Fossa Venous Anatomy. Int J Anat Var. 2023;16(4):285-289.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Context: The venous system within the popliteal fossa is the main route for draining deoxygenated blood from the leg into the femoral vein. Understanding this system and its variations holds clinical relevance, particularly as it relates to imaging, diagnosis, treatment, and surgery.
Objective: The present study aims to review and describe diverse types of variations within the popliteal fossa venous system, calculate their frequency, and correlate their clinical relevance.
Materials and methods: Bilateral popliteal venous systems were dissected and analyzed in 30 adult embalmed anatomy lab cadavers. Due to ill-preserved venous structures during dissection, three limbs were excluded from this study, totaling the number of lower limbs studied to 57.
Results: Approximately 20% of lower limbs had an anatomical variation within the popliteal fossa venous system. The profunda femoris vein formed a direct connection to the popliteal vein in the popliteal fossa in approximately 9% of cases. Around 5% of lower limbs displayed popliteal vein duplication. The lateral circumflex femoral vein connected to the popliteal vein below the adductor hiatus in 4% of cases, and the popliteal artery coursed superficially to the popliteal vein in 2% of cases.
Conclusion: There are numerous variations in the lower extremity venous anatomy, and each has significant clinical consequences.
Keywords
Popliteal fossa venous; Anatomy variations; Profunda femoris vein; Popliteal arter
INTRODUCTION
The popliteal fossa is a diamond-shaped fat-filled cavity posterior to the knee joint [1]. In addition to lymphatics, the popliteal fossa houses the nerves that provide muscular innervation to the leg and foot and cutaneous innervation for the same area. Usually deep to the nervous structures, arteries traverse the region to supply the leg and foot and provide genicular branches that supply the knee [1]. Aside from the lymphatic system, arteries, and nerves, the popliteal fossa contains a highly variable and clinically relevant venous system.
There are two compartments of the lower extremity venous system: superficial and deep. The superficial compartment contains superficial and perforating veins, such as the great and small saphenous veins, and subcutaneous tissues between the skin and fascia of the muscle [6]. The deep compartment includes tissues deep to the muscular fascia and deep veins, including popliteal, femoral, profunda femoris, peroneal, anterior tibial, and posterior tibial veins [6]. These compartments are separated by fascia and communicate through perforating veins [3]. In most cases, the lower limb veins are paired below the popliteal fossa and continue cranially as the popliteal, femoral, and profunda femoris veins [3].
The venous system in the popliteal fossa includes the termination of the small saphenous vein, the popliteal vein, and the popliteal vein’s tributaries [1]. The small saphenous vein passes from the posterior aspect of the lateral malleolus to the popliteal fossa, where it drains into the popliteal vein [1]. The popliteal vein also drains the anterior tibial vein, posterior tibial vein, and peroneal vein. As the popliteal vein continues superiorly, it will become the femoral vein once it traverses the adductor hiatus [1]. All the while, the popliteal vein lies superficial and close to the popliteal artery within the same fibrous sheath.
Although many variations in this system have been identified, there are no consistently applied classification systems due to varying study populations and modalities [2]. Sadowska observed high origins of the popliteal vein from the coalescence of two or three tributaries, cases of duplication of vein, and the presence of a persistent sciatic vein in a cadaveric sample in Poland [3]. Some of the earliest studies of popliteal fossa variation were conducted by Cockett who illustrated that the single, large popliteal and profunda femoris veins, as depicted in traditional textbooks, are more unusual than previously believed [4]. Obtained through literature review, Cockett reported a “plexiform” variant and another alternative variant where the “lower part of the profunda [femoris] vein is large and unites directly with the popliteal vein or popliteal venous plexus” [4]. In addition to systematic literature reviews and cadaver studies, Park described the topography of the region using computer tomography (CT) venography [5]. Park observed a case of a persistent sciatic vein draining the lower extremities rather than the popliteal and femoral veins [5]. Understanding the veins of the lower extremities and their alternates is of great significance for improving their imaging recognition, pathologic treatment, and prevention of vascular injury during surgery.
While understanding the most common anatomy of the popliteal fossa venous system is essential, further knowledge of variants can improve diagnoses and outcomes of pathologies, such as deep vein thrombosis, phlebitis, and aneurysms. We evaluated dissected bilateral venous systems in the popliteal fossa of 30 anatomy lab cadavers to assess the distinct types of variations and calculate their frequency. We describe these cases’ embryologic origin and clinical significance.
MATERIALS AND METHODS
Bilateral popliteal venous systems were analyzed and dissected in 30 adult embalmed anatomy lab cadavers. Age, sex, and cause of death were the only demographic/health information available for each donor. There were ten female donors (33.3%) and twenty male donors (66.7%). Their ages ranged from 52 to 100 years old. The University of Texas Southwestern Medical Center Willed Body Program provided donors to the Edward Via College of Osteopathic Medicine (VCOM), Louisiana campus, with consent for student education and research. Institutional Review Board (IRB) review was confirmed as not required by the institution’s review board.
Osteopathic medical students from VCOM Class of 2026 dissected the popliteal fossa venous systems during regular coursework. Each venous system was retrospectively reviewed and analyzed for variations in anatomy. Due to ill-preserved venous structures during dissection, three limbs were excluded from this study, totaling the number of limbs studied to 57. The definition of normal anatomy was determined using Moore’s Clinically Oriented Anatomy [1] and Rohen’s Anatomy: A Photographic Atlas [20]. Variant length and diameter measurements, popliteal vein diameter, schematic representations, and photographs were collated to illustrate and describe variations. The recorded diameter was the greatest width along the veins course. The length was the total length from the vein’s origin to termination.
RESULTS
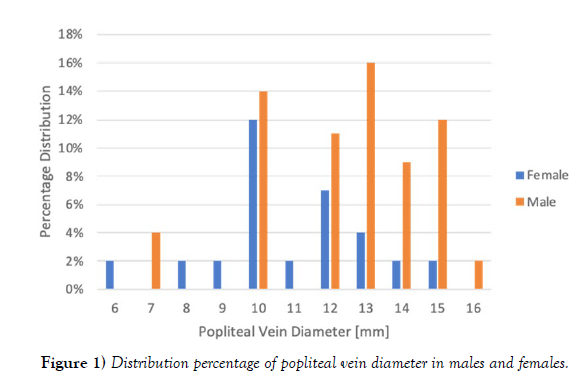
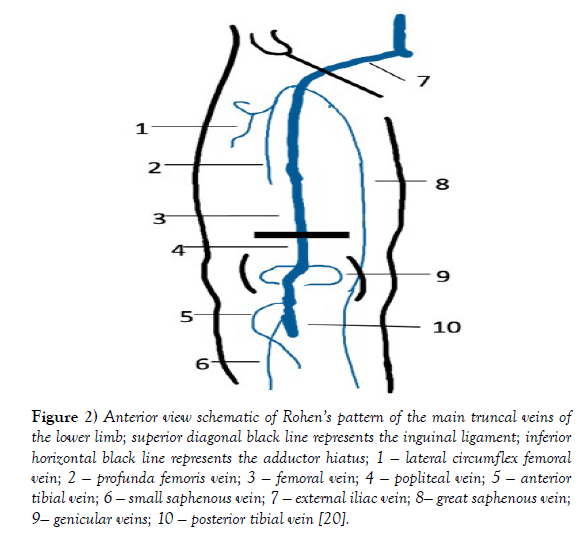
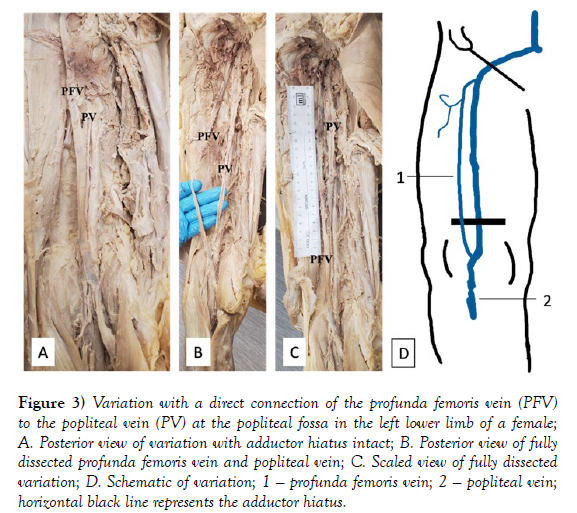
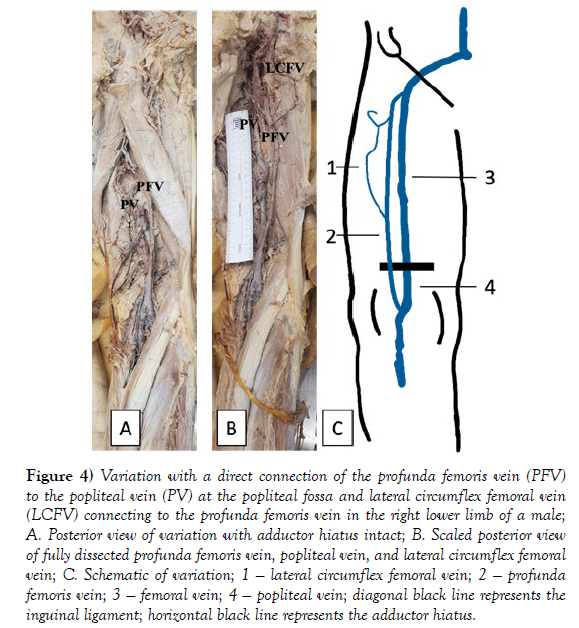
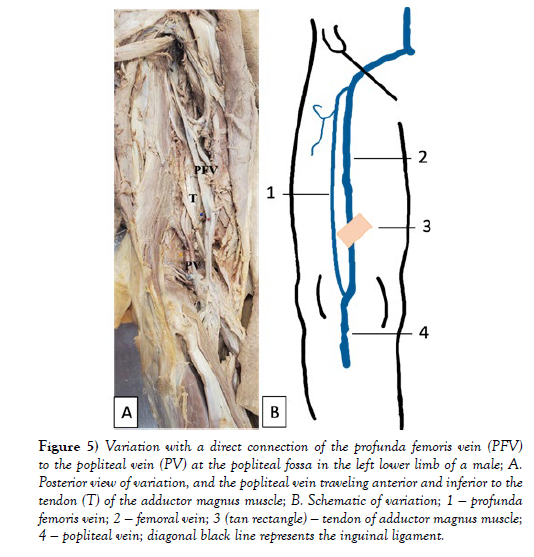
Female popliteal vein diameters ranged from 6 to 15 mm, while popliteal vein diameters ranged from 7 to 16 mm in males (Figure 1). Of the 57 lower extremity limbs, forty-six (80.7%) displayed the classic textbook pattern of the popliteal fossa venous system: 16 female cases and 30 male cases (Figure 2). All variations and their frequencies can be found in Table 1 Of the variations that deviated from the usual presentation, the most common was observed in five cases (8.8%) and was a direct connection of the profunda femoris vein to the popliteal vein at the popliteal fossa (Figures 3-5). The lengths and diameters of the profunda femoris veins are displayed in Table 2. An additional anomalous finding in the left limb of a male donor was the popliteal vein and artery traveling within a hiatus located anterior and inferior to the tendon of the adductor magnus muscle (Figure 5).
Figure 2) Anterior view schematic of Rohen’s pattern of the main truncal veins of the lower limb; superior diagonal black line represents the inguinal ligament; inferior horizontal black line represents the adductor hiatus; 1 — lateral circumflex femoral vein; 2 — profunda femoris vein; 3 — femoral vein; 4 — popliteal vein; 5 — anterior tibial vein; 6 — small saphenous vein; 7 — external iliac vein; 8— great saphenous vein; 9— genicular veins; 10 — posterior tibial vein [20].
| Variation | Female Number of Cases | Male Number of Cases | Total Number of Cases | Frequency |
|---|---|---|---|---|
| Normal | 16 | 30 | 46 | 80.7% |
| Profunda femoris vein connecting directly to the popliteal vein in the popliteal fossa | 1 | 4 | 5 | 8.8% |
| Popliteal vein duplication | 1 | 2 | 3 | 5.2% |
| Lateral circumflex femoral vein connecting to the popliteal vein below adductor hiatus | 0 | 2 | 2 | 3.5% |
| Popliteal artery coursing superficial to the popliteal vein and crossing the posterior tibial vein | 1 | 0 | 1 | 1.8% |
| Total | 19 | 38 | 57 | 100% |
Table 1) Popliteal Fossa Venous Variations.
Figure 3) Variation with a direct connection of the profunda femoris vein (PFV) to the popliteal vein (PV) at the popliteal fossa in the left lower limb of a female; A. Posterior view of variation with adductor hiatus intact; B. Posterior view of fully dissected profunda femoris vein and popliteal vein; C. Scaled view of fully dissected variation; D. Schematic of variation; 1 — profunda femoris vein; 2 — popliteal vein; horizontal black line represents the adductor hiatus.
Figure 4) Variation with a direct connection of the profunda femoris vein (PFV) to the popliteal vein (PV) at the popliteal fossa and lateral circumflex femoral vein (LCFV) connecting to the profunda femoris vein in the right lower limb of a male; A. Posterior view of variation with adductor hiatus intact; B. Scaled posterior view of fully dissected profunda femoris vein, popliteal vein, and lateral circumflex femoral vein; C. Schematic of variation; 1 — lateral circumflex femoral vein; 2 — profunda femoris vein; 3 — femoral vein; 4 — popliteal vein; diagonal black line represents the inguinal ligament; horizontal black line represents the adductor hiatus.
Figure 5) Variation with a direct connection of the profunda femoris vein (PFV) to the popliteal vein (PV) at the popliteal fossa in the left lower limb of a male; A. Posterior view of variation, and the popliteal vein traveling anterior and inferior to the tendon (T) of the adductor magnus muscle; B. Schematic of variation; 1 — profunda femoris vein; 2 — femoral vein; 3 (tan rectangle) — tendon of adductor magnus muscle; 4 — popliteal vein; diagonal black line represents the inguinal ligament.
There was only one bilateral case of the profunda femoris vein joining with the popliteal vein within both popliteal fossae of a male donor. Also notable in this case was the right profunda femoris vein joined with the lateral circumflex femoral vein before draining into the femoral vein (Figure 4B). The approximated total length of the profunda femoris in the left leg was 385 mm with a 14 mm diameter, and the right leg was 334 mm in length with an 8 mm diameter (Table 2).
| Profunda Femoris Vein Case | Profunda Femoris Vein Length [mm] | Profunda Femoris Vein Diameter [mm] |
|---|---|---|
| Female Case | 346 | 6 |
| Male Case 1 | 338 | 14 |
| Male Case 2 | 303 | 8 |
| Male Case 3 - Left | 385 | 14 |
| Male Case 3 - Right | 334 | 8 |
Table 2) Length and Diameter of Aberrant Profunda Femoris Vein.
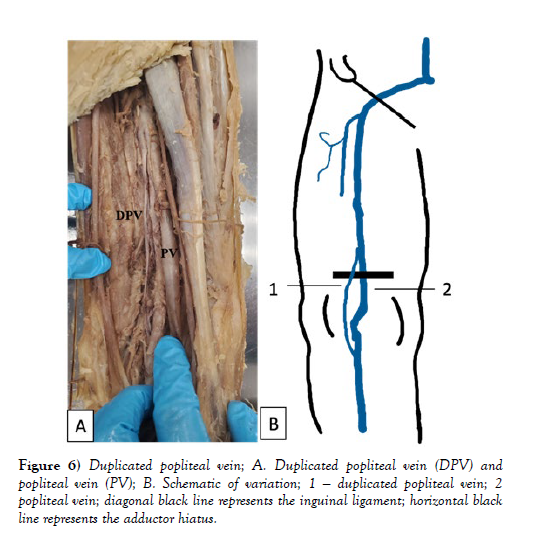
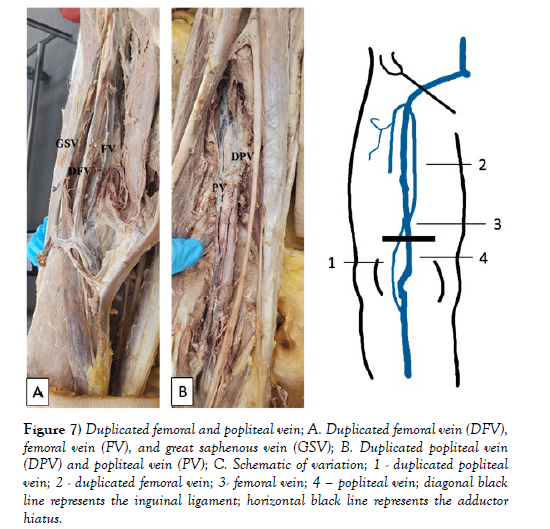
Duplication of the popliteal vein was found in 3 of the 57 cases (5.2%). Unilateral duplicated popliteal veins were discovered in one female and two male cadavers and measured 132 mm, 188 mm, and 142 mm in length, respectively (Figure 6). The duplicated popliteal vein in the female donor converged at the adductor hiatus and then became a duplicated femoral vein with a length of 174 mm (Figure 7).
Figure 7) Duplicated femoral and popliteal vein; A. Duplicated femoral vein (DFV), femoral vein (FV), and great saphenous vein (GSV); B. Duplicated popliteal vein (DPV) and popliteal vein (PV); C. Schematic of variation; 1 - duplicated popliteal vein; 2 - duplicated femoral vein; 3- femoral vein; 4 – popliteal vein; diagonal black line represents the inguinal ligament; horizontal black line represents the adductor hiatus.
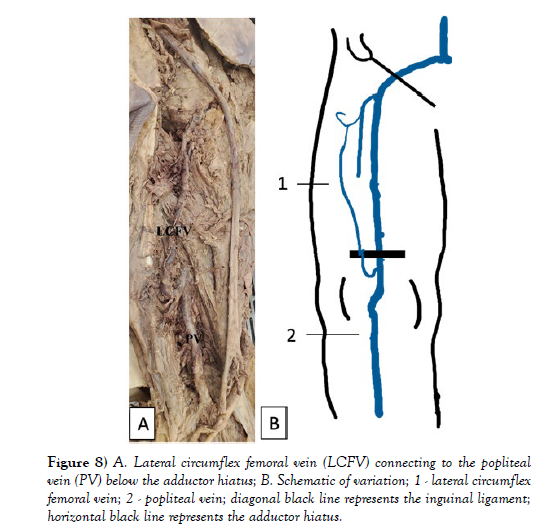
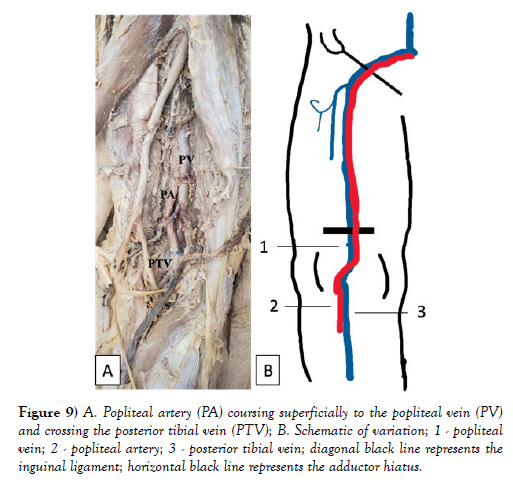
Moreover, in 3.5% of the 57 cases, the lateral circumflex femoral vein terminated at the popliteal vein just below the adductor hiatus (Figure 8). Lastly, a unique variant was the popliteal artery coursing superficially to the popliteal vein and crossing the posterior tibial vein within the popliteal fossa in a female donor (Figure 9).
Figure 8) A. Lateral circumflex femoral vein (LCFV) connecting to the popliteal vein (PV) below the adductor hiatus; B. Schematic of variation; 1 - lateral circumflex femoral vein; 2 - popliteal vein; diagonal black line represents the inguinal ligament; horizontal black line represents the adductor hiatus.
Figure 9) A. Popliteal artery (PA) coursing superficially to the popliteal vein (PV) and crossing the posterior tibial vein (PTV); B. Schematic of variation; 1 - popliteal vein; 2 - popliteal artery; 3 - posterior tibial vein; diagonal black line represents the inguinal ligament; horizontal black line represents the adductor hiatus.
DISCUSSION
The venous system is complex and often contains numerous variations. Acquired conditions and embryological development can both contribute to these variations in the vascular system. Arteriovenous fistulas, peripheral vascular bypass, and varicose veins are some examples of acquired conditions that produce venous variations [7]. These may be due to iatrogenic, traumatic, or idiopathic causes. On the other hand, the embryogenesis of the venous system is not fully understood and precise chain of event studies have not been confirmed by direct observations in human embryos [8].
The limb buds become visible at the end of the fourth week of gestation with the forelimbs appearing one to two days before the hind limbs [9]. By week eight, the embryo has established limb form, innervation, and vasculature [10]. The severity of malformations is related to the stage of embryological development [11]. Therefore, simple anatomical variations occur after the organogenesis period in week eight [8]. Simple anatomical variations typically do not cause pathologies, albeit changes in lifestyle, environmental, or bodily conditions may evoke pathological states in embryologically-derived variants [12].
In this study, approximately 20% of limbs had an anatomical variation within the popliteal fossa venous system. The profunda femoris vein formed a direct connection to the popliteal vein in the popliteal fossa in 9% of cases. Around 5% of lower limbs displayed popliteal vein duplication, the lateral circumflex femoral vein connected to the popliteal vein below the adductor hiatus in 4% of cases, and the popliteal artery coursed superficially to the popliteal vein in 2% of cases. Due to their location, these variations have important clinical implications in deep vein thrombosis and other venous pathologies. The popliteal vein is one of the most common locations for deep vein thrombosis (DVT) [6]. Additional pathologies of the lower extremity veins include venous insufficiency, aneurysms, and hemorrhage from trauma [13]. Moreover, lower extremity venous systems are susceptible to arteriovenous fistulas, varicosities, thrombophlebitis, and phlebothrombosis [14].
Duplication of the femoral and popliteal venous systems may lead to false negatives in DVT studies and, therefore, the misdiagnosis of thromboembolic disease and delay of treatment [15]. Another example is the popliteal artery crossing the popliteal vein superficially in the popliteal fossa could lead to popliteal entrapment syndrome (PES). Although the popliteal artery is the most widely recognized involved structure in PES, popliteal vein entrapment can also create a set of symptoms related to compression of the neurovascular bundle in the popliteal fossa [16]. The most common presenting symptom of PES is limb swelling [16]. PES may also present with knee edema, leg heaviness, varicosities, pain with ambulation, dermal hyperpigmentation, and venous ulceration [16].
In other situations, variations can pose a protective factor against pathologies. Referred to as axial transformation, the enlargement of collateral anastomosis between the profunda femoris and popliteal vein can serve as collateral circulation in cases of popliteal vein obstruction [17]. Likewise, the lateral circumflex femoral vein connecting distally to the popliteal vein can also serve as collateral circulation to an obstructed popliteal vein. The bilateral case of the profunda femoris vein connecting directly to the popliteal vein exemplified these collateral circulation routes. There was a diameter discrepancy in profunda femoris and popliteal vein for the left lower limb (14 mm and 7 mm, respectively) compared to the right (8 mm and 14 mm, respectively). The enlarged left profunda femoris vein in the left lower limb may indicate axial transformation occurred to serve as collateral circulation for an obstructed popliteal vein.
It is also crucial to understand popliteal fossa venous system variations not only for pathological diagnosis and treatment but also for surgical and procedural applications. Posterior knee approaches are less likely to be performed due to the increased risk of neurovascular injury. However, posterior knee approaches occur for Baker cyst excision, fracture and avulsion repair, cartilage and meniscal repair, loose body removal, and neurovascular repair [18]. Even with innovative approaches to surgery, such as a posteromedial incision or procedures through the popliteal vein, it is vital to have an in-depth knowledge of anatomical variations [19-20].
CONCLUSION
The popliteal fossa venous system is complex and can accommodate different variations. These variations are known to be commonplace and clinically overlooked due to silent presentations. An understanding of this system and its variants will improve diagnosis, treatment, and surgical outcomes. Through studying 57 limbs from 30 cadavers, we discovered several distinct types of variations, calculated their frequency, and described these cases’ clinical significance.
ETHICAL APPROVAL
IRB review was confirmed as not required by the institute’s review board as it involves cadaveric research.
INFORMED CONSENT
All donors provided general research consent under their donation to the University of Texas Southwestern’s Willed Body Program.
AUTHOR CONTRIBUTIONS
Savannah Newell provided substantial contributions to conception, design, and acquisition of data; Marti Gay provided substantial contribution to acquisition, analysis, and interpretation of data; Marti Gay drafted the article; Savannah Newell revised the article critically for important intellectual content; Savannah Newell gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ACKNOWLEDGEMENT
The authors of this paper would like to thank the University of Texas Southwestern’s Willed Body Program and the donors for their donation, as well as the Edward Via College of Osteopathic Medicine Class of 2026 for their work exposing the anatomy during their anatomy coursework.
REFERENCES
- Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. 8th ed. Wolters Kluwer; 2018.
- Yadgire GS, Rawlani S, Chauhan AMS, Rawlani M. Variation of Venous System in Popliteal Fossa. Indian J Anat. 2016; 5(1):79-82.
- Sadowska A, Spodnik JH, Wójcik S. Variations in popliteal fossa venous anatomy: implications for diagnosis of deep-vein thrombosis. Folia Morphol (Warsz). 2013; 72(1):51-56.
- Cockett FB. Abnormalities of the Deep Veins of the Leg. Postgrad Med J. 1954; 30(348):512-543.
- Park EA, Chung JW, Lee W. Three-Dimensional Evaluation of the Anatomic Variations of the Femoral Vein and Popliteal Vein in Relation to the Accompanying Artery by Using CT Venography. Korean J Radiol. 2011; 12(3):327.
- Sawyer E, Sinkler MA, Tadi P. Anatomy, Bony Pelvis and Lower Limb, Popliteal Vein. PubMed. 2021.
- Ying A, Al-Asady R, Vicaretti M. Endovascular treatment of a large iatrogenic popliteal arteriovenous fistula. Journal of Vascular Surgery Cases, Innovations and Techniques. 2020; 6(1):129-132.
- UHL JF. Focus on venous embryogenesis of the human lower limbs. Servier - Phlebolymphology. 2015.
- Silverman AJ. Limb Development. 2004.
- Sadler TW, Langman J. Langman’s Medical Embryology. 14th ed. Wolters Kluwer. 2019.
- Behravesh S, Yakes W, Gupta N. Venous malformations: clinical diagnosis and treatment. Cardiovasc Diagn Ther. 2016; 6(6):557-569.
- Kachlík D, Varga I, Báča V, Musil V. Variant Anatomy and Its Terminology. Medicina (Kaunas). 2020; 56(12).
- De Popas E, Brown M. Varicose Veins and Lower Extremity Venous Insufficiency. Seminars in Interventional Radiology. 2018;35(01):056-061.
- Kumar V, Abbas AK, Aster JC. Robbins and Cotran Pathologic Basis of Disease. 10th ed. Saunders Elsevier; 2021.
- Simpson W, Krakowsi D. Prevalence of lower extremity venous duplication. Indian J Radiol Imaging. 2010; 20(3):230.
- Chen CK, Kolber M. Venous popliteal entrapment syndrome. Cardiovasc Diagn Ther. 2021; 11(5):1168-1171.
- Raju S, Fountain T, Neglén P, Devidas M. Axial transformation of the profunda femoris vein. J Vasc Surg. 1998; 27(4):651-659.
- Faucett SC, Gannon J, Chahla J, Ferrari MB, LaPrade RF et al. Posterior Surgical Approach to the Knee. Arthrosc Tech. 2017; 6(2):e391-e395.
- Kim H, Yim N, Kim J, Kang Y, Jung H et al. Inferior vena cava filter insertion through the popliteal vein: enabling the percutaneous endovenous intervention of deep vein thrombosis with a single venous approach in a single session. Diagn Interv Radiol. 2016; 27(3):S287.
- Rohen JW, Chihiro Yokochi, Lütjen-Drecoll E. Photographic Atlas of Anatomy. 8th ed. Philadelphia Wolters Kluwer; 2016.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref