A Case Report on Renal Vasculature Anomalies: A Rare Incidental Finding
Received: 04-Jul-2023, Manuscript No. ijav-23-6615; Editor assigned: 05-Jul-2023, Pre QC No. ijav-23-6615 (PQ); Accepted Date: Jul 24, 2023; Reviewed: 19-Jul-2023 QC No. ijav-23-6615; Revised: 24-Jul-2023, Manuscript No. ijav-23-6615 (R); Published: 31-Jul-2023, DOI: 10.37532/1308-4038.16(7).288
Citation: Hvizdosova N. A Case Report on Renal Vasculature Anomalies: A Rare Incidental Finding. Int J Anat Var. 2023;16(7):351-352.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Renal vasculature anomalies are uncommon clinical findings often discovered incidentally during routine imaging studies. This case report presents the incidental discovery of a rare renal vasculature anomaly in a 52-year-old female patient with no previous history of renal or vascular abnormalities. The patient underwent a comprehensive diagnostic workup, including contrastenhanced computed tomography (CT) and magnetic resonance angiography (MRA). The findings revealed an aberrant renal artery originating from the abdominal aorta with an unusual branching pattern. This case report highlights the importance of meticulous imaging evaluation and raises awareness among healthcare professionals regarding the identification and management of renal vasculature anomalies.
Keywords
Renal vasculature; Renal artery; Computed tomography; Magnetic resonance angiography; Vascular anomaly
INTRODUCTION
Renal vasculature anomalies are infrequently encountered clinical entities that can pose diagnostic challenges due to their rarity and diverse presentations. These anomalies may be congenital or acquired and can affect the renal arteries, veins, or both. Incidental detection of renal vasculature anomalies during radiological investigations has increased with the widespread use of advanced imaging modalities [1]. Early identification and appropriate management are crucial in preventing potential complications. This case report describes the identification and management of a rare renal vasculature anomaly discovered incidentally in an asymptomatic middle-aged female patient [2-3].
CASE REPORT
A 52-year-old female presented to the outpatient radiology department for a routine health check-up. The patient had no significant medical history, with no reported renal or vascular symptoms. Physical examination and routine laboratory investigations, including serum creatinine levels, were within normal limits. The patient’s blood pressure was also within the normal range (120/80 mmHg).
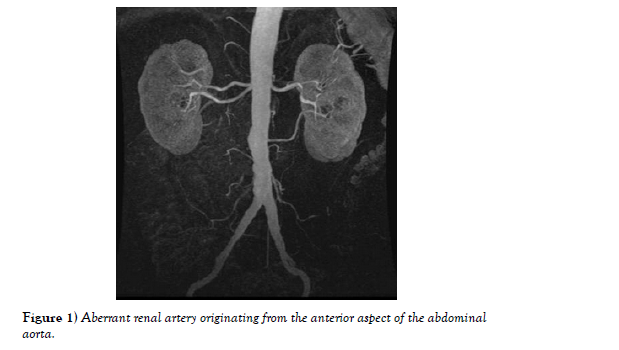
Imaging Studies: To further assess the patient’s renal vasculature a contrastenhanced abdominal computed tomography (CT) scan was performed the CT scan revealed an unexpected finding of an aberrant renal artery originating from the anterior aspect of the abdominal aorta, approximately 2 cm below the origin of the superior mesenteric artery (Figure 1).
The aberrant artery coursed posteriorly towards the right kidney, displaying a unique tortuous and elongated pathway. Subsequently, a magnetic resonance angiography (MRA) was performed to obtain more detailed information about the renal vasculature. The MRA confirmed the presence of the aberrant renal artery, which demonstrated an atypical branching pattern upon reaching the right kidney. The main trunk of the renal artery bifurcated into multiple smaller branches, providing an unusual appearance compared to the typical bifurcation observed in a normal renal artery.
Diagnosis and Management: Based on the imaging findings, a diagnosis of a rare renal vasculature anomaly was made. The patient’s renal function and blood pressure remained stable throughout the evaluation, indicating no immediate need for intervention or surgical correction.
FOLLOW-UP AND PROGNOSIS
The patient was scheduled for regular follow-up visits to monitor her renal function, blood pressure, and overall health. Asymptomatic cases of renal vasculature anomalies with preserved renal function and blood pressure often do not require immediate intervention. However, the patient was advised about potential complications that might arise in the future, such as hypertension or renal artery stenosis, which could necessitate further evaluation and management [4-5].
DISCUSSION
Renal vasculature anomalies are a diverse group of conditions that may be congenital or acquired. Congenital anomalies result from abnormal embryological development of the renal arteries or veins, while acquired anomalies can arise due to trauma, surgery, or other pathological processes affecting the renal vasculature. In this case, the anomaly appeared to be congenital, as the patient had no history of trauma or surgery that could explain the vascular aberration.
The most common renal vascular anomaly is a variation in the number of renal arteries or veins [6-7]. The presence of multiple renal arteries or veins can have significant implications for surgical procedures, kidney transplantation, or interventional radiology treatments. In contrast, the presence of a single renal artery or vein can increase the risk of vascular compromise in case of injury or disease.
However, the specific anomaly observed in this case report, i.e., an aberrant renal artery with an unusual branching pattern, is exceptionally rare. Such anomalies may be asymptomatic or present with clinical manifestations such as hypertension, renal impairment, or vascular complications.
The initial diagnostic imaging, including CT and MRA, played a vital role in identifying the renal vasculature anomaly and understanding its unique anatomical characteristics. Meticulous evaluation of imaging studies is crucial to detecting these anomalies, as they can be easily overlooked during routine radiological examinations. Early detection allows for appropriate management and monitoring to prevent potential complications and improve patient outcomes [8-10].
CONCLUSION
Renal vasculature anomalies are rare clinical entities that may have profound implications for patient management and outcomes. This case report presented an incidental discovery of a unique renal vasculature anomaly in a 52-year-old female patient with no prior history of renal or vascular issues. The anomaly involved an aberrant renal artery originating from the abdominal aorta, exhibiting an atypical branching pattern as it coursed towards the right kidney.
The successful identification of this rare anomaly was achieved through a comprehensive diagnostic workup, including contrast-enhanced computed tomography (CT) and magnetic resonance angiography (MRA). Such advanced imaging modalities play a pivotal role in detecting renal vasculature anomalies, given their intricate nature and potential to be overlooked during routine evaluations. Therefore, meticulous and detailed evaluation of imaging studies is vital for early detection and appropriate management.
While this patient’s anomaly was asymptomatic and did not require immediate intervention, it is crucial to acknowledge the potential risks associated with renal vasculature anomalies. Early diagnosis allows for timely intervention if required, preventing the development of complications such as hypertension, renal artery stenosis, or vascular compromise. For asymptomatic cases, regular follow-up is essential to monitor renal function, blood pressure, and overall health, ensuring timely intervention if clinical status changes.
The management of renal vasculature anomalies is individualized and depends on various factors, including the patient’s age, overall health, symptoms, and the anatomical characteristics of the anomaly. Asymptomatic cases with preserved renal function and blood pressure may not require immediate intervention but necessitate diligent monitoring. In contrast, symptomatic cases or those at risk of complications may require interventional radiology, endovascular procedures, or surgical correction.
Additionally, awareness of renal vasculature anomalies among healthcare professionals is crucial to promote early detection and appropriate management. Education and training regarding these rare entities should be emphasized in medical curricula and continuing medical education programs.
This case report also emphasizes the importance of interdisciplinary collaboration between radiologists, urologists, nephrologists, and vascular surgeons. Together, they can devise comprehensive management strategies for patients with renal vasculature anomalies, thereby ensuring optimal patient outcomes.
In conclusion, this case report underscores the significance of identifying and managing renal vasculature anomalies promptly. As advanced imaging technologies continue to improve, the chances of incidentally discovering such anomalies will likely increase. Therefore, healthcare professionals must remain vigilant during routine radiological evaluations and be prepared to address and manage these rare clinical findings effectively. With early detection and appropriate management, patients with renal vasculature anomalies can experience improved quality of life and reduced risk of potential complications in the long term. Further research and continued awareness of these rare anomalies are essential to enhance our understanding and optimize patient care in the field of renal medicine.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST
The author declares no conflicts of interest related to this case report.
REFERENCES
- Xin W, Bofu L. Aortic Dissection with Rare Anatomical Aortic Arch Variation Depicted by Computed Tomography Angiography. Heart Surg Forum. 2021; 24(2): E407-E408.
- Foivos I, Jonathon K, Daryll B. Aberrant right subclavian artery - a rare congenital anatomical variation causing dysphagia lusoria. Vasa. 2021; 504(5):394-397.
- Schizas N, Patris V, Lama N. Arc of Buhler: A lifesaving anatomic variation. A case report. J Vasc Bras. 2012; 37(11):9-326.
- Penprapa SK, Brianna KR. Duplication of the inferior vena cava: evidence of a novel type IV. Folia Med Cracov. 2020; 28; 60(2):5-13.
- Laurent de K, Stefano M. Variability of repairable bicuspid aortic valve phenotypes: towards an anatomical and repair-oriented classification. Eur J Cardiothorac Surg. 2019; 37(11):9-828.
- Jun S, Zhang-Y, Chuan C. Postoperative neovascularization, cerebral hemodynamics, and clinical prognosis between combined and indirect bypass revascularization procedures in hemorrhagic moyamoya disease. Clin Neurol Neurosurg. 2021 Sep; 208:106869.
- Qi L, Xiaojie T, Yafang D. Evaluation of Carotid Plaque Rupture and Neovascularization by Contrast-Enhanced Ultrasound Imaging: an Exploratory Study Based on Histopathology. Transl Stroke Res. 2021 Feb; 12(1):49-56.
- Kuo-Shyang J, Shu-Sheng L, Chiung-FC. The Role of Endoglin in Hepatocellular Carcinoma. Int J Mol Sci. 2021 Mar 22;22(6):3208.
- Anri S, Masayoshi O, Shigeru H. Glomerular Neovascularization in Nondiabetic Renal Allograft Is Associated with Calcineurin Inhibitor Toxicity. Nephron. 2020; 144 Suppl 1:37-42.
- Mamikonyan VR, Pivin EA, Krakhmaleva DA. Mechanisms of corneal neovascularization and modern options for its suppression. Vestn Oftalmo. 2016; 132(4):81-87.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at,, Google Scholar,, Crossref
Indexed at,, Google Scholar, Crossref