A Case Report on Inferior Alveolar Nerve
Received: 03-Nov-2022, Manuscript No. ijav-22-5056 ; Editor assigned: 06-Nov-2022, Pre QC No. ijav-22-5056 (PQ); Accepted Date: Jun 23, 2022; Reviewed: 20-Nov-2022 QC No. ijav-22-5056 ; Revised: 23-Nov-2022, Manuscript No. ijav-22-5056 (R); Published: 30-Nov-2022, DOI: 10.37532/1308-4038.15(11).226
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This case report presents an impacted third molar with associated dentigerous cyst in which the IAN is externalised and runs along the lateral surface of the mandible. This case reiterates the limitations of standard radiographic techniques such as the orthopantomogram.
Keywords
Inferior alveolar nerve; Impacted third molars; Cone beam computed tomography; Maxillofacial anatomy
Introduction
Third molar surgery remains one of the commonest procedures carried out by oral surgeons. One of the main concerns whilst performing this procedure is inferior alveolar nerve (IAN) damage [1]. We present a case of an unusual anatomical variation in which the inferior alveolar nerve was externalized. This case reiterates the need for appropriate pre-operative radiological assessment to identify the anatomic relationship of IAN with third molar teeth. In this occasion, an altered approach was required to preserve the IAN. This report is in line with the SCARE criteria.
CASE REPORT
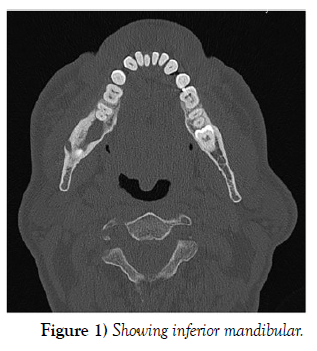
A medically fit 50-year-old male presented with a longstanding sinus in the right lower third molar region with intermittent pain, swelling and discharge. A standard orthopantomogram (OPG) showed the tooth to be horizontally impacted with an associated cystic lesion. Deviation and narrowing of the inferior alveolar canal was also noted on the OPG, suggesting a close approximation to the IAN. A computerized tomography (CT) scan was obtained to further assess the relationship and course of the nerve. This showed the nerve could be seen traversing laterally and superiorly in the buccal cortical bone within a corticated channel (Figure 1). Apart from the aforementioned cystic lesion, no other adverse features were reported by the consultant radiologist.
Discussion
There have been many human anatomical studies and, more recently, radiological studies that examine the course of the IAN [2]. In the majority of cases, the IAN is found inferior to the impacted third molar. Positional variation of the nerve in relation to the tooth tends to be in the buccolingual plane. Showed that 74% of IANs travel inferiorly and lingually to mandibular third molars [3]. A superior and buccal placement of the IAN, as in this case, is extremely rare. We believe this is the first report of an externalized IAN with clinical and radiological correlation. No information is currently present in the literature regarding the incidence of this variation. Some may argue that our finding is secondary to the cyst rather than a true anatomical variance. However, given that there was no bony expansion or change to the mandibular contour, we feel this variance is most likely to be anatomical, rather than pathological. The fact that there was intact cortical bone between cyst and nerve further supports our hypothesis. We appreciate that odontogenic cysts can displace the IAN canal. However, despite 18.1% of odontogenic cysts being dentigerous in nature, the externalization of the IAN has not been reported a finding with these lesions. Thus, in the balance of probabilities, we feel that externalization of nerve seen is this case is indeed due to an anatomical variation rather than a result of pathology [4-5].
Conclusion
Incidence of permanent IAN damage ranges from 0.35% to 8.4%. Although a rare complication, the implications of nerve damage can be significant for the patient. Timely and accurate pre-operative visualization of nerve is paramount in a safe clinical practice and reduces the risk of unnecessary litigations. Although the OPG has classically been used in the prediction of nerve proximity to lower third molars, it is limited in that it does not permit three-dimensional assessment of the inferior alveolar canal position. Cone beam CT has been proven to have better sensitivity and specificity in demonstrating nerve and tooth relationships. It allows the surgeon to plan the surgical approach to minimize risk and deliver a safe service. The CT, in this case, provided vital information regarding the proximity and externalization of the nerve, leading to the modification of surgical technique. Without this vital information, damage to the IAN could have been caused on reflecting the flap. The authors advise the use of Cone beam CT to assess third molars which have adverse features on plain film radiographs.
Acknowledgement
None.
Conflicts of Interest
None.
REFERENCES
- Maegawa H, Sano K, Kitagawa Y. Preoperative assessment of the relationship between the mandibular third molar and mandibular canal by axial computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 96(5):639-46.
- Jones AV. Craig GT. Franklin CD. Range and demographics of odontogenic cysts diagnosed in the UK over a 30 year period. J Oral Pathol Med. 35(8):500-700.
- Sarikov R, Juodzbalys G. Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. J Oral Maxillofac Res. 29; 5(4):e1.
- Rood JP, Shehab N. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 28(1):20-25.
- Tantanapornkul W, Kiyoshi O, Yoshikuni F, Masashi Y, et al. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 103(2):253-259.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref