A Case Report on Clinical Anatomy: Unusual Variation in the Renal Vasculature
Received: 04-Jun-2023, Manuscript No. ijav-23-6532; Editor assigned: 05-Jun-2023, Pre QC No. ijav-23-6532 (PQ); Accepted Date: Jun 23, 2023; Reviewed: 19-Jun-2023 QC No. ijav-23-6532; Revised: 23-Jun-2023, Manuscript No. ijav-23-6532 (R); Published: 30-Jun-2023, DOI: 10.37532/1308-4038.16(6).274
Citation: Hvizdosova N. A Case Report on Clinical Anatomy: Unusual Variation in the Renal Vasculature. Int J Anat Var. 2023;16(6):323-324.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This case report highlights an unusual anatomical variation of the renal vasculature observed during a routine anatomical dissection. The presence of accessory renal arteries and veins, along with their branching patterns, were meticulously documented and analyzed. This case report emphasizes the importance of understanding such anatomical variations to avoid complications during renal surgeries and interventions. The unique anatomical features observed in this case contribute to the existing body of knowledge on renal vascular anatomy and call for further exploration of such variations.
Keywords
Clinical anatomy; Renal vasculature; Accessory renal arteries; Accessory renal veins; Anatomical variations; Renal surgery
INTRODUCTION
Anatomical variations are commonly encountered in clinical practice and have significant implications for surgical procedures and interventions. Adequate knowledge of the anatomical variations in various organ systems, including the renal vasculature, is crucial for surgeons, radiologists, and other healthcare professionals involved in the diagnosis and treatment of renal disorders. This case report presents a rare anatomical variation in the renal vasculature, emphasizing the importance of thorough anatomical knowledge and its implications in clinical settings. The renal vasculature, comprising the arteries and veins supplying the kidneys, is no exception to anatomical variations [1]. The kidneys, being vital organs responsible for filtration and regulation of body fluids, receive a rich blood supply to fulfill their physiological functions. The understanding of renal vascular anatomy is of paramount importance for surgeons, interventional radiologists, and clinicians involved in renal surgeries, renal transplantations, and other therapeutic interventions targeting renal disorders [2].
Anatomical variations in the renal vasculature can pose challenges during surgical procedures, potentially leading to complications such as bleeding, ischemia, or damage to adjacent structures. Surgeons must possess detailed knowledge of the normal and variant anatomical structures to navigate the complexities of renal surgeries effectively [3]. Accurate preoperative identification of anatomical variations through imaging techniques, such as computed tomography angiography (CTA) or magnetic resonance angiography (MRA), can assist surgeons in planning procedures and anticipating potential difficulties.
In this case report, we present an unusual anatomical variation in the renal vasculature encountered during a routine anatomical dissection. The identification and documentation of accessory renal arteries and veins, along with their branching patterns, provide valuable insights into the variability of renal vascular anatomy. By sharing this case, we aim to enhance the understanding of such variations and emphasize the significance of anatomical knowledge in clinical practice [4-5].
CASE REPORT
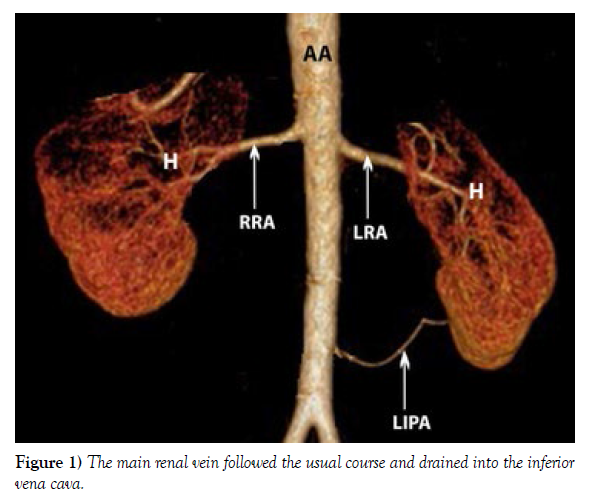
During a routine anatomical dissection conducted on a cadaver, an unusual variation in the renal vasculature was identified. The right kidney exhibited accessory renal arteries and veins in addition to the normal renal vasculature. The primary renal artery arose from the abdominal aorta, as expected, and bifurcated into an upper and lower branch. However, the upper branch gave rise to two additional accessory renal arteries, while the lower branch proceeded as the main renal artery. The accessory renal arteries were smaller in diameter compared to the main renal artery and exhibited distinct branching patterns. The main renal vein followed the usual course and drained into the inferior vena cava; however, there were two accessory renal veins originating from the upper and lower poles of the kidney (Figure 1).
DISCUSSION
The presence of accessory renal arteries and veins is not uncommon, with reported prevalence ranging from 20% to 50% in various studies. These variations often result from embryonic developmental processes, and their recognition is crucial to avoid inadvertent damage during surgical procedures involving the renal vasculature. In this case, the presence of accessory renal arteries could have potential implications for renal surgeries, such as renal artery embolization or nephron-sparing surgeries, as well as for renal transplant procedures. The knowledge of such anatomical variations is vital for surgeons to plan appropriate interventions and minimize the risk of complications [6].
The branching pattern of the accessory renal arteries in this case report is noteworthy [7]. The upper branch of the main renal artery gave rise to two additional accessory renal arteries, one supplying the upper pole and the other supplying the mid-pole of the kidney. The lower branch continued as the main renal artery, supplying the lower pole. Understanding these variations is essential during surgeries involving segmental resections or partial nephrectomies to ensure preservation of the blood supply to specific regions of the kidney [8].
The presence of accessory renal veins also merits attention. While variations in renal venous drainage are less common than arterial variations, their identification is crucial to avoid complications during surgeries involving renal veins or renal transplantation. In this case, the presence of two accessory renal veins originating from the upper and lower poles of the kidney adds complexity to the venous anatomy. Surgeons must be aware of such variations to ensure safe and effective procedures [9-10].
CONCLUSION
This case report highlights the importance of thorough anatomical knowledge and its implications in clinical settings, particularly in the context of renal vasculature variations. The presence of accessory renal arteries and veins, along with their branching patterns, necessitates meticulous preoperative assessment and intraoperative vigilance during renal surgeries and interventions. Surgeons and healthcare professionals involved in renal procedures should be well-versed in the normal anatomy and potential variations to ensure optimal patient outcomes.
Understanding anatomical variations in the renal vasculature not only enables safer surgical interventions but also contributes to the advancement of clinical anatomy. By documenting and sharing such cases, the existing body of knowledge can expand, ultimately benefiting patient care and surgical education. Additionally, further studies are warranted to explore the prevalence and clinical implications of anatomical variations in larger populations. Such research will promote a deeper understanding of renal vascular anatomy, enhance surgical planning, and reduce the risk of complications in renal disorders.
In conclusion, this case report highlights an unusual anatomical variation in the renal vasculature, underscoring the significance of anatomical knowledge in clinical practice. The presence of accessory renal arteries and veins, along with their branching patterns, should be thoroughly examined and considered during surgical planning to prevent inadvertent complications. Comprehensive understanding of anatomical variations contributes to improved surgical outcomes, patient safety, and the continued advancement of clinical anatomy.
ACKNOWLEDGEMENT
The authors would like to acknowledge the cadaveric donor and their family for their valuable contribution to medical education and research.
CONFLICT OF INTEREST
The authors declare no conflicts of interest related to this case report.
REFERENCES
- Krause DA, Youdas JW. Bilateral presence of a variant subscapularis muscle. Int J Anat Var. 2017; 10(4):79-80.
- Mann MR, Plutecki D, Janda P, Pękala J, Malinowski K, et al. The subscapularis muscle‐a meta‐analysis of its variations, prevalence, and anatomy. Clin Anat. 2023; 36(3):527-541.
- Pillay M, Jacob SM. Bilateral presence of axillary arch muscle passing through the posterior cord of the brachial plexus. Int. J. Morphol., 27(4):1047-1050, 2009.
- Pires LAS, Souza CFC, Teixeira AR, Leite TFO, Babinski MA, et al. Accessory subscapularis muscle–A forgotten variation?. Morphologie. 2017; 101(333):101-104.
- John C, Christian J. Commentary: Thoracic surgery residency: Not a spectator sport. J Thorac Cardiovasc Surg. 2020 Jun; 159(6):2345-2346.
- Anri S, Masayoshi O, Shigeru H. Glomerular Neovascularization in Nondiabetic Renal Allograft Is Associated with Calcineurin Inhibitor Toxicity. Nephron. 2020; 144 Suppl 1:37-42.
- Mamikonyan VR, Pivin EA, Krakhmaleva DA. Mechanisms of corneal neovascularization and modern options for its suppression. Vestn Oftalmo. 2016; 132(4):81-87.
- Gaigalaite V, Dementaviciene J, Vilimas A, Kalibatiene D. Association between the posterior part of the circle of Willis and vertebral artery hypoplasia. PLoS ONE. 2019; 14(9): e0213-226.
- Mujagic S, Kozic D, Huseinagic H, Smajlovic D. Symmetry, asymmetry and hypoplasia of intracranial internal carotid artery on magnetic resonance angiography. Acta Med Acad. 2016; 45:1- 9.
- Rusu MC, Vrapclu AD, Lazar M. A rare variant of accessory cerebral artery. Surg Radiol Anat. 2023; 45(5):523-526.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref