A simplified approach to the treatment of erectile dysfunction Based on the Canadian Urology Association Erectile Dysfunction Guidelines
- *Corresponding Author:
- Dr GB Brock
Department of Urology, St Joseph?s Health Care London, London, Ontario N6A 4V2.
Telephone: 519-646-6042
fax: 519-646-6037
E-mail: gebrock@attcanada.ca
Keywords
Diagnosis; Erectile dysfunction; Evaluation; Impotence
Dramatic advances in the understanding of the causes of erectile dysfunction (ED) have occurred over the past decade. Sildenafil citrate (Viagra, Pfizer Inc, USA), the first effective oral agent for ED is currently available, and others are under regulatory review and should be available in Canada by the end of 2003. These developments have fueled public interest and transformed the way in which couples with sexual dysfunction seek help. The patient is now often the source of referral, with many health care visits initiated and conversations about sexual concerns started following direct requests from patients.
This mandates that clinicians are comfortable discussing these topics and that they are up-to-date on the therapeutics and approaches to treatment.
The present article is based on the guidelines from the Canadian Urology Association, approved June 2002.
Summary Concepts
• ED is the preferred clinical term to describe the inability to achieve and maintain a penile erection of sufficient rigidity to permit satisfactory sexual activity.
• Diagnosis and treatment of ED are performed most effectively by primary care physicians (PCPs).
• The underlying risk factors associated with ED are common to cardiovascular disease in general and, therefore, may represent the initial clinical sign of generalized vascular insufficiency.
• PCPs, urologists, internists, psychiatrists and other health care professionals should be encouraged to initiate an open dialogue of sexual issues to identify men with ED who may not otherwise volunteer their sexual concerns.
• Frequently, a careful history, physical examination, and serum glucose, lipids and optional testosterone testing are all that are needed to diagnose ED and to initiate first-line therapy.
• Organic (physical) causes of ED are present in the majority of men, but situational factors often contribute, and addressing these issues may enhance treatment efficacy.
• When reversible causes of ED have been ruled out, a trial of oral medication is recommended as first-line therapy based on treatment efficacy, side effect profile and minimal invasiveness.
• Specialized testing and referral are generally reserved for cases in which greater insight into the etiology is desired by the patient and/or physician, or when oral first-line treatment was unsuccessful or not appropriate.
• Second-line therapies, although more invasive than oral agents, are generally well tolerated and effective.
• Surgery is an important option for those men unresponsive to medical management, and offers durable and reliable relief from ED.
Background
ED is a highly prevalent condition that impacts the quality of life of thousands of Canadian couples. Dramatic advances in understanding the pathophysiology of erection have led to the development of new, highly effective, minimally invasive therapeutic agents.
PCPs are rapidly acquiring the diagnostic and therapeutic skills necessary to become the dominant health care providers for this condition. Armed with effective oral agents able to treat ED, such as the phosphodiesterase type- 5 inhibitors (PDE-5i) and the promise of a multitude of other new oral and sublingual agents in the research pipeline, ED is becoming more of a medical than surgical clinical entity. Family physicians, internists, cardiologists and other medical specialists are approached by couples with ED who are requesting treatment. In many cases, longstanding relationships exist between the couple and their treating physician, which fosters an important therapeutic alliance that may translate into an improved clinical response to the selected treatment approach. A shared-care model for the treatment of ED, in which PCPs initially identify and treat patients with ED and refer those individuals who require more invasive or specialized testing and treatment, is a valid concept. The combined experience and knowledge of PCPs, coupled with the diverse knowledge of specialists, may result in optimal care for the patient.
The present suggestions for management are based on peer-reviewed literature, the 1999 World Heath Organization consensus panel, and the evolving research on new medical approaches to ED management – all placed into a Canadian perspective, as described in the 2002 Canadian Urology Association guidelines [1-7].
Global Management Objectives
• To establish treatment of patient and partner.
• Use of diagnostic tests based on the patient’s presenting complaints and goals of therapy.
• To provide the patient and partner with a diagnosis and understanding of the likely etiology of ED.
• To offer treatment choices with comprehensive information on cost, likelihood of success and common side effects.
• To initiate therapy with the least invasive option that satisfies the patient’s and partner’s goals of treatment.
• To re-establish the couple’s ability to achieve and maintain sexual intimacy in as natural a manner as possible.
The Step-Wise Approach to the Patient
Diagnosis
• Determine that ED exists, rather than premature ejaculation or sexual dysfunction from other causes (eg, Peyronie’s disease or a low desire state).
• Establish the timing of onset, nature of the problem and significance to the couple.
• Evaluate whether a potentially reversible cause of ED exists (eg, patient takes medication; is under stress; has depression or hormonal imbalance; uses tobacco, alcohol or drugs; or has partner-specific issues).
• Categorize the etiology based on the patient’s history, physical examination and laboratory testing (optional). A commonly used schema for testing is:
• Organic
– Vascular
– Endocrine
– Neurological
– End organ (penile deformity)
– Mixed
• Nonorganic
– Situational
– Mixed
Methods
• History and clinical questioning (this is the most important component of the ED evaluation).
• A focused physical examination (directed at neural and vascular systems essential for achieving and maintaining erections).
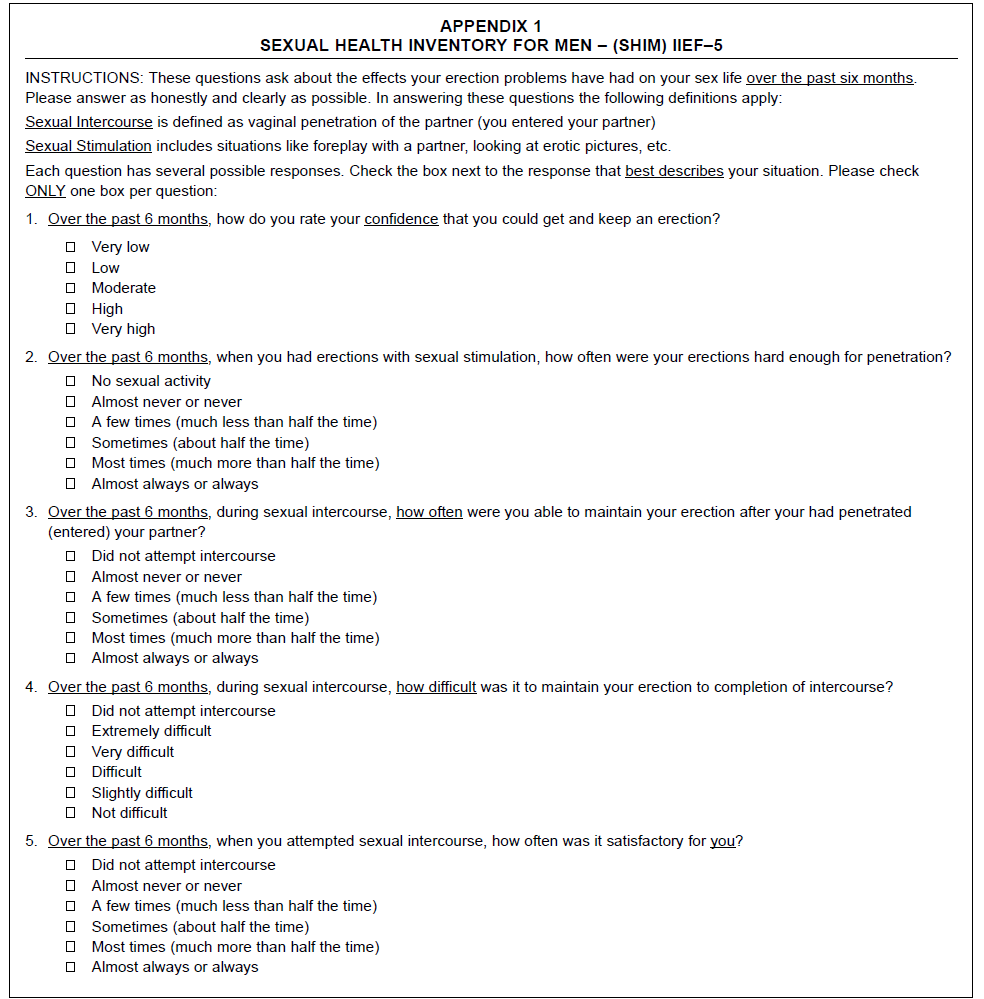
• Questionnaires (eg, International Index of Erectile Function, Sexual Health Inventory for Men [Appendix 1]).
• Laboratory tests, including serum glucose, hormonal screening (total testosterone or bioavailable testosterone) and lipid screening.
• Referrals to endocrinology, cardiology and psychology, when appropriate
• Specialized tests
– In-office intracavernous injections
– Duplex ultrasound with vasoactive penile injection
– Dynamic infusion cavernosography and cavernosometry
– Penile angiogram
Treatment choices
• Sexual counselling (This may represent a spectrum of approaches, from a simple open discussion with the PCP to sexual therapists or psychiatry experts in intimacy-building and sensate focus therapy.)
• Oral therapy (PDE-5i) or hormonal supplementation, if required
• Vacuum device
• Local therapy (intraurethral or intracaverous agents)
• Surgery
– Penile implant
– Surgical repair for Peyronie’s disease
• Vascular bypass procedure (generally reserved for young men following traumatic penile vascular injury
Making the Diagnosis
History
The patient’s medical history is the cornerstone of the evaluation of sexual dysfunction and ED. The patient’s history will provide the likely diagnosis in the majority of cases. There are a variety of approaches to obtaining a thorough history, the most common of which is a supportive health care professional allowing the couple to relate their concerns and express their goals of treatment in an unhurried manner.
Key components of the history are:
• Situations, onset, severity, significance of ED
• The patient’s sexual desire, relationship issues, stress at home, and stress at work
• Lifestyle factors, including smoking, and substance use and/or abuse
• Comorbid conditions, including hypertension, peripheral vascular disease, diabetes and renal disease
• Pelvic surgery or radiation
• Medications
• Psychiatric illness or conditions
• Genital pain or altered shape
Use of validated questionnaires may be of significant benefit when diagnosing ED. Questionnaires can be patient selfadministered. Their greatest utility may be in establishing a response to therapy and determining overall satisfaction with drug use over a specified length of time (eg, four weeks). The Sexual Health Inventory for Men is shown in Appendix 1.
Physical examination
A strong association exists between ED and peripheral vascular disease and occult coronary syndromes. The physical examination may be an important opportunity to unmask these conditions. Assessment should include body habitus (secondary sexual characteristics), the peripheral circulation, neurological systems and genitourinary systems.
Identification of penile deformities such as Peyronie’s disease may be best achieved by stretching the penis to make the plaque more pronounced.
Laboratory tests
Assessment for occult diabetes may be performed with a fasting glucose or Hemoglobin A1c. Although recommended by the World Health Organization consensus panel, a lipid screen is not a routine component of the Canadian ED assessment, but is considered to be a valuable addition to the evaluation and a good general practice.
Hormonal profile screening is a controversial aspect of the routine evaluation of ED. In general, in men with ED and hypoactive desire, testing and treatment for low levels of testosterone is appropriate. In men with normal desire and ED, the need for global testing is controversial and currently unclear. Although it is beyond the scope of the present article, hormonal supplementation is contraindicated in men with breast or prostate cancer. Once initiated on exogenous testosterone, ongoing follow-up is recommended.
Optional tests for thyroid-stimulating hormone, luteinizing hormone and prolactin, as well as a complete blood count and urinalysis, are complementary and are not essential in the evaluation of ED in most cases.
Specialized testing
Psychological and/or psychiatric referrals: May provide important complementary insight into relationships and situational causes of ED. These assessments do not form a routine component of the ED workup and should be considered in the unusual case.
Vascular testing: A variety of vascular tests exist. Historically, a penile brachial index (PBI) assessment was used. The PBI is a noninvasive test that records penile pressure as an index of arm pressure, providing a rough idea of the penile circulation.
The availability of a duplex scan is common. The ultrasound scanner localizes and measures the flow through the cavernous vessels, before and after vasoactive injection, and allows a more refined assessment of the penile circulation.
The dynamic infusion cavernosometry and cavernosography measure the rise and fall of intrapenile pressure with radiological visualization of the veins draining the penis to determine whether there is a competent veno-occlusive mechanism.
The penile angiogram is reserved for cases of high-flow priapism or planned vascular bypass. This test allows visualization of the penile circulation and directs embolization for the unusual cases of penile injury-induced, high-flow priapism.
Endocrinological tests: There is controversy about what is the ideal endocrine workup for men with ED. Testing for morning total testosterone, or bioavailable testosterone, is logical in cases in which sexual interest or significant reduction in ejaculate volume are present. Free testosterone measurement may have significant intra-assay variability, which may limit its clinical utility.
Neurophysiological testing: This form of testing generally allows for measurement of the sacral reflex arc – an indirect measure of the perineal neural integrity.
Recommendations
• Detailed history and physical examination are the essential elements of the ED workup.
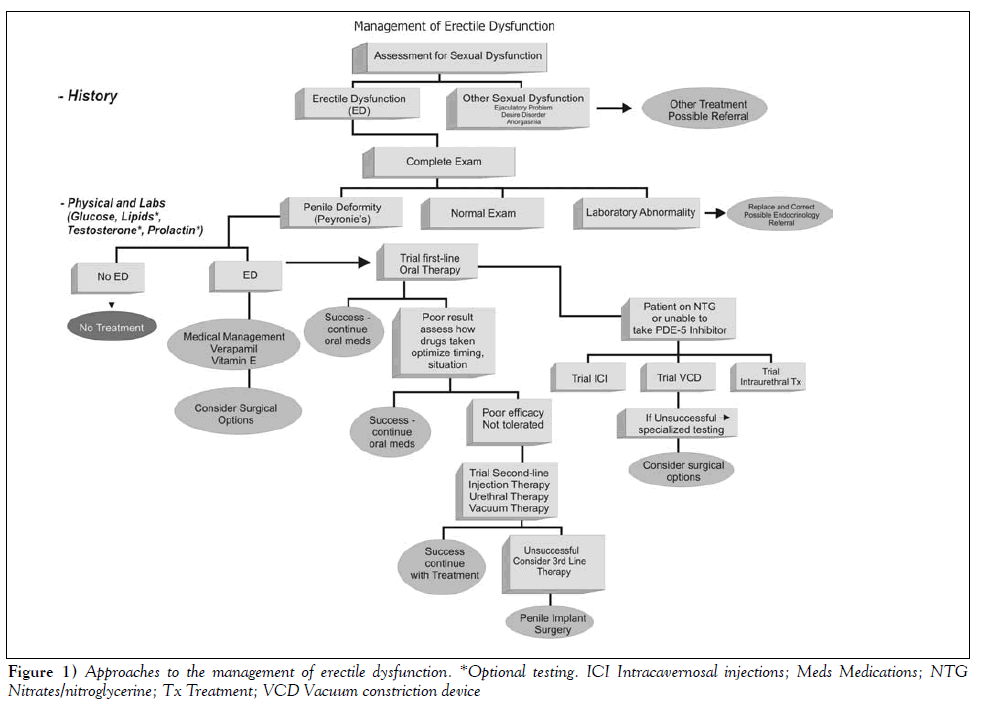
• A step-wise algorithmic treatment approach initiating treatment with the least invasive option is suggested.
• When failure of the initial oral medication is encountered, trials of more invasive second-line treatment or investigations may be appropriate.
• Surgery should be reserved for men in whom less invasive reversible treatments have not succeeded or are contraindicated.
• Treatment should be individualized, and follow-up arranged to assess the efficacy and satisfaction of treatment.
References
- Jardin A, Wagner G, Khoury S, et al. Recommendations of the first international consultation on erectile dysfunction. World Health Organization, International Consultation on Urological Diseases; Societe Internationale d?Urologie. Paris, July 1-3, 1999.
- Ralph D, McNicholas T. UK management guidelines for erectile dysfunction. BMJ 2000;321:499-503.
- NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA 1993;270:83-90.
- Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ,McKinlay JB. Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. J Urol 1994;151:54-61.
- Benet AE, Melman A. The epidemiology of erectile dysfunction. Urol Clin North Am 1995;22:699-709.
- McKinlay JB. The worldwide prevalence and epidemiology of erectile dysfunction. Int J Impot Res 2000;12(Suppl 4):S6-11.
- Aytac IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int 1999;84:50-6.
- *Corresponding Author:
- Dr GB Brock
Department of Urology, St Joseph?s Health Care London, London, Ontario N6A 4V2.
Telephone: 519-646-6042
fax: 519-646-6037
E-mail: gebrock@attcanada.ca
Abstract
Advances in the diagnosis and treatment of erectile dysfunction (ED) over the past decade have led to a refined approach to the management of this common disorder. Recently, the Canadian Male Sexual Health Council, in conjunction with the Guidelines Committee of the Canadian Urology Association, developed an ED treatment guideline for physicians. This step-wise approach using oral agents and a minimal workup as the first-line approach, followed by more invasive second- and third-line treatments in difficult to treat cases, has become accepted management in most developed countries. A simplified treatment algorithm is presented, highlighting this treatment strategy
-Keywords
Diagnosis; Erectile dysfunction; Evaluation; Impotence
Dramatic advances in the understanding of the causes of erectile dysfunction (ED) have occurred over the past decade. Sildenafil citrate (Viagra, Pfizer Inc, USA), the first effective oral agent for ED is currently available, and others are under regulatory review and should be available in Canada by the end of 2003. These developments have fueled public interest and transformed the way in which couples with sexual dysfunction seek help. The patient is now often the source of referral, with many health care visits initiated and conversations about sexual concerns started following direct requests from patients.
This mandates that clinicians are comfortable discussing these topics and that they are up-to-date on the therapeutics and approaches to treatment.
The present article is based on the guidelines from the Canadian Urology Association, approved June 2002.
Summary Concepts
• ED is the preferred clinical term to describe the inability to achieve and maintain a penile erection of sufficient rigidity to permit satisfactory sexual activity.
• Diagnosis and treatment of ED are performed most effectively by primary care physicians (PCPs).
• The underlying risk factors associated with ED are common to cardiovascular disease in general and, therefore, may represent the initial clinical sign of generalized vascular insufficiency.
• PCPs, urologists, internists, psychiatrists and other health care professionals should be encouraged to initiate an open dialogue of sexual issues to identify men with ED who may not otherwise volunteer their sexual concerns.
• Frequently, a careful history, physical examination, and serum glucose, lipids and optional testosterone testing are all that are needed to diagnose ED and to initiate first-line therapy.
• Organic (physical) causes of ED are present in the majority of men, but situational factors often contribute, and addressing these issues may enhance treatment efficacy.
• When reversible causes of ED have been ruled out, a trial of oral medication is recommended as first-line therapy based on treatment efficacy, side effect profile and minimal invasiveness.
• Specialized testing and referral are generally reserved for cases in which greater insight into the etiology is desired by the patient and/or physician, or when oral first-line treatment was unsuccessful or not appropriate.
• Second-line therapies, although more invasive than oral agents, are generally well tolerated and effective.
• Surgery is an important option for those men unresponsive to medical management, and offers durable and reliable relief from ED.
Background
ED is a highly prevalent condition that impacts the quality of life of thousands of Canadian couples. Dramatic advances in understanding the pathophysiology of erection have led to the development of new, highly effective, minimally invasive therapeutic agents.
PCPs are rapidly acquiring the diagnostic and therapeutic skills necessary to become the dominant health care providers for this condition. Armed with effective oral agents able to treat ED, such as the phosphodiesterase type- 5 inhibitors (PDE-5i) and the promise of a multitude of other new oral and sublingual agents in the research pipeline, ED is becoming more of a medical than surgical clinical entity. Family physicians, internists, cardiologists and other medical specialists are approached by couples with ED who are requesting treatment. In many cases, longstanding relationships exist between the couple and their treating physician, which fosters an important therapeutic alliance that may translate into an improved clinical response to the selected treatment approach. A shared-care model for the treatment of ED, in which PCPs initially identify and treat patients with ED and refer those individuals who require more invasive or specialized testing and treatment, is a valid concept. The combined experience and knowledge of PCPs, coupled with the diverse knowledge of specialists, may result in optimal care for the patient.
The present suggestions for management are based on peer-reviewed literature, the 1999 World Heath Organization consensus panel, and the evolving research on new medical approaches to ED management – all placed into a Canadian perspective, as described in the 2002 Canadian Urology Association guidelines [1-7].
Global Management Objectives
• To establish treatment of patient and partner.
• Use of diagnostic tests based on the patient’s presenting complaints and goals of therapy.
• To provide the patient and partner with a diagnosis and understanding of the likely etiology of ED.
• To offer treatment choices with comprehensive information on cost, likelihood of success and common side effects.
• To initiate therapy with the least invasive option that satisfies the patient’s and partner’s goals of treatment.
• To re-establish the couple’s ability to achieve and maintain sexual intimacy in as natural a manner as possible.
The Step-Wise Approach to the Patient
Diagnosis
• Determine that ED exists, rather than premature ejaculation or sexual dysfunction from other causes (eg, Peyronie’s disease or a low desire state).
• Establish the timing of onset, nature of the problem and significance to the couple.
• Evaluate whether a potentially reversible cause of ED exists (eg, patient takes medication; is under stress; has depression or hormonal imbalance; uses tobacco, alcohol or drugs; or has partner-specific issues).
• Categorize the etiology based on the patient’s history, physical examination and laboratory testing (optional). A commonly used schema for testing is:
• Organic
– Vascular
– Endocrine
– Neurological
– End organ (penile deformity)
– Mixed
• Nonorganic
– Situational
– Mixed
Methods
• History and clinical questioning (this is the most important component of the ED evaluation).
• A focused physical examination (directed at neural and vascular systems essential for achieving and maintaining erections).
• Questionnaires (eg, International Index of Erectile Function, Sexual Health Inventory for Men [Appendix 1]).
• Laboratory tests, including serum glucose, hormonal screening (total testosterone or bioavailable testosterone) and lipid screening.
• Referrals to endocrinology, cardiology and psychology, when appropriate
• Specialized tests
– In-office intracavernous injections
– Duplex ultrasound with vasoactive penile injection
– Dynamic infusion cavernosography and cavernosometry
– Penile angiogram
Treatment choices
• Sexual counselling (This may represent a spectrum of approaches, from a simple open discussion with the PCP to sexual therapists or psychiatry experts in intimacy-building and sensate focus therapy.)
• Oral therapy (PDE-5i) or hormonal supplementation, if required
• Vacuum device
• Local therapy (intraurethral or intracaverous agents)
• Surgery
– Penile implant
– Surgical repair for Peyronie’s disease
• Vascular bypass procedure (generally reserved for young men following traumatic penile vascular injury
Making the Diagnosis
History
The patient’s medical history is the cornerstone of the evaluation of sexual dysfunction and ED. The patient’s history will provide the likely diagnosis in the majority of cases. There are a variety of approaches to obtaining a thorough history, the most common of which is a supportive health care professional allowing the couple to relate their concerns and express their goals of treatment in an unhurried manner.
Key components of the history are:
• Situations, onset, severity, significance of ED
• The patient’s sexual desire, relationship issues, stress at home, and stress at work
• Lifestyle factors, including smoking, and substance use and/or abuse
• Comorbid conditions, including hypertension, peripheral vascular disease, diabetes and renal disease
• Pelvic surgery or radiation
• Medications
• Psychiatric illness or conditions
• Genital pain or altered shape
Use of validated questionnaires may be of significant benefit when diagnosing ED. Questionnaires can be patient selfadministered. Their greatest utility may be in establishing a response to therapy and determining overall satisfaction with drug use over a specified length of time (eg, four weeks). The Sexual Health Inventory for Men is shown in Appendix 1.
Physical examination
A strong association exists between ED and peripheral vascular disease and occult coronary syndromes. The physical examination may be an important opportunity to unmask these conditions. Assessment should include body habitus (secondary sexual characteristics), the peripheral circulation, neurological systems and genitourinary systems.
Identification of penile deformities such as Peyronie’s disease may be best achieved by stretching the penis to make the plaque more pronounced.
Laboratory tests
Assessment for occult diabetes may be performed with a fasting glucose or Hemoglobin A1c. Although recommended by the World Health Organization consensus panel, a lipid screen is not a routine component of the Canadian ED assessment, but is considered to be a valuable addition to the evaluation and a good general practice.
Hormonal profile screening is a controversial aspect of the routine evaluation of ED. In general, in men with ED and hypoactive desire, testing and treatment for low levels of testosterone is appropriate. In men with normal desire and ED, the need for global testing is controversial and currently unclear. Although it is beyond the scope of the present article, hormonal supplementation is contraindicated in men with breast or prostate cancer. Once initiated on exogenous testosterone, ongoing follow-up is recommended.
Optional tests for thyroid-stimulating hormone, luteinizing hormone and prolactin, as well as a complete blood count and urinalysis, are complementary and are not essential in the evaluation of ED in most cases.
Specialized testing
Psychological and/or psychiatric referrals: May provide important complementary insight into relationships and situational causes of ED. These assessments do not form a routine component of the ED workup and should be considered in the unusual case.
Vascular testing: A variety of vascular tests exist. Historically, a penile brachial index (PBI) assessment was used. The PBI is a noninvasive test that records penile pressure as an index of arm pressure, providing a rough idea of the penile circulation.
The availability of a duplex scan is common. The ultrasound scanner localizes and measures the flow through the cavernous vessels, before and after vasoactive injection, and allows a more refined assessment of the penile circulation.
The dynamic infusion cavernosometry and cavernosography measure the rise and fall of intrapenile pressure with radiological visualization of the veins draining the penis to determine whether there is a competent veno-occlusive mechanism.
The penile angiogram is reserved for cases of high-flow priapism or planned vascular bypass. This test allows visualization of the penile circulation and directs embolization for the unusual cases of penile injury-induced, high-flow priapism.
Endocrinological tests: There is controversy about what is the ideal endocrine workup for men with ED. Testing for morning total testosterone, or bioavailable testosterone, is logical in cases in which sexual interest or significant reduction in ejaculate volume are present. Free testosterone measurement may have significant intra-assay variability, which may limit its clinical utility.
Neurophysiological testing: This form of testing generally allows for measurement of the sacral reflex arc – an indirect measure of the perineal neural integrity.
Recommendations
• Detailed history and physical examination are the essential elements of the ED workup.
• A step-wise algorithmic treatment approach initiating treatment with the least invasive option is suggested.
• When failure of the initial oral medication is encountered, trials of more invasive second-line treatment or investigations may be appropriate.
• Surgery should be reserved for men in whom less invasive reversible treatments have not succeeded or are contraindicated.
• Treatment should be individualized, and follow-up arranged to assess the efficacy and satisfaction of treatment.
References
- Jardin A, Wagner G, Khoury S, et al. Recommendations of the first international consultation on erectile dysfunction. World Health Organization, International Consultation on Urological Diseases; Societe Internationale d?Urologie. Paris, July 1-3, 1999.
- Ralph D, McNicholas T. UK management guidelines for erectile dysfunction. BMJ 2000;321:499-503.
- NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA 1993;270:83-90.
- Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ,McKinlay JB. Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. J Urol 1994;151:54-61.
- Benet AE, Melman A. The epidemiology of erectile dysfunction. Urol Clin North Am 1995;22:699-709.
- McKinlay JB. The worldwide prevalence and epidemiology of erectile dysfunction. Int J Impot Res 2000;12(Suppl 4):S6-11.
- Aytac IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int 1999;84:50-6.