A rare case of looping of supraclavicular nerve branches around external jugular vein and transverse cervical artery
T. Ramesh Rao1*, Prakashchandra Shetty2 and Suresh Rao3
1Department of Paraclinical Sciences, Faculty of Medical Sciences, The University of The West Indies, St. Augustine, Trinidad, West Indies
2Department of Anatomy, Kasturba Medical College, Manipal – 576104, Udupi, Karnataka, India
3Department of Preclinical Sciences, Faculty of Medical Sciences, The University of The West Indies, St. Augustine, Trinidad, West Indies
- *Corresponding Author:
- T. Ramesh Rao, MSc, PhD
Faculty of Medical Sciences, Department of Paraclinical Sciences, Faculty of Medical Sciences, The University of The West Indies, St. Augustine, Trinidad, West Indies
Tel: +1 (868) 662-1472, ext. 5001
Fax: +1 (868) 662-1472
E-mail: varun1195@yahoo.com
Date of Received: November 5th, 2008
Date of Accepted: May 6th, 2009
Published Online: May 11th, 2009
© IJAV. 2009; 2: 48–50.
[ft_below_content] =>Keywords
supraclavicular nerve, entrapment, lesion, direct repair
Introduction
A classical description of the supraclavicular nerve given in Gray’s Anatomy indicates that the supraclavicular nerve is one of the superficial branches of the cervical plexus from the roots C3, C4, C5, emerging from the posterior border of the sternocleidomastoid muscle [1]. In its course it descends underneath the platysma muscle and the investing layer of the deep cervical fascia. The nerve divides into medial, intermediate and the lateral branches and pierces the deep fascia a little above the clavicle. The medial branch of the supraclavicular is in close relation with external jugular vein and sternocleidomastoid muscle on the inferiomedial side and supplies the skin as far as the midline and down to the second rib and also to the sternoclavicular joint. The intermediate branch crosses the clavicle to supply the skin over the pectoralis major and deltoid muscles up to the level of second rib. The lateral supraclavicular branch descends superficial to trapezius muscle and the acromion of the scapula, and supplies the skin over the shoulder region and also the acromioclavicular joint.
The external jugular vein begins near the angle of the mandible by the union of the posterior division of the retromandibular vein with the posterior auricular vein. In its course it crosses the sternocleidomastoid muscle obliquely, deep to the platysma, and enters the anterioinferior part of the lateral cervical region. It then pierces the investing layer of deep cervical fascia and terminates in the subclavian vein. It drains most of the scalp and side of the face [2].
Transverse cervical artery, according to Weiglein et al., also known as cervicodorsal trunk, arises laterally from the thyrocervical trunk of subclavian artery [3]. Transverse cervical artery further bifurcates into superficial cervical artery (superficial branch) and dorsal scapular artery (deep branch). These branches run superficially and laterally across the scalenus anterior muscle and trunks of the brachial plexus, 2–3 cm superior to the clavicle. The superficial branch passes deep to the trapezius accompanying the spinal accessory nerve, and the deep branch runs deep to the levator scapulae and rhomboid muscles, supplying both and participating in the arterial anastomoses around the scapula [4].
Case Report
Using conventional dissecting techniques, with a purpose of preparation of the teaching and museum anatomical specimens the triangles of the neck were dissected in a 55-year-old embalmed male cadaver, in the anatomy department of Kasturba Medical College, Manipal, India. There was no sign of trauma, surgery or wound scars in the neck region. The skin, superficial fascia of the neck, the platysma muscles and the superficial investing layer of deep fascia were removed systematically on both sides. The muscles, nerves and vessels were cleaned and exposed on both sides of the neck. Special attention was given to the nerves and vessels of the posterior and anterior triangles on both sides of the neck.
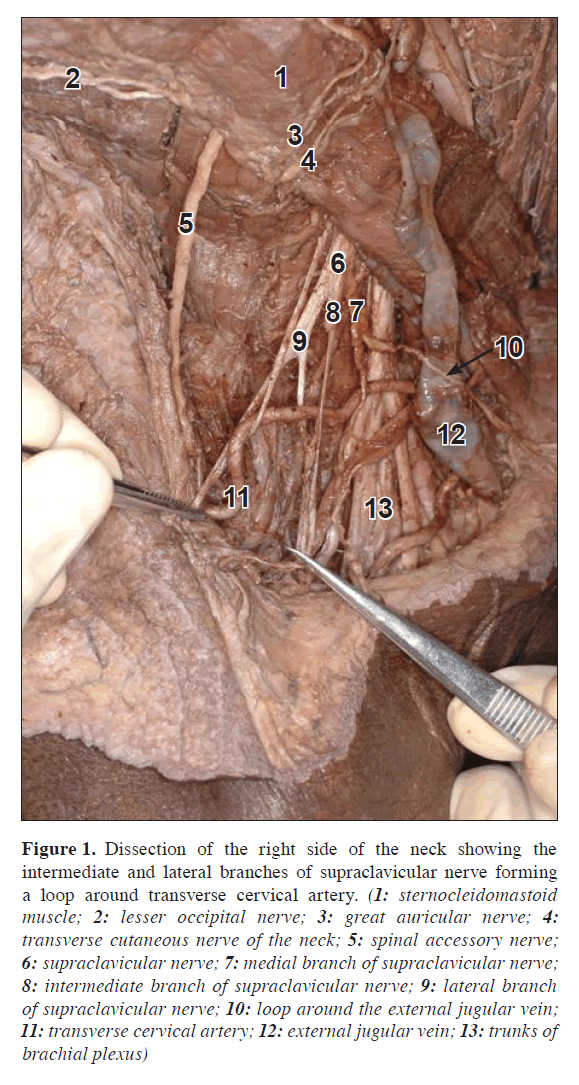
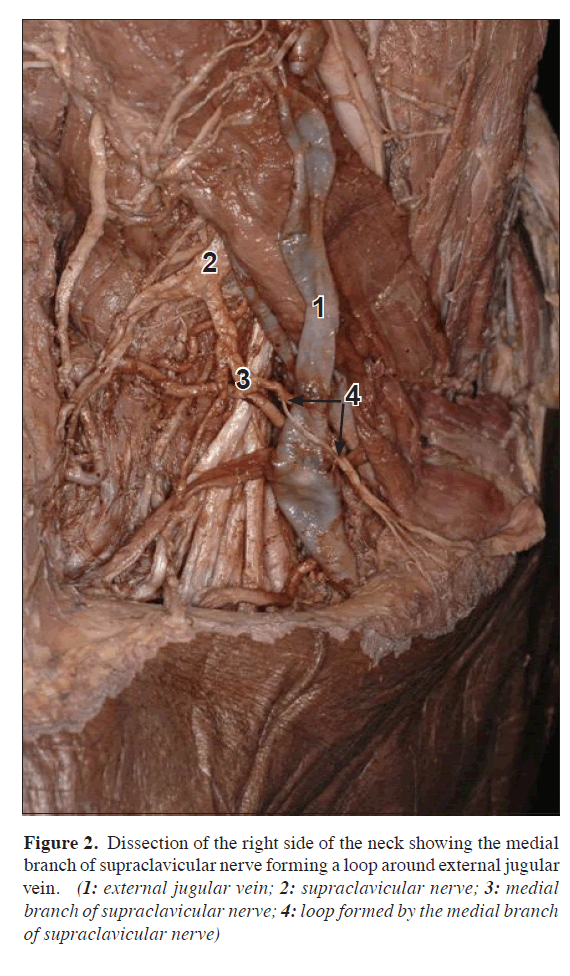
During the dissections of the triangles of the neck, on the posterior triangle of the right side of the neck we observed a rare case of loop formation by the medial, intermediate and lateral branches of the supraclavicular nerve around the external jugular vein and the transverse cervical artery. The medial branch of the supraclavicular nerve formed a loop around the external jugular vein (Figures 1, 2) and the intermediate and the lateral branches of supraclavicular nerve formed loop around the transverse cervical artery (Figure 1). However, we did not observe any variations in further course and distribution of these branches of the supraclavicular nerve.
Figure 1. Dissection of the right side of the neck showing the intermediate and lateral branches of supraclavicular nerve forming a loop around transverse cervical artery. (1: sternocleidomastoid muscle; 2: lesser occipital nerve; 3: great auricular nerve; 4: transverse cutaneous nerve of the neck; 5: spinal accessory nerve; 6: supraclavicular nerve; 7: medial branch of supraclavicular nerve; 8: intermediate branch of supraclavicular nerve; 9: lateral branch of supraclavicular nerve; 10: loop around the external jugular vein; 11: transverse cervical artery; 12: external jugular vein; 13: trunks of brachial plexus)
Figure 2. Dissection of the right side of the neck showing the medial branch of supraclavicular nerve forming a loop around external jugular vein. (1: external jugular vein; 2: supraclavicular nerve; 3: medial branch of supraclavicular nerve; 4: loop formed by the medial branch of supraclavicular nerve)
Discussion
Knowledge of the structure in the human body is not only the domain to the surgeon; it is also essential for effective and responsible clinical practice. It requires many skills that lead to a considered analysis of the patient’s normal or abnormal structure. In this report, we describe an unusual variation of looping of the supraclavicular nerve around the external jugular vein and transverse cervical artery.
The posterior triangle of the neck, including blood vessels, cervical lymph nodes, supraclavicular nerves, brachial plexus and fibro-fatty tissue, is a key landmark during certain surgical procedures [5]. Tubbs RS et al. [6] reported a male cadaver having his right intermediate branch of the supraclavicular nerve piercing the clavicle. Following a review of the literature, it appears that symptoms related to this finding are rare but do occur most commonly involving the intermediate branch of the supraclavicular nerve. Symptoms may be relieved with surgical decompression of the entrapped nerve. Although rare, the clinician should include entrapment of the supraclavicular nerve within the clavicle in their differential diagnosis of shoulder pain. Supraclavicular nerve may give a branch to the phrenic nerve, which will pass down into the thorax over the subclavian artery or vein before joining the phrenic nerve. In 10 of 254 cases, the clavicle was perforated by the middle branch of supraclavicular nerve. It traversed the bone in intraclavicular canal and was visible on x-ray films [7]. For the first time Jelev and Surchev suggested that in addition to the bony canal through the clavicle, certain fibrous and muscular structures could also be an anatomical basis for supraclavicular nerve entrapment syndrome [8]. Due to the unusual looping of the supraclavicular nerve around the external jugular vein and transverse cervical artery in the present case, certain types of trauma could possibly cause neuropathic pain or dysfunction.
The external jugular vein, since it is usually visible in most patients, may serve as a useful venous manometer in cardiac cases. It can also be used for catheterization. Modern general practice requires an ability to handle minor procedures such as venipuncture, regional anesthesia for minor operations, suturing in trauma cases, and catheterization of vessels as well as performing a biopsy. All these procedures require knowledge of anatomical variations. The external jugular veins are so variable that it is not possible to determine a “normal” pattern. Several reports on different types of variations of external jugular vein have been documented in the literature such as, both veins may be very tiny, or one may be much larger than the other. The external jugular vein may be missing on one or both sides; the veins that normally form it then open into the internal jugular vein. It may be formed merely by the posterior auricular vein. On occasion it receives the facial, lingual and cephalic veins. It may pass over the clavicle and open into the cephalic, subclavian or internal jugular vein. The vein is sometimes doubled. The external jugular vein may descend posterior to the inferior belly of the omohyoid. In some cases it forms an annulus around the clavicle. The vein occasionally receives a lingual vein or an accessory external thoracic vein that ascends subcutaneously from the nipple [7]. In the present case unusual looping of medial branch of supraclavicular nerve must be taken into consideration during surgical intervention of the external jugular vein, damage to this branch can lead to loss of sensation in the area of its distribution.
Transverse cervical artery arises from the subclavian artery in about 61% of cases and from the thyrocervical trunk in about 38%. When it arises from the subclavian artery, it is usually behind or lateral to scalenus anterior muscle. It may arise from the dorsal scapular (possibly as high as 20%). In addition, it sometimes arises from the inferior thyroid, internal thoracic arteries, costocervical trunk, or the first part of the subclavian artery. Dorsal scapular nerve making a loop around the deep branch of transverse cervical artery is documented in the literature [9]. As far as the authors are aware there are no published reports to compare our present observation on the variation in the course and branching pattern of supraclavicular nerve.
Conclusion
Variations of the looping of the supraclavicular branches may be asymptomatic; this type of looping might result in the nerve compression caused by the artery. So an extra care must be undertaken even during routine surgical interventions involving removal of deep cervical lymph nodes, supraclavicular brachial plexus block for anesthesia of the upper limb and other neck surgeries.
References
- Berry M, Bannister LH, Standring SM. Nervous system. In: Williams PL, Bannister LH, Berry MM, Collins P, Dyson M, Dussek JE, Ferguson MWJ, eds. Gray’s Anatomy. 38th Ed., Edinburg, Churchill Livingstone. 1995; 1263–1264.
- Anson BJ. Morris’ Human Anatomy. 12th Ed., New York, McGraw-Hill. 1966; 702, 795.
- Weiglein AH, Moriggl B, Schalk C, Kunzel KH, Muller U. Arteries in the posterior cervical triangle in man. Clin Anat. 2005; 18: 553–557.
- Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. 6th Ed. Philadelphia, Lippincott Williams & Wilkins. 2009; 995.
- McGregor IA, McGregor FM. Cancer of the face and mouth: pathology and management for surgeons. 2nd Ed. Edinburgh, Churchill Livingstone. 1986; 156–166.
- Tubbs RS, Salter EG, Oakes WJ. Anomaly of the supraclavicular nerve: case report and review of the literature. Clin Anat. 2006; 19; 599–601.
- Bergman RA, Thomson SA, Afifi AK, Saadeh FA. Compendium of human anatomic variation. Baltimore, Urban & Schwarzenberg. 1988; 70, 89, 139.
- Jelev L, Surchev L. Study of variant anatomical structures (bony canals, fibrous bands, and muscles) in relation to potential supraclavicular nerve entrapment. Clin Anat. 2007; 20: 278–285.
- George BM, Nayak SB. Neuromuscular variations in the posterior triangle of the neck – a case report. Neuroanatomy. 2008; 7: 8–9.
T. Ramesh Rao1*, Prakashchandra Shetty2 and Suresh Rao3
1Department of Paraclinical Sciences, Faculty of Medical Sciences, The University of The West Indies, St. Augustine, Trinidad, West Indies
2Department of Anatomy, Kasturba Medical College, Manipal – 576104, Udupi, Karnataka, India
3Department of Preclinical Sciences, Faculty of Medical Sciences, The University of The West Indies, St. Augustine, Trinidad, West Indies
- *Corresponding Author:
- T. Ramesh Rao, MSc, PhD
Faculty of Medical Sciences, Department of Paraclinical Sciences, Faculty of Medical Sciences, The University of The West Indies, St. Augustine, Trinidad, West Indies
Tel: +1 (868) 662-1472, ext. 5001
Fax: +1 (868) 662-1472
E-mail: varun1195@yahoo.com
Date of Received: November 5th, 2008
Date of Accepted: May 6th, 2009
Published Online: May 11th, 2009
© IJAV. 2009; 2: 48–50.
Abstract
Awareness of the topographic anatomy of various neurovascular variations in the triangles of the neck may serve as a useful guide for radiologists, anesthesiologists and surgeons. It can help to prevent diagnostic errors, influence surgical and interventional procedures and avoid surgical complications during head and neck surgeries. Here we present the detailed case report with review of the literature of a 55-year-old formalin fixed male cadaver showing an unusual loop formation from the three main branches of supraclavicular nerve around the external jugular vein and the transverse cervical artery on the right side of the neck. Such a loop may lead to neurovascular symptoms. Cases bearing this kind of variations should be managed carefully during surgical and/or electrophysiological procedures.
-Keywords
supraclavicular nerve, entrapment, lesion, direct repair
Introduction
A classical description of the supraclavicular nerve given in Gray’s Anatomy indicates that the supraclavicular nerve is one of the superficial branches of the cervical plexus from the roots C3, C4, C5, emerging from the posterior border of the sternocleidomastoid muscle [1]. In its course it descends underneath the platysma muscle and the investing layer of the deep cervical fascia. The nerve divides into medial, intermediate and the lateral branches and pierces the deep fascia a little above the clavicle. The medial branch of the supraclavicular is in close relation with external jugular vein and sternocleidomastoid muscle on the inferiomedial side and supplies the skin as far as the midline and down to the second rib and also to the sternoclavicular joint. The intermediate branch crosses the clavicle to supply the skin over the pectoralis major and deltoid muscles up to the level of second rib. The lateral supraclavicular branch descends superficial to trapezius muscle and the acromion of the scapula, and supplies the skin over the shoulder region and also the acromioclavicular joint.
The external jugular vein begins near the angle of the mandible by the union of the posterior division of the retromandibular vein with the posterior auricular vein. In its course it crosses the sternocleidomastoid muscle obliquely, deep to the platysma, and enters the anterioinferior part of the lateral cervical region. It then pierces the investing layer of deep cervical fascia and terminates in the subclavian vein. It drains most of the scalp and side of the face [2].
Transverse cervical artery, according to Weiglein et al., also known as cervicodorsal trunk, arises laterally from the thyrocervical trunk of subclavian artery [3]. Transverse cervical artery further bifurcates into superficial cervical artery (superficial branch) and dorsal scapular artery (deep branch). These branches run superficially and laterally across the scalenus anterior muscle and trunks of the brachial plexus, 2–3 cm superior to the clavicle. The superficial branch passes deep to the trapezius accompanying the spinal accessory nerve, and the deep branch runs deep to the levator scapulae and rhomboid muscles, supplying both and participating in the arterial anastomoses around the scapula [4].
Case Report
Using conventional dissecting techniques, with a purpose of preparation of the teaching and museum anatomical specimens the triangles of the neck were dissected in a 55-year-old embalmed male cadaver, in the anatomy department of Kasturba Medical College, Manipal, India. There was no sign of trauma, surgery or wound scars in the neck region. The skin, superficial fascia of the neck, the platysma muscles and the superficial investing layer of deep fascia were removed systematically on both sides. The muscles, nerves and vessels were cleaned and exposed on both sides of the neck. Special attention was given to the nerves and vessels of the posterior and anterior triangles on both sides of the neck.
During the dissections of the triangles of the neck, on the posterior triangle of the right side of the neck we observed a rare case of loop formation by the medial, intermediate and lateral branches of the supraclavicular nerve around the external jugular vein and the transverse cervical artery. The medial branch of the supraclavicular nerve formed a loop around the external jugular vein (Figures 1, 2) and the intermediate and the lateral branches of supraclavicular nerve formed loop around the transverse cervical artery (Figure 1). However, we did not observe any variations in further course and distribution of these branches of the supraclavicular nerve.
Figure 1. Dissection of the right side of the neck showing the intermediate and lateral branches of supraclavicular nerve forming a loop around transverse cervical artery. (1: sternocleidomastoid muscle; 2: lesser occipital nerve; 3: great auricular nerve; 4: transverse cutaneous nerve of the neck; 5: spinal accessory nerve; 6: supraclavicular nerve; 7: medial branch of supraclavicular nerve; 8: intermediate branch of supraclavicular nerve; 9: lateral branch of supraclavicular nerve; 10: loop around the external jugular vein; 11: transverse cervical artery; 12: external jugular vein; 13: trunks of brachial plexus)
Figure 2. Dissection of the right side of the neck showing the medial branch of supraclavicular nerve forming a loop around external jugular vein. (1: external jugular vein; 2: supraclavicular nerve; 3: medial branch of supraclavicular nerve; 4: loop formed by the medial branch of supraclavicular nerve)
Discussion
Knowledge of the structure in the human body is not only the domain to the surgeon; it is also essential for effective and responsible clinical practice. It requires many skills that lead to a considered analysis of the patient’s normal or abnormal structure. In this report, we describe an unusual variation of looping of the supraclavicular nerve around the external jugular vein and transverse cervical artery.
The posterior triangle of the neck, including blood vessels, cervical lymph nodes, supraclavicular nerves, brachial plexus and fibro-fatty tissue, is a key landmark during certain surgical procedures [5]. Tubbs RS et al. [6] reported a male cadaver having his right intermediate branch of the supraclavicular nerve piercing the clavicle. Following a review of the literature, it appears that symptoms related to this finding are rare but do occur most commonly involving the intermediate branch of the supraclavicular nerve. Symptoms may be relieved with surgical decompression of the entrapped nerve. Although rare, the clinician should include entrapment of the supraclavicular nerve within the clavicle in their differential diagnosis of shoulder pain. Supraclavicular nerve may give a branch to the phrenic nerve, which will pass down into the thorax over the subclavian artery or vein before joining the phrenic nerve. In 10 of 254 cases, the clavicle was perforated by the middle branch of supraclavicular nerve. It traversed the bone in intraclavicular canal and was visible on x-ray films [7]. For the first time Jelev and Surchev suggested that in addition to the bony canal through the clavicle, certain fibrous and muscular structures could also be an anatomical basis for supraclavicular nerve entrapment syndrome [8]. Due to the unusual looping of the supraclavicular nerve around the external jugular vein and transverse cervical artery in the present case, certain types of trauma could possibly cause neuropathic pain or dysfunction.
The external jugular vein, since it is usually visible in most patients, may serve as a useful venous manometer in cardiac cases. It can also be used for catheterization. Modern general practice requires an ability to handle minor procedures such as venipuncture, regional anesthesia for minor operations, suturing in trauma cases, and catheterization of vessels as well as performing a biopsy. All these procedures require knowledge of anatomical variations. The external jugular veins are so variable that it is not possible to determine a “normal” pattern. Several reports on different types of variations of external jugular vein have been documented in the literature such as, both veins may be very tiny, or one may be much larger than the other. The external jugular vein may be missing on one or both sides; the veins that normally form it then open into the internal jugular vein. It may be formed merely by the posterior auricular vein. On occasion it receives the facial, lingual and cephalic veins. It may pass over the clavicle and open into the cephalic, subclavian or internal jugular vein. The vein is sometimes doubled. The external jugular vein may descend posterior to the inferior belly of the omohyoid. In some cases it forms an annulus around the clavicle. The vein occasionally receives a lingual vein or an accessory external thoracic vein that ascends subcutaneously from the nipple [7]. In the present case unusual looping of medial branch of supraclavicular nerve must be taken into consideration during surgical intervention of the external jugular vein, damage to this branch can lead to loss of sensation in the area of its distribution.
Transverse cervical artery arises from the subclavian artery in about 61% of cases and from the thyrocervical trunk in about 38%. When it arises from the subclavian artery, it is usually behind or lateral to scalenus anterior muscle. It may arise from the dorsal scapular (possibly as high as 20%). In addition, it sometimes arises from the inferior thyroid, internal thoracic arteries, costocervical trunk, or the first part of the subclavian artery. Dorsal scapular nerve making a loop around the deep branch of transverse cervical artery is documented in the literature [9]. As far as the authors are aware there are no published reports to compare our present observation on the variation in the course and branching pattern of supraclavicular nerve.
Conclusion
Variations of the looping of the supraclavicular branches may be asymptomatic; this type of looping might result in the nerve compression caused by the artery. So an extra care must be undertaken even during routine surgical interventions involving removal of deep cervical lymph nodes, supraclavicular brachial plexus block for anesthesia of the upper limb and other neck surgeries.
References
- Berry M, Bannister LH, Standring SM. Nervous system. In: Williams PL, Bannister LH, Berry MM, Collins P, Dyson M, Dussek JE, Ferguson MWJ, eds. Gray’s Anatomy. 38th Ed., Edinburg, Churchill Livingstone. 1995; 1263–1264.
- Anson BJ. Morris’ Human Anatomy. 12th Ed., New York, McGraw-Hill. 1966; 702, 795.
- Weiglein AH, Moriggl B, Schalk C, Kunzel KH, Muller U. Arteries in the posterior cervical triangle in man. Clin Anat. 2005; 18: 553–557.
- Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. 6th Ed. Philadelphia, Lippincott Williams & Wilkins. 2009; 995.
- McGregor IA, McGregor FM. Cancer of the face and mouth: pathology and management for surgeons. 2nd Ed. Edinburgh, Churchill Livingstone. 1986; 156–166.
- Tubbs RS, Salter EG, Oakes WJ. Anomaly of the supraclavicular nerve: case report and review of the literature. Clin Anat. 2006; 19; 599–601.
- Bergman RA, Thomson SA, Afifi AK, Saadeh FA. Compendium of human anatomic variation. Baltimore, Urban & Schwarzenberg. 1988; 70, 89, 139.
- Jelev L, Surchev L. Study of variant anatomical structures (bony canals, fibrous bands, and muscles) in relation to potential supraclavicular nerve entrapment. Clin Anat. 2007; 20: 278–285.
- George BM, Nayak SB. Neuromuscular variations in the posterior triangle of the neck – a case report. Neuroanatomy. 2008; 7: 8–9.