A unique lpsilateral axillary artery variation
Received: 07-Jan-2021 Accepted Date: Feb 02, 2021; Published: 09-Feb-2021, DOI: 10.37532/1308-4038.14(2).159-162
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
In an 87-year-old male cadaver received through the Gift Body Program at Saint Louis University School of Medicine, a common arterial trunk arose from the third part of the left axillary artery (AA) that divided into the subscapular artery (SA) and a common stem for the deep brachial artery (DBA), the anterior humeral circumflex artery (AHCA), and the posterior humeral circumflex artery (PHCA). Both the SA and AHCA appeared normal. The PHCA traveled through the quadrangular space and gave off the radial collateral artery (RCA) in the posterior arm which anastomosed with the radial recurrent artery. The DBA traveled through the triangular interval and continued as the middle collateral artery (MCA) in the posterior arm to anastomose with the interosseous recurrent artery. Lastly, the medial and lateral cord contributions to the median nerve formed posteriorly to the AA. Knowing anatomical variation of the AA has clinical and embryological significance.
Keywords
Axillary artery; Median nerve; Deep brachial artery; Arterial variations.
Introduction
The AA is a direct continuation of the subclavian artery, beginning at the lateral border of the first rib and continuing as the brachial artery distal to the inferior border of the teres minor muscle. Anatomically, the AA is divided into three parts, each giving rise to characteristic branches. The first part of the AA begins at the lateral border of the first rib and ends at the superior border of the pectoralis minor muscle. It gives a single branch, the superior thoracic artery, which supplies the superficial aspect of the first two intercostal spaces. The second part of the AA exists deep to the pectoralis minor muscle and typically gives off the thoracoacromial trunk and the lateral thoracic artery. Finally, the third part of the AA begins at the inferior border of the pectoralis minor muscle and ends at the inferior border of the teres major muscle, continuing as the brachial artery. The third part of the AA usually gives off three branches, the SA, which is the largest branch, the AHCA, and the PHCA. As a continuation of the AA, the brachial artery courses through the upper arm and gives off several muscular branches. It also gives off three named branches including a larger DBA, and both the superior and inferior ulnar collateral arteries. The DBA travels posteriorly along the radial sulcus of the humerus, deep to the triceps brachii, and through the triangular interval, along with the radial nerve. It terminates by branching into the RCA and the MCA. The brachial artery continues into the forearm where it bifurcates into the radial and ulnar arteries.
The elbow joint has a rich collateral circulation formed by collateral branches from the arm and recurrent branches from the forearm. Collateral circulation permits multiple paths to vascularization of the elbow; in the case that one path is compromised. The radial recurrent artery, a branch of the radial artery, anastomoses with the RCA deep to the brachialis muscles and superficial to the lateral epicondyle. Deep to the anconeus muscle, the MCA runs with the nerve to the anconeus muscle and anastomoses with the recurrent interosseous artery, a branch of the posterior interosseous artery. Additionally, the anterior and posterior ulnar recurrent arteries arising from ulnar artery anastomose with inferior and superior ulnar collateral arteries, respectively.
Case Report
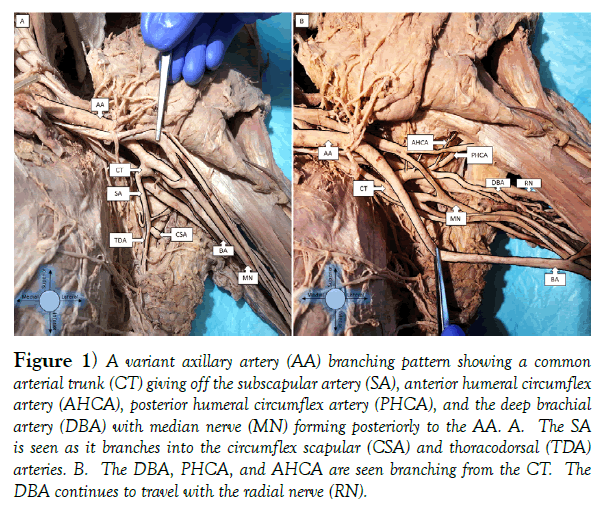
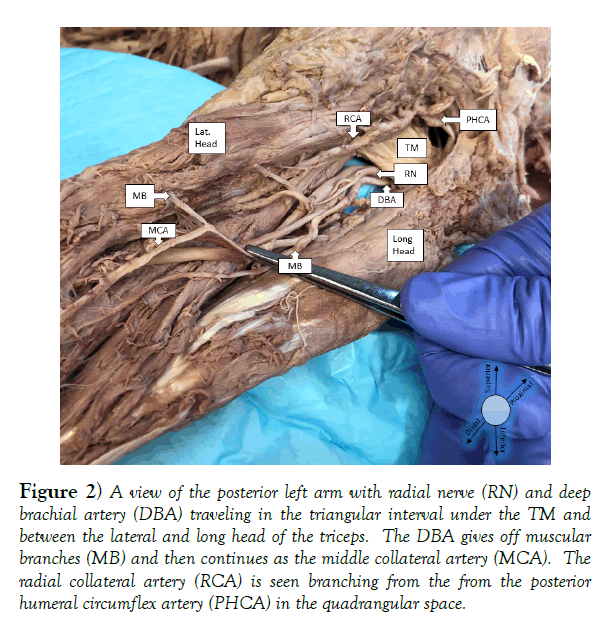
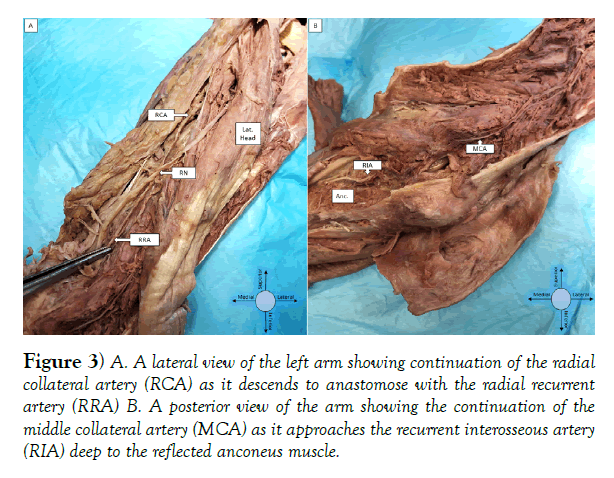
During the routine dissection of the left axillary region on an 87-year-old male cadaver, a common arterial trunk for the SA, AHCA, PHCA and DBA was discovered arising from the 3rd part of the left AA. This common trunk projected inferiorly from the posterior aspect of the AA. It quickly gave off the SA branch, which traveled inferiorly, along the ventral aspect of the scapula, branching into the circumflex scapular artery (CSA) and the thoracodorsal artery (TDA) (Figure 1). The CSA passed through the triangular space anastomosing with suprascapular and dorsal scapular arteries to supply the surrounding structures, while the TDA traveled to supply the latissimusdorsi muscle. Overall, the SA and its branches displayed typical branching patterns and routes. The common stem for the DBA, AHCA, PHCA, and several muscle branches was observed with some atypical paths (Figure 1). The DBA traveled with the radial nerve, coursed posteriorly to the humerus, anterior to the tendon of the teres major, and then entered the triangular interval. The DBA gave off several muscular branches as it traveled in the radial groove, eventually continuing as the MCA in the posterior compartment of the arm (Figure 2). Notably, the RCA was missing from the DBA. Distally, the MCA anastomosed with the recurrent interosseous artery, just deep to the anconeus muscle (Figure 3). All other branches of the DBA were observed terminating within the muscle belly of the triceps brachii muscle.
Figure 1) A variant axillary artery (AA) branching pattern showing a common arterial trunk (CT) giving off the subscapular artery (SA), anterior humeral circumflex artery (AHCA), posterior humeral circumflex artery (PHCA), and the deep brachial artery (DBA) with median nerve (MN) forming posteriorly to the AA. A. The SA is seen as it branches into the circumflex scapular (CSA) and thoracodorsal (TDA) arteries. B. The DBA, PHCA, and AHCA are seen branching from the CT. The DBA continues to travel with the radial nerve (RN).
Figure 2) A view of the posterior left arm with radial nerve (RN) and deep brachial artery (DBA) traveling in the triangular interval under the TM and between the lateral and long head of the triceps. The DBA gives off muscular branches (MB) and then continues as the middle collateral artery (MCA). The radial collateral artery (RCA) is seen branching from the from the posterior humeral circumflex artery (PHCA) in the quadrangular space.
Figure 3) A. A lateral view of the left arm showing continuation of the radial collateral artery (RCA) as it descends to anastomose with the radial recurrent artery (RRA) B. A posterior view of the arm showing the continuation of the middle collateral artery (MCA) as it approaches the recurrent interosseous artery (RIA) deep to the reflected anconeus muscle.
The small AHCA of the common stem traveled anteriorly along the surgical neck of the humerus (Figure 1). It gave off a small number of branches to the shoulder joint and muscles around the area. The PHCA was the final branch of the common stem (Figure 1), which traveled with the axillary nerve through the quadrangular space posterior to the humerus (Figure 2). In addition to some small muscular branches, the PHCA crossed posterior to the teres major and continued as the RCA in the posterior compartment of the arm (Figure 2). In order to evaluate collateral circulation of the RCA, the radial recurrent artery was dissected in the antecubital fossa and followed proximally. It traveled anterior to the lateral epicondyle to anastomose with the RCA (Figure 3). To ascertain any other variations in this cadaver, the brachial plexus and all other nervous and vascular structures of the left arm and axilla were investigated. Proximally, the branching pattern of the brachial plexus appeared to be typical except for the median nerve which formed posteriorly to the AA. The medial cord contribution was seen passing anterior to the CT while the lateral cord contribution was observed running in between the CT and AA (Figure 1). The median nerve then traveled distally along the BA. The BA terminated in the antecubital fossa as it split into the ulnar and radial arteries. The branching pattern of all other vasculature of the left axilla and arm was typical. There were no variations in the arterial branching pattern of the right axilla or arm.
Discussion
Vascular variation of the axilla and upper extremity is relatively common, and there are a plethora of reports covering anomalies of the superior thoracic artery, PHCA, and the BA [1-3]. There is also extensive literature on the AA branching into a superficial and deep brachial artery [4,5]. However, the presence of a common trunk for the branches of the third part of the AA and the DBA is less documented. Five reported cases of a similar common trunk to that which we present in this study were found in the literature [6-10]. While there are similarities between the common trunks, no reports were found that present collateral circulation around the elbow as described in this case study. (Table 1) provides a summary of other cadaveric observations of a common trunk for the branches of the third part of the AA and the DBA or branches of the DBA.
| Authors | Year | Common Trunk Findings | Collateral Circulation Findings |
|---|---|---|---|
| Samuel et al. [6] | 2006 | CT branches into SA, AHCA, and PHCA and gives collateral elbow circulation. Complete absence of DBA. The median nerve forms posterior to the AA, circumscribing the CT. | CT continues to give off the superior ulnar collateral artery, radial collateral artery, and the middle collateral artery. No discussion of the inferior ulnar collateral artery. |
| George et al. [7] | 2007 | CT branches into the SA, AHCA, and PHCA and continues as the DBA. The median nerve forms posterior to the AA, circumscribing the CT. | Collateral circulation of the elbow not discussed. |
| Ramesh Rao et al. [8] | 2008 | CT branches into the SA, ACHA, and PHCA. The DBA is a branch of the CT, with the CT continuing as the ulnar collateral arteries. The median nerve forms posteriorly to the AA, circumscribing the CT. | Ulnar collateral arteries branch directly from the CT. No discussion of the radial collateral circulation. |
| Kumar et al. [9] | 2014 | CT branches into the SA, AHCA, and PHCA and continues as the DBA. The median nerve forms posterior to the AA, circumscribing the CT. | Collateral circulation of the elbow not discussed. |
| Aastha et al. [10] | 2015 | CT branches into the SA, AHCA, and PHCA and continues as the DBA. The median nerve forms posteriorly to the AA, circumscribing the CT. | DBA branches into the ulnar collateral arteries. No discussion of the radial collateral circulation. |
Table 1: Cadaveric observations of a common trunk for branches of the 3rd part of the AA and DBA.
In 2006 Samuel et al. presented a unique common trunk for the branches of the third part of the AA, as well as the RCA, MCA, and the superior ulnar collateral artery [7]. They reported the absence of a DBA and stated that all its relevant branches came from the common trunk. The medial cord contribution was reported to travel posterior to the AA to join the lateral cord contribution of the median nerve, surrounding the common trunk. There was no discussion of the inferior ulnar collateral artery. In 2007, George et al. described a unilateral trunk arising from the AA that contained all three branches of the third part of the AA, as well as the DBA [8]. The median nerve is described to have formed posterior to the AA, and the lateral and medial cord contributions circumscribed the common trunk. In contrast to the current report, George et al. also noted a unique double axillary vein and report that the median nerve communicated with both the radial and musculocutaneous nerves in the arm. Ramesh Rao et al. discussed a cadaveric case of a common arterial trunk involving the third part of the axillary artery and the deep brachial artery like ours [9]. The common trunk described traveled b/etween the medial and lateral cord contributions of the median nerve to give all three branches of the third part of the AA and the DBA. In contrast to the current report, the common trunk then continued as the superior and inferior ulnar collateral arteries, which is typically seen arising from the BA. In 2014 Naveen et al. described a common arterial trunk very similar to ours, which contained all branches of the third part of the AA and continued as the DBA [10]. The median nerve formed posteriorly to the AA, circumscribing the common trunk. In addition to a unique variation of the superior thoracic artery, Aastha et al. presented, in 2015, a unilateral common trunk for all three branches of the AA that continued as the DBA [6]. In their case report, the median nerve contributions again formed posteriorly to the AA, circumscribing the common trunk. They also discussed collateral circulation of the medial elbow, noting that the superior ulnar collateral artery and the inferior ulnar collateral artery arose from the DBA instead of the BA. Any variation in the collateral circulation around the elbow was not addressed in any of the above studies.
In summary, the current report presents a comprehensive description the common trunk for the third part of the AA and its relevance to collateral circulation of the elbow. This adds detail to previous reports of this kind of common trunk, with description of the collateral circulation of the elbow. Moreover, our report delves into both the embryological and clinical significance of these findings, further buttressing the significance.
Embryological Significance
Considering these findings through an embryological lens provides an interesting perspective on these variations. Typically, the medial cord contribution of the median nerve travels anterior to the AA to join the lateral cord contribution and form the median nerve. However, in the current study, as well as the five other reports of this type of common arterial trunk [6-10], the medial and lateral cord contributions travel posterior to the AA to form the median nerve. This raises the question: What embryological structures and processes drive the development of the median nerve in this way?
It is understood that anatomical neurovascular variation of the arm is the result of differing embryological development of vascular and neural networks of the upper limb bud. Here, embryological development is the result of specific expression of morphogens that drive the axonal, vascular, and mesenchymal growth of the upper limb bud. Neural development of the upper limb bud is the result of elaborately coordinated, location specific interactions between the growing axons and paraxial mesoderm beginning around week 5 of development [11,12]. Occurring simultaneously with neural development of the upper limb bud, the arterial system of the upper limb begins to develop [13]. The AA branching anomalies often arise from the persistence of arteries from the capillary plexus of the upper limb bud that would normally regress [14-16]. Given the proximity in time and location of these two systems developing in the upper limb bud, it is reasonable to postulate that changes in circulatory factors during differentiation of the brachial plexus could alter the development of the median nerve [17].
We propose that the unusual proximal emergence of the DBA from the common trunk of the AA encouraged the median nerve to develop posterior to the AA, thereby circumscribing the common trunk containing the DBA. This hypothesis is founded on the consistent findings between the current, and the other, studies of this unique trunk [6-10], as well as literature citing variations in DBA in association with median nerve development [18]. This hypothesis is also derived from case reports stating that common trunks in the third part of the AA without the DBA show no such unusual development of the median nerve [19,20]. Future studies could aim to investigate this hypothesis, as it would contribute to our knowledge of embryological development.
Clinical Significance
The variations described in this case should be considered during surgical procedures involving the arm and axilla. Specifically, in the setting of iliofemoral arterial occlusive or aortic disease, such as acute ascending aortic dissection, ascending aortic aneurysm or coronary artery bypass grafting, cardiovascular surgeons may use the AA for providing arterial inflow during cardiopulmonary bypass [21]. Moreover, knowledge of variations in the AA is crucial for accurate interpretation of diagnostic procedures and subsequent planning of invasive vascular surgeries.
The observations of the medial cord contribution of the median nerve passing between the AA and the common trunk, and the lateral cord contribution of the medial nerve between the AA and common stem, provide a relationship that could allow the median nerve to be susceptible to compression. Inversely, the fact that a significant arterial trunk passes from the AA through the roots of the median nerve increases the susceptibility of arterial compression. Thus, knowledge of this type of neurovascular anomaly is for quite relevant for clinicians.
Finally, a surgical neck fracture of the humerus is an important consideration when discussing these variations. The PHCA is prone to damage following a surgical neck fracture [22]. In the setting of the vascular anomaly we present, a humeral surgical neck fracture could injure the PHCA, thereby altering collateral circulation around the elbow. Again, this example demonstrates the necessity that clinicians, like orthopedic surgeons and radiologists, be knowledgeable of variations of the AA.
Conclusion
We present a unique, unilateral common trunk for the third part of the axillary artery and the deep brachial artery. Radial collateral circulation of the elbow was also altered in this anomaly, as was the normal course of the median nerve. These rare findings have both embryological and clinical significance.
Acknowledgement
We would like to thank the individuals, and family members, of those who choose to donate their bodies for the purpose of educating those in the medical community. We would also like to thank the Gift Body Program of the Center for Anatomical Science and Education, Department of Surgery at Saint Louis University School of Medicine.
REFERENCES
- Olinger A, Benninger B. Branching patterns of the lateral thoracic, subscapular, and posterior circumflex humeral arteries and their relationship to the posterior cord of the brachial plexus. Clin Anat. 2010;23:407-12.
- Sharma T, Singla RK, Sachdeva K. Bilateral superficial brachial artery. Kathmandu Univ Med J (KUMJ). 2009;7:426-8.
- Baral P, Vijayabhaskar P, Roy S, et al. Multiple arterial anomalies in upper limb. Kathmandu Univ Med J (KUMJ). 2009;7:293-7.
- Vijaya Bhaskar P, Ritesh R, Shankar PR. Anomalous branching of the axillary artery: a case report. Kathmandu Univ Med J (KUMJ). 2006;4:517-9.
- Sawant SP, Shaikh ST, More RM. Variant axillary artery -A case report. IJCRR. 2012;4:102-8.
- Aastha, Jain A, Kumar MS. An unusual variation of axillary artery: a case report. J Clin Diagn Res. 2015;9:5-7.
- Vijaya PS. A rare variation in the branching pattern of the axillary artery. Indian J Plast Surg. 2006;39:222-3.
- George BM, Nayak S, Kumar P. Clinically significant neurovascular variations in the axilla and the arm-A case report. Neuroanatomy. 2007;6.
- Ramesh RT, Prakashchandra S, Suresh R. Abnormal Branching Pattern of the Axillary Artery and its Clinical Significance. Int J Morphol. 2008;26:389-92.
- Naveen K, Jyothsna P, Nayak SB, et al. Variant origin of an arterial trunk from axillary artery continuing as profundabrachii artery--a unique arterial variation in the axilla and its clinical implications. Ethiop J Health Sci. 2014;24:93-6.
- Bennett MR, Brown MC, Hopkins WG, et al. Essentials of Neural Development. Q Rev Biol. 1992;67:233.
- Larsen W. Human Embryology. 2nd ed. 1997, Edinberg: Churchill Linvingstone.
- Rodríguez-Niedenführ M, Burton GJ, Deu J, et al. Development of the arterial pattern in the upper limb of staged human embryos: normal development and anatomic variations. J Anat. 2001;199:407-17.
- Chitra P, Anandhi V. A unique variation in branching pattern of axillary artery. IJAV. 2013;6:1-3.
- Kanaka S, Eluru RT, Basha MA, et al. Frequency of Variations in Axillary Artery Branches and its Surgical Importance. Int J Sci Study. 2015;3.
- Nakatani T, Izumi A, Tanaka S. Bilateral superficial median arteries. J Anat. 1999;194:475-7.
- Budhiraja V, Rastogi R, Asthana AK. Anatomical variation of median nerve formation: embryological and clinical correlation. J Morphol Sci. 2011;28:283-6.
- Pais D, Casal D, Santos A, et al. A variation in the origin of the median nerve associated with an unusual origin of the deep brachial artery. J Morphol Sci. 2010;27.
- Bagoji IB, Hadimani GA, Bannur BM, et al. A unique branching pattern of the axillary artery: a case report. J Clin Diagn Res. 2013;7:2939-40.
- Saeed M, Rufai AA, Elsayed SE, et al. Variations in the subclavian-axillary arterial system. Saudi Med J. 2002;23:206-212.
- Kokotsakit J, Lazopoulos G, Milonakis M, et al. Right axillary artery cannulation for surgical management of the hostile ascending aorta. TEX HEART I J, 2005;32:189-93.
- Atema JJ, Unlu C, Reekers JA, et al. Posterior circumflex humeral artery injury with distal embolisation in professional volleyball players: a discussion of three cases. Eur J Vasc Endovasc Surg. 2012;44:195-8.