A case of bilateral persistent median artery associated with a rightsided duplicate palmaris longus muscle
Received: 11-Oct-2017 Accepted Date: Nov 01, 2017; Published: 07-Nov-2017
Citation: Katrikh AZ, Stark E. A case of bilateral persistent median artery associated with a right-sided duplicate palmaris longus muscle. Int J Anat Var. 2017;10(4):77-8.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
We present a rare case of the simultaneous presence of bilateral persistent median artery and right-sided duplicate palmaris longus identified in a 72-year-old Caucasian male cadaver during routine anatomical dissection at the David Geffen School of Medicine at UCLA. Both persistent median arteries were located in a fibrous sheath accompanying the median nerve through the carpal tunnel. They originated as a branch of the ulnar artery and anastomosed with the superficial palmar arch in the hand. In addition to a normal palmaris longus muscle with usual attachments, a duplicate muscle was examined ulnar to the typical, originating at the common flexor tendon of the medial epicondyle of the humerus, and distally attaching to the flexor retinaculum. This case has clinical relevance for surgical management of carpal tunnel syndrome and tendon graft procedures.
Keywords
Persistent median artery; Duplicate palmaris longus muscle; Carpal tunnel syndrome
Introduction
The presence of a Persistent Median Artery (PMA) in the adult forearm is due to failure in normal regression of vasculature during gestation. According to Rodriguez-Niedenfuhr et al [1] the median artery normally undergoes retrogression following the first trimester of pregnancy into a small vessel that supplies the median nerve. A failure of apoptosis results in a PMA that travels through the carpal tunnel with the associated nerve and most commonly anastomoses with the superficial palmar arch. Natsis et al [2] completed an exhaustive literature review of cases of PMA identified between 1953 and 2009.
The palmaris longus muscle in the forearm is one of the most variable muscles in the body. The typical palmaris longus muscle originates at the common flexor tendon of the medial epicondyle and has a tendinous insertion on the palmar aponeurosis. The most common variation to the muscle is agenesis, with one study showing an overall prevalence of absence in 26.6% of cases [3]. A recent study conducted by Georgiev et al [4] classifies variations in the muscle as belonging to two anatomical categories. The first describes any change in the normal position or the existence of an accessory muscle belly. The second category consists of variations to the tendon or an accessory muscle. In this case, in addition to complete absence, the palmaris longus muscle can be duplicate or triplicate. Similarly, the tendon can bifurcate or trifurcate and insert into the same or different sites.
Case Report
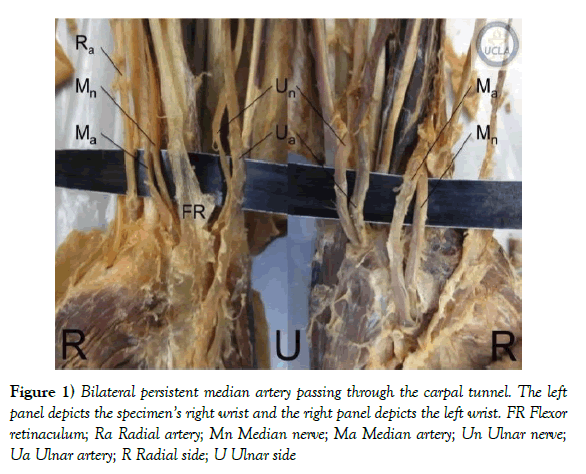
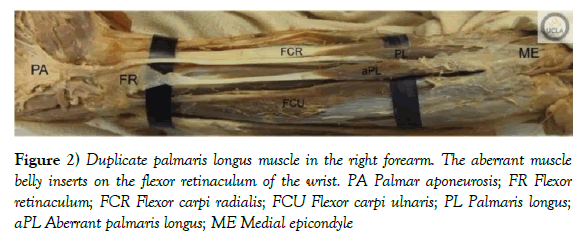
During routine anatomical dissection of a 72-year-old Caucasian male in the instructional gross anatomy laboratory of the David Geffen School of Medicine at UCLA a case of bilateral PMA along with right-sided duplicate PL muscle was observed. The median arteries on both sides traveled in a fibrous connective sheath with the median nerve through the carpal tunnel (Figure 1). Both arteries were tributaries of the ulnar artery and shared the same diameter as their respective median nerves (0.3 cm on the right side and 0.4 cm on the left side). In both cases the artery was situated anterior to the nerve in the carpal tunnel. In the right forearm, a duplicate muscle belly arose on the ulnar side of the normal PL. Both muscle bellies originated at the common flexor tendon, and the aberrant muscle belly inserted on the flexor retinaculum, while the normal PL distal attachment was unremarkable (Figure 2). The morphology of the two muscle bellies and tendons is summarized in Table 1. The two muscle bellies and tendons were equal in width. The lengths varied due to the separate attachments to the palmar aponeurosis and flexor retinaculum.
Figure 1) Bilateral persistent median artery passing through the carpal tunnel. The left panel depicts the specimen’s right wrist and the right panel depicts the left wrist. FR Flexor retinaculum; Ra Radial artery; Mn Median nerve; Ma Median artery; Un Ulnar nerve; Ua Ulnar artery; R Radial side; U Ulnar side
Figure 2) Duplicate palmaris longus muscle in the right forearm. The aberrant muscle belly inserts on the flexor retinaculum of the wrist. PA Palmar aponeurosis; FR Flexor retinaculum; FCR Flexor carpi radialis; FCU Flexor carpi ulnaris; PL Palmaris longus; aPL Aberrant palmaris longus; ME Medial epicondyle
| Morphology | Typical Palmaris Longus | Aberrant Palmaris Longus |
|---|---|---|
| Origin | Common flexor tendon | Common flexor tendon |
| Insertion | Palmar aponeurosis | Flexor retinaculum |
| Muscle Belly Length | 11.3 cm | 14.2 cm |
| Tendon Length | 16.6 cm | 8.3 cm |
| Muscle Belly Width | 1.1 cm | 1.1 cm |
| Tendon Width | 0.4 cm | 0.4 cm |
The muscle belly and tendon width was measured at the widest point. The lengths were measured from origin at the common flexor tendon to the musculotendinous junction to the distal insertion of the tendon
Table 1: Morphology of the typical and aberrant palmaris longus
Discussion and Conclusion
Natsis et al [2] published a literature review of 53 studies that reported the incidence of PMA in either cadavers or operative patients. Taking these reports together, a sample size of 5764 upper limbs of adults were observed with an incidence of 365 of PMA, or 6.3% overall incidence. This is excluding all neonatal cadavers dissected, which have a much higher incidence of PMA (65 of 180, or 36%). Of the cases that reported whether the PMA was unilateral or bilateral, 123 reported the former, and 29 incidences of the latter were observed, making bilateral PMA, as is our case, a rarer finding. The PMA is most commonly a branch of the ulnar artery, followed by the common interosseus, brachial, anterior interosseus, and radial arteries in terms of descending incidence, making our case in the majority.
the carpal tunnel and has been associated with carpal tunnel syndrome in many cases. The presence of a large pulsating median artery in the adult can cause compression of the median nerve at the carpal tunnel, mimicking symptoms of the syndrome [5]. Toranto [6] described a case in which an aneurism formed in the artery causing carpal tunnel syndrome. Additionally other cases have been reported where a thrombus [7] or a calcification [8] in the artery caused compression of the nerve, which presented with downstream motor and sensory loss of the median nerve distribution.
Variants to the PL have also been linked to median nerve compression in many case reports [9,10]. According to the new classifications by Georgiev et al [4] our case of muscle duplication would belong to the second anatomic category. This study also separates variations in PL into two clinical classifications: those correlated to nerve compression, or related to reconstructive surgery. Our case of duplicate PL would fall under the latter, as the duplicate muscle tendon would be available for additional tendon graft procedures.
To our knowledge our case is the only report of bilateral persistent median artery and a right-sided double palmaris longus occurring simultaneously (MEDLINE; 1920–2017; English language; search terms: “persistent median artery,” and “palmaris longus”). In this case, it is feasible that the presence of the PMA could have caused compression of the median nerve, although no detailed medical history was obtained and carpal tunnel syndrome was not recorded. The PMA was the same diameter as the nerve and closely adhered to it in a tough fibrous sheath that enclosed both structures. In the carpal tunnel of both upper limbs, the nerve was located tightly between the artery and the tendons of flexor digitorum profundus and flexor pollicis longus, increasing the likelihood of compression (Figure 1). The distal attachment of the variant palmaris longus to the flexor retinaculum (Figure 2) in the right forearm could increase the tension in the anterior boundary of the carpal tunnel, further decreasing the size of the already tightly packed space. The existence of a PMA and variants in the palmaris longus are not uncommon occurrences. The latter is commonly used as an autologous donor site for tendon repair, and therefore knowledge of variation in the anatomy of that muscle is critical for any surgeon utilizing the palmaris longus tendon. Furthermore, it is essential that any surgeon performing carpal tunnel release or any other procedure in the forearm and hand be aware of the related anatomy of the median artery, should it be persistent in that patient.
Acknowledgement
We would like to thank the individuals who graciously and generously donate their remains to UCLA for education and research purposes. We would also like to thank the Donated Body Program staff for the work they do in preserving and caring for UCLA donors’ remains.
REFERENCES
- Rodriguez-Niedenführ M, Burton GJ, Deu J, et al. Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. J Anat. 2001;199:407-17.
- Natsis K, Lordache G, Gigis I, et al. Persistent median artery in the carpal tunnel: anatomy, embryology, clinical significance, and review of the literature. Folia Morphol. 2009;68:193-200.
- Kose O, Adanir O, Cirpar M, et al. The prevalence of absence of the palmaris longus: a study in Turkish population. Arch Orthop Trauma Surg. 2009;129:609-11.
- Georgiev GP, Iliev AA, Dimitrova IN, et al. Palmaris longus muscle variations: clinical significance and proposal of new classifications. Folia Medica. 2017;59:Ahead of print.
- Bilgin SS, Olcay SE, Derincek A, et al. Can simple release relieve symptoms of carpal tunnel syndrome caused by a persistent median artery? Clinical experience. Arch Orthop Trauma Surg. 2004;124:154-6.
- Toranto IR. Aneurysm of the median artery causing recurrent carpal tunnel syndrome and anatomic review. Plast Reconstr Surg. 1989;84:510-2.
- Khashaba A. Carpal tunnel syndrome from thrombosed persistent median artery. J Emerg Med. 2002;22:55-7.
- Dickinson JC, Kleinert JM. Acute carpal-tunnel syndrome caused by a calcified median artery. J Bone Joint Surg. 1991;73A:610-1.
- Cope JM, Looney EM, Craig CA. Median nerve compression and the reversed palmaris longus. Int J Anat Var. 2009;2:102-4.
- Seyhan T. Median nerve compression at the wrist caused by reversed 3-headed palmaris longus muscle: case report and review of the literature. Am J Orthop. 2005;34:544-6.