A Case Report on Massive Hemoptysis, Cavitary Lesion Left Lower Lobe Lung with Aspergilloma of Post COVID 19Complication
Received: 18-Feb-2022, Manuscript No. PULJP-22-3933; Editor assigned: 21-Feb-2022, Pre QC No. PULJP-22-3933(PQ); Reviewed: 07-Mar-2022 QC No. PULJP-22-3933; Revised: 11-Mar-2022, Manuscript No. PULJP-22-3933(R); Published: 18-Mar-2022
Citation: Nikhil H. A case report on massive hemoptysis, cavitary lesion left lower lobe lung with aspergilloma of post COVID 19 complication. J Pulmonol. 2022;6(2):1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Pulmonary aspergilloma is a mass caused by a fungal infection. It usually grows in lung cavities. The infection can also appear in the brain, kidney, or other organs.
Case presentation: The authors present a case of a 60-year-old male with chief complaints of massive hemoptysis, several episodes over one day and shortness of breath. He had history of Diabetes Mellitus (DM) and Coronavirus disease of 19 (COVID-19).
Conclusion: This case emphasizes the importance of maintaining a high index of suspicion and In addition, this case tells us that aspergillosis is one of the new emerging infections in intensive care units.
Keywords
Pulmonary aspergillosis; Aspergilloma; COVID-19; Hemoptysis
Background
Pulmonary Aspergillosis refers to the clinical spectrum of lung diseases caused by several species of the genus Aspergillus. These fungal infections have recently shown increased incidence and are associated with significant morbidity and mortality [1]. In spite of the known clinical impact and improvement in diagnostics, Aspergillosis remains a diagnostic challenge in clinical practice. In this report, we present a case of pulmonary aspergillosis complicated by hemoptysis in a patient with history of immunodeficiency diseases like pulmonary Tuberculosis (TB), COVID-19.
Risk factors
Alveolar macrophages are the first line of defense against inhaled Aspergillus conidia. In the lungs, pathogen recognition receptors, such as Toll-like receptors, dectin-1 and mannose-binding Lectin, identify specific fungal wall components and produce cytokines that stimulate neutrophil recruitment, the main defense mechanism against Aspergillus hyphae [2]. The major risk factor for invasive pulmonary Aspergillosis (IPA) is immunodeficiency, which includes neutropenia, Hematopoietic Stem Cell Transplantation (HSCT) and solid-organ transplantation, prolonged therapy with high-dose corticosteroids, hematological malignancy, cytotoxic therapy, advanced Acquired Immuno-deficiency Syndrome (AIDS) and Chronic Granulomatous Disease (CGD) [3-5].
Case Presentation
A 60-year-old male was admitted with chief complaints of massive hemoptysis, several episodes over one day and shortness of breath. He had history of Diabetes mellitus in the last 30 years and was on oral hypoglycemics and COVID-19, 2 months back and was admitted in intensive care unit and underwent over high dose of corticosteroids for 10 days with oxygen support (Table 1).
| 1 | Patient (gender,age) | 60-year-old male |
| 2 | Final Diagnosis | Massive hemoptysis, cavitary lesion left lower lobe lung with aspergilloma of post covid 19 complication |
| 3 | Symptoms | massive hemoptysis, several episodes over one day and shortness of breath |
| 4 | Medications | with IV liposomal amphotericin-B of 300 mg for 7 days, IV antibiotics for 7 days, low molecular weight heparin, iron supplements, insulin and other supportive treatment |
| 5 | Clinical Procedure | Left lower lobectomy |
| 6 | Specialty | Cardiovascular and thoracic surgery |
Table 1: Summary of the case.
Investigations
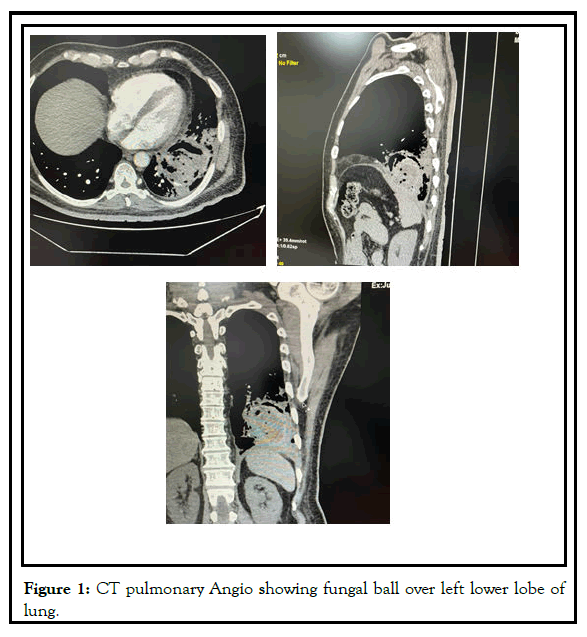
At the time of admission, he had low oxygen saturation of 89-91% with reduced airway entry on the left side. On required investigations, his CT pulmonary Angio it revealed destroyed left lower lobe of lung with very dense, vascularized adhesions between lower lobe and diaphragm and pericardium. Poorly developed major fissure with lingula also adherent to the lower lobe. Upper lobe appeared normal with normal aeration. A large 7.8 × 6.2 cm cavity in the lower lobe, a freely lying ball of tissue suggestive of fungal ball was found lying within the cavity and an eroded blood vessel with a clot was seen in the cavity. The patient had increased levels of Creactive protein of 28.83 mg/L, D-dimer of 1596 ng/ml, glycosylated hemoglobin of 12.1% and Prothrombin time of 13.6 sec He had low levels of Hemoglobin of 9.4 gm/dl. His other blood investigations like complete blood count, liver function tests, and kidney function tests, bleeding and clotting time were within the normal ranges. As patient underwent for left lung lower lobectomy, a specimen was sent for biopsy which was suggestive of bronchiectasis and the fungal ball specimen was sent for biopsy which revealed missed fungal infection, possibly of aspergilloma associated with zygomycosis (Figure 1).
Treatment
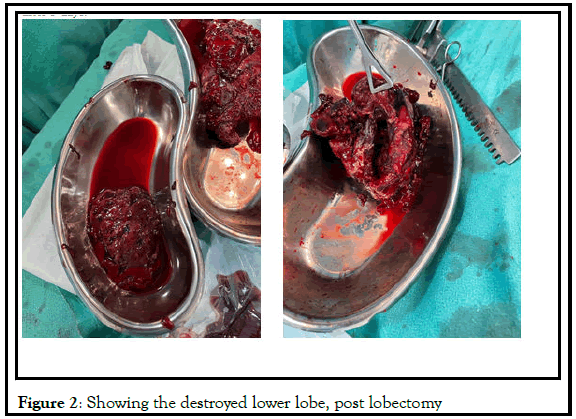
Patient underwent emergency lobectomy. Post-operative period was uneventful. He was treated with IV liposomal amphotericin-B of 300 mg for 7 days, IV antibiotics for 7 days, low molecular weight heparin, iron supplements, insulin and other supportive treatment. The drain was removed after 5 days (Figure 2).
Prognosis
At the time of discharge, he was stable, in sinus rhythm; wounds were healing well and advised to continue oral antibiotics and oral Posaconazole-300 mg once daily, for 1 month, regular breathing exercises, shoulder exercises and spirometry for 1 month.
Discussion
This case highlights the challenge of establishing a diagnosis of pulmonary aspergillosis. On admission, the main differential diagnoses were TB, aspergillosis and malignancy. CT showed the classic sign of a cavity colonized by Aspergillus. The final diagnosis and confirmation of the clinical form was only possible after appropriate histological samples were obtained through an invasive surgical procedure. This case illustrates that the diagnosis of aspergillosis must be suspected early on and prompt treatment initiated to prevent further complications.
Pulmonary aspergillosis presents with a variety of clinical forms including invasive pulmonary aspergillosis, chronic necrotizing aspergillosis (subacute invasive pulmonary aspergillosis), aspergilloma, Chronic Cavitary Pulmonary Aspergillosis (CCPA) and allergic bronchopulmonary aspergillosis [6]. Differential diagnosis among these forms is sometimes difficult due to overlapping presentations. The case presented here was a CCPA as defined elsewhere, [7] since the patient had only one pulmonary cavity, few symptoms and no radiological demonstration of progression.
Hemoptysis is one of the most devastating complications of pulmonary aspergillosis and is reported in 64%–83% of cases with aspergilloma [8].
In a recent report of 30 patients (40% with simple aspergillosis and 60% with chronic cavitary pulmonary aspergillosis), [9] recommended that surgery should be reserved for patients with unilateral localized disease, failure of medical treatment and to treat complications such as hemoptysis. Antifungal therapy is not excluded by surgical intervention in most cases since it can serve as an adjuvant treatment to prevent both Aspergillus empyema and recurrence of aspergillosis post-surgery [9]. In our case, the attempt to control bleeding with artery embolization yielded only partial results. Definitive treatment was successfully achieved only by surgical intervention.
Conclusion
Aspergillus is a mould which may lead to a variety of infectious, allergic diseases depending on the host’s immune status or pulmonary structure. Invasive pulmonary aspergillosis occurs primarily in patients with severe immunodeficiency. The significance of this infection has dramatically increased with growing numbers of patients with impaired immune state associated with the management of malignancy, organ transplantation, autoimmune and inflammatory conditions; critically ill patients and those with chronic obstructive pulmonary disease appear to be at an increased risk. The introduction of new noninvasive tests, combined with more effective and better-tolerated antifungal agents, has resulted in lower mortality rates associated with this infection.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Thompson GR III, Patterson TF. Pulmonary aspergillosis: recent advances. Semin Respir Crip Care Med 2011;32:673–681.
[cross refer] [Google scholar] [pubmed]
- Schaffner A, Douglas H, Braude A, et al. Selective protection against conidia by mononuclear and against mycelia by polymorphonuclear phagocytes in resistance to Aspergillus. Observations on these two lines of defense in vivo and in vitro with human and mouse phagocytes. J Clin Invest 1982;69:617–631.
[cross refer] [Google scholar] [pubmed]
- Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest 2002;121:1988–1999.
[cross refer] [Google scholar] [pubmed]
- Gerson SL, Talbot GH, Hurwitz S, et al. Prolonged granulocytopenia: the major risk factor for invasive pulmonary aspergillosis in patients with acute leukemia. Ann Intern Med 1984;100:345–351.
[cross refer] [Google scholar] [pubmed]
- Segal BH, Walsh TJ. Current approaches to diagnosis and treatment of invasive aspergillosis. Am J Respir Crit Care Med 2006; 173: 707–717.
[cross refer] [Google scholar] [pubmed]
- Walsh TJ, Anaissie EJ, Denning DW, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 2008;46:327–360.
[cross refer] [Google scholar] [pubmed]
- Smith NL, Denning DW. Underlying conditions in chronic pulmonary aspergillosis including simple aspergilloma. Eur Respir J 2011;37:865–872.
[cross refer] [Google scholar] [pubmed]
- Jewkes J, Kay PH, Paneth M, et al. Pulmonary aspergilloma: analysis of prognosis in relation to haemoptysis and survey of treatment. Thorax 1983;38:572–578.
[cross refer] [Google scholar] [pubmed]
- Farid S, Mohamed S, Devbhandari M, et al. Results of surgery for chronic pulmonary aspergillosis, optimal antifungal therapy and proposed high risk factors for recurrence a National Centre’s experience. J Cardiothorac Surg 2013;8:180.