A case series of patients with early diastolic mitral regurgitation and left ventricular aneurysm
Received: 27-Aug-2021 Accepted Date: Sep 13, 2021; Published: 17-Sep-2021
Citation: Uema A, Sugiyama T, Yasu T. A case series of patients with early diastolic mitral regurgitation and left ventricular aneurysm. Clin Cardiol J. 2021;5(5):1-3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
This study presents patients with left ventricular aneurysm after anterior myocardial infarction showing early diastolic mitral regurgitation. This study was a case series (n=4) of patients with concurrent left ventricular aneurysm and early diastolic mitral regurgitation who died within six months following echocardiography. All the four patients showed low left ventricle ejection fraction values <33%, died of heart failure within six months following echocardiography. Incidentally, trans-mitral flow in all the four patients showed low-velocity E-waves with lower velocities (two showed no E-wave), as well as an end-diastolic A-wave with higher velocities than the E-wave. An impaired relaxation pattern was observed, despite the high pulmonary arterial wedge pressure >25 mm Hg and heart rate <90 bpm. These cases are first report of early-diastolic mitral regurgitation in left ventricular aneurysm with low left ventricle ejection fraction, which may be due to relatively high pressure in the left ventricle. In such cases the trans-mitral flow pattern in such cases could not predict pulmonary arterial wedge pressure.
Keywords
Diastolic mitral regurgitation; Left ventricular aneurysm; Myocardial infarction; Trans-mitral flow
Introduction
Left ventricular (LV) aneurysm is a critical mechanical complication of acute myocardial infarction (AMI) associated with low survival rate [1]. LV aneurysm also causes an increase in the LV end-diastolic pressure. We are the first to report concurrent early diastolic mitral regurgitation (MR) and LV aneurysm, following MI, to the best of our knowledge. Diastolic MR has a low velocity, owing to a relatively low diastolic LV–left atrial (LA) pressure gradient, resulting in occasionally difficult detection [2,3]. The present study aimed to present a case series report of patients with LV aneurysm showing early diastolic MR.
Method
Study design and subjects
This study was a retrospective case series report of four patients diagnosed with LV aneurysm after anterior AMI, who also presented with early diastolic MR on echocardiography, between April 2012 and December 2017, in our institution. This study had a single-center case series study design. All subjects underwent echocardiography and cardiac catheterization.
Ethics approval
This study was conducted in accordance with the principles outlined in the Declaration of Helsinki and the ethics guidelines for clinical research from the Ministry of Health, Labor and Welfare (Tokyo, Japan). Informed consent in the form of opt-out was obtained from patients at our institute, and patients who refused to provide informed consent were excluded. The study protocol was reviewed and approved by the institutional ethics committee of Dokkyo Medical University Nikko Medical Center (Approval number: Nikko 29006).
Results
Case 1
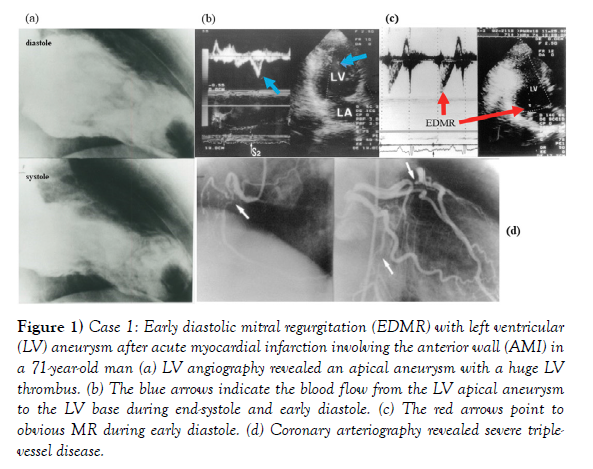
A 71-year-old man with a previous history of AMI involving the anterior wall and apical aneurysm with an LVEF of 32% and an LV thrombus (Figure 1a) exhibited early diastolic blood flow from the apex to the LV base (Figure 1b), as well as obvious early diastolic MR (Figure 1c). Coronary arteriography revealed severe stenosis in the proximal left anterior descending (LAD) artery, circumflex artery, and proximal right coronary artery (Figure 1d). The patient underwent urgent coronary artery bypass surgery (internal thoracic artery to the LAD artery, right internal thoracic artery to the right coronary artery, and saphenous vein to the left circumflex artery), LV thrombectomy, and resection of aneurysm. The intraoperative observation indicated no pathological findings involving the mitral valve, papillary muscle, or chordae. The patient died of heart failure and acute renal failure at postoperative day 3.
Figure 1: Case 1: Early diastolic mitral regurgitation (EDMR) with left ventricular (LV) aneurysm after acute myocardial infarction involving the anterior wall (AMI) in a 71-year-old man (a) LV angiography revealed an apical aneurysm with a huge LV thrombus. (b) The blue arrows indicate the blood flow from the LV apical aneurysm to the LV base during end-systole and early diastole. (c) The red arrows point to obvious MR during early diastole. (d) Coronary arteriography revealed severe triplevessel disease.
Case 2
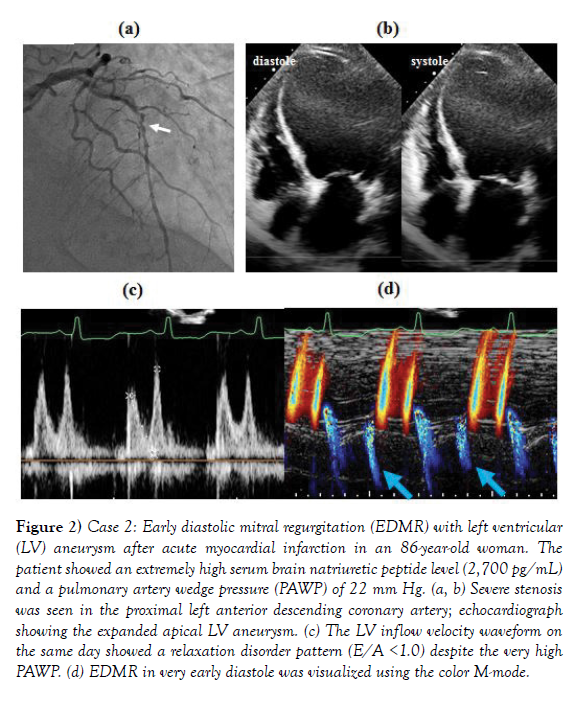
An 86-year-old woman was hospitalized for heart failure. Coronary arteriography revealed severe stenosis in the proximal LAD artery (Figure 2a). Echocardiography indicated an LVEF of 21% with an apical aneurysm (Figure 2b). In this patient, the serum Brain Natriuretic Peptide (BNP) level was 2700 pg/mL, and the Pulmonary Artery Wedge Pressure (PAWP) had increased to 22 mm Hg upon Swan-Ganz catheterization. Nonetheless, echocardiography revealed a relaxation disorder pattern in the LV inflow velocity waveform (Figure 2c), and early diastolic MR was observed (Figure 2d). Despite the provision of positive-pressure ventilation and administration of diuretics and catecholamines, the patient died of heart failure on the 48th hospital day.
Figure 2: Case 2: Early diastolic mitral regurgitation (EDMR) with left ventricular (LV) aneurysm after acute myocardial infarction in an 86-year-old woman. The patient showed an extremely high serum brain natriuretic peptide level (2,700 pg/mL) and a pulmonary artery wedge pressure (PAWP) of 22 mm Hg. (a, b) Severe stenosis was seen in the proximal left anterior descending coronary artery; echocardiograph showing the expanded apical LV aneurysm. (c) The LV inflow velocity waveform on the same day showed a relaxation disorder pattern (E/A <1.0) despite the very high PAWP. (d) EDMR in very early diastole was visualized using the color M-mode.
Case 3
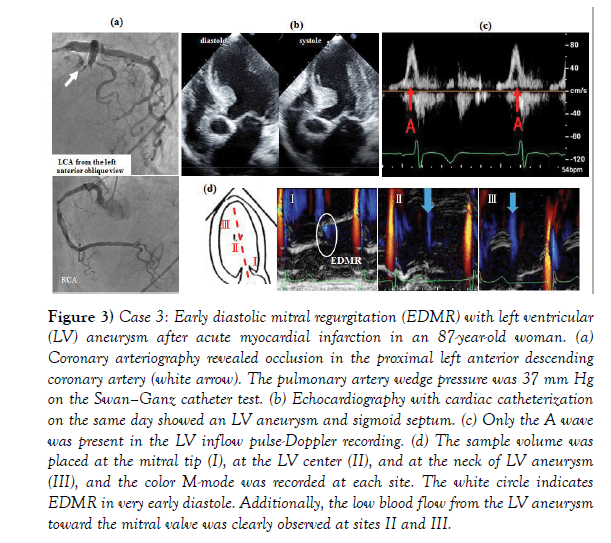
An 87-year-old woman was hospitalized for heart failure due to AMI involving the anterior wall two days following the index cardiac event. Coronary arteriography revealed occlusion in the proximal LAD artery and 75% stenosis in the proximal right artery (Figure 3a). Percutaneous coronary intervention (PCI) with deployment of a drug-eluting stent was performed for the proximal LAD artery lesion. Echocardiography showed wall dyskinesia from the mid-anterior wall to the apex, which was also affected by wall thinning. The LVEF was 23% (Figure 3b). This patient had a high serum BNP level (403 pg/mL), and the PAWP increased to 37 mm Hg upon Swan-Ganz catheterization. However, echocardiography indicated that the E wave of the LV inflow velocity could not be visualized (Figure 3c). Furthermore, the color M-mode method revealed early diastolic MR (Figures 3d-I), and slow blood flow from the LV aneurysm toward the mitral valve was observed (Figure 3d-II, III). The patient died of heart failure three months following her discharge.
Figure 3: Case 3: Early diastolic mitral regurgitation (EDMR) with left ventricular (LV) aneurysm after acute myocardial infarction in an 87-year-old woman. (a) Coronary arteriography revealed occlusion in the proximal left anterior descending coronary artery (white arrow). The pulmonary artery wedge pressure was 37 mm Hg on the Swan-Ganz catheter test. (b) Echocardiography with cardiac catheterization on the same day showed an LV aneurysm and sigmoid septum. (c) Only the A wave was present in the LV inflow pulse-Doppler recording. (d) The sample volume was placed at the mitral tip (I), at the LV center (II), and at the neck of LV aneurysm (III), and the color M-mode was recorded at each site. The white circle indicates EDMR in very early diastole. Additionally, the low blood flow from the LV aneurysm toward the mitral valve was clearly observed at sites II and III.
Case 4
A 78-year-old man was hospitalized for AMI affecting the anterior wall, 6 h following the index cardiac event. Electrocardiography showed abnormal Q-waves in leads V1-V3, whereas echocardiography indicated LV aneurysm with an LVEF of 30% (Figure 4a). Coronary arteriography revealed 99% stenosis in the proximal LAD artery (Figures 4b). PCI, with mechanical support by intraortic balloon pumping, was performed for the proximal LAD artery lesion and involved the deployment of a drug-eluting stent. This patient had an extremely high serum BNP level of 3340 pg/mL and PAWP of 30 mmHg. Nevertheless, echocardiography revealed a relaxation disorder pattern (Figures 4c) and slight early diastolic MR (Figures 4d).
Figure 4: Case 4: (a) Early diastolic mitral regurgitation (EDMR) with left ventricular (LV) aneurysm after acute myocardial infarction in a 78-year-old male patient. (b) Coronary arteriography revealed severe stenosis in the proximal left anterior descending artery (white arrow). The patient showed a brain natriuretic peptide level of 3340 pg/mL and pulmonary artery wedge pressure of 30 mm Hg. (c) Echocardiography indicated an E/A of 0.89 in the LV inflow velocity waveform and (d) slight EDMR.
All the four patients with concurrent LV aneurysm and early diastolic MR, who showed low LVEF values <33%, died of heart failure within six months following echocardiography (Table 1). Incidentally, the trans-mitral flow (TMF) in all the four patients showed an E-wave with lower velocities (two showed no E-wave), as well as an end-diastolic A-wave with higher velocities than the E-wave, together with an impaired relaxation pattern, despite the high PAWP >25 mm Hg and heart rate <90/m (Table 1).
| Variables | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Age (years) | 71 | 86 | 87 | 78 |
| Sex | M | F | F | M |
| Coronary artery lesion | LAD#6 99%, | LAD#7 90% | LAD#7 100% | LAD#6 100% |
| RCA#2 99%, LCX#1390% | RCA#1 75% | |||
| Treatment | CABG | Medication | PCI | PCI |
| LVEF (%) | 32 | 21 | 23 | 30 |
| E/A | E wave not detected | 0.7 | Â E wave not detected | 0.9 |
| BNP (pg/ml) | 2,901 | 2,794 | 403 | 3,342 |
| PAWP (mm Hg) | 29 | 27 | 37 | 30 |
| MACE | Death from HF | Death from HF on the 48th  hospital day | Death from HF | Death from HF |
| 3 days after CABG surgery | 48 days after admission | Â after 3 months | 1 week after PCI | |
| BNP: Brain Natriuretic Peptide, CABG: Coronary Artery Bypass Grafting, LAD: Left Anterior Descending Coronary Artery, LCX: Left Circumflex Coronary Artery, LVEF: Left Ventricular Ejection Fraction, PCI: Percutaneous Coronary Intervention, PAWP: Pulmonary Artery Wedge Pressure, RCA: Right Coronary Artery, MACE: Major Adverse Cardiac Events, cardiovascular death, non-fatal myocardial infarction, stroke, and heart failure or unstable angina requiring hospitalization. |
||||
TABLE 1.Four cases of anterior myocardial infarction with left ventricular aneurysm and early diastolic mitral regurgitation.
BNP: Brain Natriuretic Peptide,
CABG: Coronary Artery Bypass Grafting,
LAD: Left Anterior Descending Coronary Artery,
LCX: Left Circumflex Coronary Artery,
LVEF: Left Ventricular Ejection Fraction,
PCI: Percutaneous Coronary Intervention,
PAWP: Pulmonary Artery Wedge Pressure,
RCA: Right Coronary Artery,
MACE: Major Adverse Cardiac Events, cardiovascular death, non-fatal myocardial infarction, stroke, and heart failure or unstable angina
requiring hospitalization.
Discussion
We reported four patients with LV aneurysm accompanied by early diastolic MR, who subsequently died due to congestive heart failure within six months. Mechanism for early diastolic MR accompanied with LV aneurysm has not been explored; however, this may result in loss of suction from the LV apical aneurysm causing a reversal of the left atrioventricular pressure gradient in early diastole [4]. Mid-late diastolic MR in patients with severe aortic regurgitation and atrioventricular block has been reported [5-9]. Midlate diastolic MR associated with AR results from considerable elevation of the LV end-diastolic pressure due to excessive blood flow from the aorta into the LV [2,5-7].
We believe that our case series study makes a significant contribution to the literature because our results indicated that estimating LV end-diastolic pressure by mitral inflow pattern [10-12] may be difficult in particular cases with LV aneurysm, especially if associated with early diastolic MR. A possible explanation for the impaired relaxation pattern (E/A <1) of TMF, despite the high PAWP in patients with LV aneurysm, may be the relatively high early diastolic LV pressure, particularly in an aneurysm. Shen et al. [1] reported that out of 71 patients with anterior AMI, 10 with aneurysm and 3 without aneurysm died within a mean follow-up duration of 53 months. Their stepwise multivariate analysis revealed that LVEF and the obstructive status of the LAD artery and collaterals were independent predictors of mortality in patients with aneurysms. Furthermore, they concluded that the reduced survival rate in patients with an aneurysm was primarily related to severe global LV dysfunction, which may be determined via assessing the residual flow to the infarct region. Of note, all four of our patients showed severe global LV dysfunction (LVEF<33%). Our study had some limitations. The number of study patients was limited. Moreover, we did not simultaneously measure the LV pressure and PAWP upon cardiac catheterization.
Conclusion
In conclusion, early diastolic MR in LV aneurysm may be attributable to relatively high pressure in the LV during the early diastolic phase. Estimating LV end-diastolic pressure by mitral inflow pattern may be difficult in particular cases with LV aneurysm, especially associated with early diastolic MR.
Acknowledgements
This work was supported by a grant from the Vehicle Racing Commemorative Foundation (to T.Y.) and by Dokkyo Medical University, Young Investigator Award (No. 2017–21) (to A.U.). Part of this paper was presented at the annual meeting of the American Heart Association in Philadelphia in November 2019. We would like to thank Editage (www.editage.com) for English language editing.
Conflict of Interest
Dr. Yasu has received grant support from Abbott Medical Japan LLC., AstraZeneca K.K., Ono Pharmaceutical Co., Ltd., Kowa Co. Ltd., and MTG Co. Ltd. The other authors have no conflicts of interest to declare.
REFERENCES
- Shen WF, Tribouilloy C, Mirode A, Dufosse H, Lesbre JP. Left ventricular aneurysm and prognosis in patients with first acute transmural anterior myocardial infarction and isolated left anterior descending artery disease. Eur Heart J 1992;13(1):39-4.
- Agmon Y, Freeman WK, Oh JK, et al. Diastolic mitral regurgitation. Circulation 1999;99:13.
- Alessandri N, Mariani S, Messina FR, et al. Diastolic mitral regurgitation: A borderline case in cardiovascular physiology. Eur Rev Med Pharmacol Sci 2003;7:161–70.
- Murayama M, Iwano H, Sarashina M, et al. Mechanism of early-diastolic mitral regurgitation. Circ J 2020;84:20-36.
- Konka M, Kusmierczyk-Droszcz B, Wozniak O, et al. Aortic regurgitation and unusual diastolic mitral regurgitation. Eur J Echocardiogr 2008;9:709–11.
- Schnittger Ⅰ, Appleton CP, Hatle LK, et al. Diastolic mitral and tricuspid regurgitation by Doppler echocardiography in patients with atrioventricular valve closure. J Am Coll Cardiol 1988;11:83–8.
- Berger RL, Katz E, Tunick P, et al. The ‘A-dip’ of diastolic mitral regurgitation: an unusual Doppler flow pattern in a patient with severe aortic insufficiency and complete heart block. Eur J Echocardiogr 2008;9:69–71.
- Sisu RC, Vinereanu D. Different mechanisms for diastolic mitral regurgitation illustrated by three comparative cases. Echocardiography 2011;28:476–9.
- Agrawal A, Parikh M, Verma I, et al. Diastolic mitral regurgitation in a patient with coronary artery disease and anaemia. BMJ Case Rep 2016;2:2016214473.
- Nagueh SF, Bhatt R, Vivo RP, et al. Echocardiographic evaluation of hemodynamics in patients with decompensated systolic heart failure. Circ Cardiovasc Imaging 2011;4:220–7.
- Dokainish H, Nguyen JS, Bobek J, et al. Assessment of the American Society of Echocardiography-European Association of Echocardiography guidelines for diastolic function in patients with depressed ejection fraction: an echocardiographic and invasive haemodynamic study. Eur J Echocardiogr 2011;12:857–64.
- Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2016;17:1321–60.