A new foramen on posterior aspect of ala of first sacral vertebra*
Rajani Singh*
Department of Anatomy, CSM Medical University, Lucknow, UP, India.
- *Corresponding Author:
- Rajani Singh
Department of Anatomy,CSM Medical University Lucknow, UP, India
Tel: +91 (945) 3193659
E-mail: nani_sahayal@rediffmail.com
Date of Received: August 12th, 2011
Date of Accepted: May 30th, 2012
Published Online: August 11th, 2012
© Int J Anat Var (IJAV). 2012; 5: 29–31.
[ft_below_content] =>Keywords
ala,artery,foramen,sacrum,transverse process
Introduction
The sacrum is a large triangular bone formed by fusion of five sacral vertebrae [1]. Anatomy of sacral vertebra is complex [2]. Technically, the placement of pedicle screw into S1 vertebra is a difficult surgical procedure. Therefore it is important to know the anatomy of S1 vertebra [3].
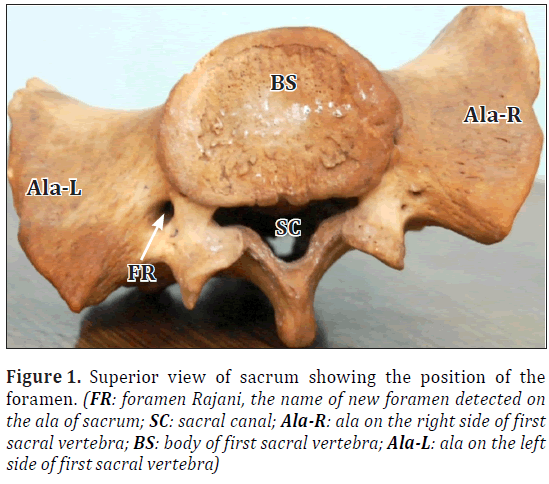
First sacral vertebra possesses the features of typical vertebra in modified form. Thus it consists of body, vertebral foramen, articular process and ala. Ala of sacrum is formed by fusion of costal elements and transverse process. Anterior 3/4 of ala of sacrum is formed by costal elements and posterior 1/4 is formed by transverse process. A new foramen (Figure 1) was detected on posterior aspect of ala of sacrum on left side. Detection of foramen on posterior aspect of ala of sacrum may change the prevailing concept of anatomy in this region.
Figure 1: Superior view of sacrum showing the position of the foramen. (FR: foramen Rajani, the name of new foramen detected on the ala of sacrum; SC: sacral canal; Ala-R: ala on the right side of first sacral vertebra; BS: body of first sacral vertebra; Ala-L: ala on the left side of first sacral vertebra)
Foramen on the first sacral vertebra has been described to be absent. No literature in the contemporary research has been found in relation to any foramen in this region except that in Cunningham’s Textbook of Anatomy [4] record the occurrence of a foramen in the lateral part of first sacral vertebra which is completely different from new foramen on posterior aspect of first sacral vertebra.
The pedicle screw fixation/instrumentation may damage the structure passing through this foramen resulting in neurovascular injury if the orthopaedic surgeon is unaware of this foramen. Therefore to alert orthopaedic surgeons, neurosurgeons, and to document its location, dimensions, modification in structural pattern and clinical implication the study has been carried out.
Case Report
A new foramen on posterior part of ala of sacrum was found during routine osteology class of MBBS students in the Department of Anatomy, CSM Medical University Lucknow, UP, India. The incidence of this foramen revolutionised the prevailing anatomical concept against the viewpoint of absence of foramen and configuration of structures in this region.
Its position was 20 mm from posterior tip of ala of sacrum, 8 mm from sacral canal and 5 mm from posterior border of body of first sacral vertebra, as measured by vernier caliper. It was oval shaped, having 6 mm horizontal and 4 mm vertical dimension. It was communicating with the first sacral foramen and sacral canal (Figure 1).
Discussion
The viewpoint of no foramen on the transverse process of thoracic, lumber and sacral vertebrae, changed due to recording of presence of a foramen on the transverse process of fifth lumber vertebra [5] and a foramen on the lateral part of first sacral vertebra [4]. The finding of new foramen on the posterior aspect of ala of first sacral vertebra has further modified the above viewpoint.
To provide separate identity to the foramen under study for addressing it in the development of anatomical theory and clinical significance, we named as “Foramen Rajani”.
Probable causes of formation of the foramen
The structures iliolumbar or common iliac vessels or lumbosacral trunk or sympathetic chain might have taken an aberrant course and created the foramen in embryonic period which may be genetically determined. This may also be generated by chemicals or environmental effect in utero. It may be associated with other congenital defects to be confirmed by further studies.
Keeping in mind the position of the foramen, most probable structure passing through the foramen may be lumbosacral trunk. Other structures which may take an aberrant course during embryonic period to create this foramen, in order of preference, may be recorded as common iliac vein, common iliac artery, lumbar branch of iliolumbar artery and sympathetic chain.
The clinical significance of the foramen
1. During sacral instrumentation, lumbosacral trunk may be injured leading to weakness of muscles supplied by this nerve. Common peroneal (L4, 5, S 1, 2) may be affected leading to weakness of short head of biceps femoris. Its cutaneous branches –(1) lateral cutaneous nerve of calf, (2) sural communicating nerve– may lead to sensory loss to varying degree in the areas supplied by these nerves. Due to tibial nerve (L4, 5 S1, 2, 3), flexor muscles supplied by this nerve may be affected leading to difficulty in walking. There may be sensory loss in the area supplied by cutaneous branches of tibial nerve i.e., sural nerve. Due to involvement of superior gluteal nerve (L4, 5, S1), there may be paralysis of gluteus medius and minimus. Inferior gluteal nerve (L 5, S 1, 2) may also be affected leading to paralysis of gluteal maximus. Due to involvement of nerve to quadratus femoris (L 4, 5, S1) and nerve to obturator internus, there may be weakness of quadratus femoris and obturator internus (L 5, S 1, 2), respectively.
2. During increased venous return, vein passing through the foramen may be compressed within bony confines of foramen leading to engorgement of veins and swelling of lower limb of affected side.
3. During instrumentation and pedicle screw fixation common iliac artery or lumbar branch or common iliac vein passing through the foramen may be injured leading to intra-operative hemorrhage.
4. Due to injury of sympathetic chain (Figure 2) there may be weakness of internal sphincter of urinary bladder, vasodilatation and loss of sweating.
Apart from this foramen Rajani assumes importance on the basis of its imaging only by CT or MRI and not by X-Rays. Hence clinically, verification of existence of this foramen is of paramount importance to surgeons to avoid intra-operative and postoperative complications during surgery involving first sacral vertebra.
Conclusion
The location of the new foramen from the surrounding landmarks provides vital information to surgeons for undergoing surgical procedures involving first sacral vertebra. Out of the five structures which might pass through the foramen, most probable structure passing through it is lumbosacral trunk as it is in the closest proximity of this foramen and least likely is sympathetic trunk.
It is recommended that study may further be extended with inclusion of data of surgical failures to confirm the model. CT and MRI are strongly recommended before pedicle screw fixation or instrumentation involving first sacral vertebra to prevent damage to structures passing through the foramen, thereby preventing intra-operative and post-operative complications.
Acknowledgement
The author very gratefully, acknowledges her father, Mr. Man Singh M.Sc. (Electronics), Ex. Sr. Scientist of ONGC India for inspiring her for this research. His unforgettable contribution through discussion gave the shape to this paper without which this piece of work has not been possible. Last but not the least author is grateful to the HOD and staff of the Department of Anatomy CSM Medical University.FRSCAla-RBSAla-L
References
- Standring S, ed. Gray’s Anatomy. 39th Ed., London, Churchill Livingstone. 2005; 749.
- Xu R, Ebraheim NA, Gove NK. Surgical anatomy of the sacrum. Am J Orthop (Belle Mead NJ). 2008; 37: E177–E181.
- Basaloglu H, Turgut M, Taser FA, Ceylan T, Basaloglu HK, Ceylan AA. Morphometry of the sacrum for clinical use. Surg Radiol Anat. 2005; 27: 467-471.
- Smith EB. Two rare vertebral anomalies. J Anat Physiol. 1902; 36: 372–374.
- Szalowski J. Ueber einige seltene Variationen an der Wirbelsäule beim Menschen. Anat Anz. 1901; 20: 305–320.
Rajani Singh*
Department of Anatomy, CSM Medical University, Lucknow, UP, India.
- *Corresponding Author:
- Rajani Singh
Department of Anatomy,CSM Medical University Lucknow, UP, India
Tel: +91 (945) 3193659
E-mail: nani_sahayal@rediffmail.com
Date of Received: August 12th, 2011
Date of Accepted: May 30th, 2012
Published Online: August 11th, 2012
© Int J Anat Var (IJAV). 2012; 5: 29–31.
Abstract
A new foramen on posterior part of ala of sacrum was found during routine osteology class of MBBS students in the Department of Anatomy, CSM Medical University Lucknow, UP, India. As no literature was available on this virgin foramen, therefore, study has been carried out. Foramen was located at 8 mm from sacral canal, 20 mm from posterior tip of ala of sacrum and 5 mm from posterior border of body of first sacral vertebra. It was oval in shape, having its horizontal and vertical dimensions as 6 mm and 4 mm, respectively. It communicated with the first sacral foramina and sacral canal. One of the structures, common iliac vessels, lumbar branch of iliolumbar artery, lumbosacral trunk and sympathetic chain is likely to pass through the “foramen Rajani”. The structure confined in this foramen may be damaged during pedicle screw fixation or instrumentation. Thus, knowledge of this foramen is of paramount importance to orthopaedic surgeon, neurosurgeons and anatomists.
-Keywords
ala,artery,foramen,sacrum,transverse process
Introduction
The sacrum is a large triangular bone formed by fusion of five sacral vertebrae [1]. Anatomy of sacral vertebra is complex [2]. Technically, the placement of pedicle screw into S1 vertebra is a difficult surgical procedure. Therefore it is important to know the anatomy of S1 vertebra [3].
First sacral vertebra possesses the features of typical vertebra in modified form. Thus it consists of body, vertebral foramen, articular process and ala. Ala of sacrum is formed by fusion of costal elements and transverse process. Anterior 3/4 of ala of sacrum is formed by costal elements and posterior 1/4 is formed by transverse process. A new foramen (Figure 1) was detected on posterior aspect of ala of sacrum on left side. Detection of foramen on posterior aspect of ala of sacrum may change the prevailing concept of anatomy in this region.
Figure 1: Superior view of sacrum showing the position of the foramen. (FR: foramen Rajani, the name of new foramen detected on the ala of sacrum; SC: sacral canal; Ala-R: ala on the right side of first sacral vertebra; BS: body of first sacral vertebra; Ala-L: ala on the left side of first sacral vertebra)
Foramen on the first sacral vertebra has been described to be absent. No literature in the contemporary research has been found in relation to any foramen in this region except that in Cunningham’s Textbook of Anatomy [4] record the occurrence of a foramen in the lateral part of first sacral vertebra which is completely different from new foramen on posterior aspect of first sacral vertebra.
The pedicle screw fixation/instrumentation may damage the structure passing through this foramen resulting in neurovascular injury if the orthopaedic surgeon is unaware of this foramen. Therefore to alert orthopaedic surgeons, neurosurgeons, and to document its location, dimensions, modification in structural pattern and clinical implication the study has been carried out.
Case Report
A new foramen on posterior part of ala of sacrum was found during routine osteology class of MBBS students in the Department of Anatomy, CSM Medical University Lucknow, UP, India. The incidence of this foramen revolutionised the prevailing anatomical concept against the viewpoint of absence of foramen and configuration of structures in this region.
Its position was 20 mm from posterior tip of ala of sacrum, 8 mm from sacral canal and 5 mm from posterior border of body of first sacral vertebra, as measured by vernier caliper. It was oval shaped, having 6 mm horizontal and 4 mm vertical dimension. It was communicating with the first sacral foramen and sacral canal (Figure 1).
Discussion
The viewpoint of no foramen on the transverse process of thoracic, lumber and sacral vertebrae, changed due to recording of presence of a foramen on the transverse process of fifth lumber vertebra [5] and a foramen on the lateral part of first sacral vertebra [4]. The finding of new foramen on the posterior aspect of ala of first sacral vertebra has further modified the above viewpoint.
To provide separate identity to the foramen under study for addressing it in the development of anatomical theory and clinical significance, we named as “Foramen Rajani”.
Probable causes of formation of the foramen
The structures iliolumbar or common iliac vessels or lumbosacral trunk or sympathetic chain might have taken an aberrant course and created the foramen in embryonic period which may be genetically determined. This may also be generated by chemicals or environmental effect in utero. It may be associated with other congenital defects to be confirmed by further studies.
Keeping in mind the position of the foramen, most probable structure passing through the foramen may be lumbosacral trunk. Other structures which may take an aberrant course during embryonic period to create this foramen, in order of preference, may be recorded as common iliac vein, common iliac artery, lumbar branch of iliolumbar artery and sympathetic chain.
The clinical significance of the foramen
1. During sacral instrumentation, lumbosacral trunk may be injured leading to weakness of muscles supplied by this nerve. Common peroneal (L4, 5, S 1, 2) may be affected leading to weakness of short head of biceps femoris. Its cutaneous branches –(1) lateral cutaneous nerve of calf, (2) sural communicating nerve– may lead to sensory loss to varying degree in the areas supplied by these nerves. Due to tibial nerve (L4, 5 S1, 2, 3), flexor muscles supplied by this nerve may be affected leading to difficulty in walking. There may be sensory loss in the area supplied by cutaneous branches of tibial nerve i.e., sural nerve. Due to involvement of superior gluteal nerve (L4, 5, S1), there may be paralysis of gluteus medius and minimus. Inferior gluteal nerve (L 5, S 1, 2) may also be affected leading to paralysis of gluteal maximus. Due to involvement of nerve to quadratus femoris (L 4, 5, S1) and nerve to obturator internus, there may be weakness of quadratus femoris and obturator internus (L 5, S 1, 2), respectively.
2. During increased venous return, vein passing through the foramen may be compressed within bony confines of foramen leading to engorgement of veins and swelling of lower limb of affected side.
3. During instrumentation and pedicle screw fixation common iliac artery or lumbar branch or common iliac vein passing through the foramen may be injured leading to intra-operative hemorrhage.
4. Due to injury of sympathetic chain (Figure 2) there may be weakness of internal sphincter of urinary bladder, vasodilatation and loss of sweating.
Apart from this foramen Rajani assumes importance on the basis of its imaging only by CT or MRI and not by X-Rays. Hence clinically, verification of existence of this foramen is of paramount importance to surgeons to avoid intra-operative and postoperative complications during surgery involving first sacral vertebra.
Conclusion
The location of the new foramen from the surrounding landmarks provides vital information to surgeons for undergoing surgical procedures involving first sacral vertebra. Out of the five structures which might pass through the foramen, most probable structure passing through it is lumbosacral trunk as it is in the closest proximity of this foramen and least likely is sympathetic trunk.
It is recommended that study may further be extended with inclusion of data of surgical failures to confirm the model. CT and MRI are strongly recommended before pedicle screw fixation or instrumentation involving first sacral vertebra to prevent damage to structures passing through the foramen, thereby preventing intra-operative and post-operative complications.
Acknowledgement
The author very gratefully, acknowledges her father, Mr. Man Singh M.Sc. (Electronics), Ex. Sr. Scientist of ONGC India for inspiring her for this research. His unforgettable contribution through discussion gave the shape to this paper without which this piece of work has not been possible. Last but not the least author is grateful to the HOD and staff of the Department of Anatomy CSM Medical University.FRSCAla-RBSAla-L
References
- Standring S, ed. Gray’s Anatomy. 39th Ed., London, Churchill Livingstone. 2005; 749.
- Xu R, Ebraheim NA, Gove NK. Surgical anatomy of the sacrum. Am J Orthop (Belle Mead NJ). 2008; 37: E177–E181.
- Basaloglu H, Turgut M, Taser FA, Ceylan T, Basaloglu HK, Ceylan AA. Morphometry of the sacrum for clinical use. Surg Radiol Anat. 2005; 27: 467-471.
- Smith EB. Two rare vertebral anomalies. J Anat Physiol. 1902; 36: 372–374.
- Szalowski J. Ueber einige seltene Variationen an der Wirbelsäule beim Menschen. Anat Anz. 1901; 20: 305–320.