A variant case of ansa cervicalis
Libor Machalek*, Jiri Charamza, Katerina Kikalova, Milada Bezdekova
Department of Normal Anatomy, Faculty of Medicine and Dentistry, Palacky University Olomouc, Czech Republic.
- *Corresponding Author:
- Libor Machalek, MD
Assistant Professor, Department of Normal Anatomy, Faculty of Medicine and Dentistry, Palacky University Olomouc, Hnevotinska 3, Olomouc 779 00, Czech Republic.
Tel: +42 585 632 206
E-mail: machlib@tunw.upol.cz
Date of Received: July 1st, 2009
Date of Accepted: November 5th, 2009
Published Online: December 24th, 2009
© IJAV. 2009; 2: 150–152.
[ft_below_content] =>Keywords
ansa cervicalis, variation, deep location
Introduction
Ansa cervicalis (ansa cervicalis profunda, ansa nervi hypoglossi) is one of the nerve connections in the human body. Two roots make up the ansa cervicalis –radix superior and radix inferior. Its sources include the ventral rami of the cervical spinal nerves; ansa innervates all infrahyoid muscles except for the thyrohyoid muscle [1,2]. In the past few years, there has been a development in the techniques using ansa cervicalis to innervate muscles of the larynx paralyzed due to surgical procedures performed in the area of the chest and neck (surgeries of esophagus, thyroid). Ansa is used during nerve anastomosis with the recurrent laryngeal nerve or, thanks to its proximity to the larynx and its activity during phonation, as a neuromuscular pedicle [3,4]. Good knowledge of topographical relationships existing in the area, including possible deviations, is one of the key prerequisites for successful surgery.
Case Report
During the dissection practice we found an unusually placed ansa cervicalis in a 68-year-old male cadaver. With standard macroanatomical dissection procedures, we clarified the location and origin of ansa cervicalis. For the purposes of photo documentation we used the digital camera NIKON D60, objective Nikon 60 mm ED AF-S.
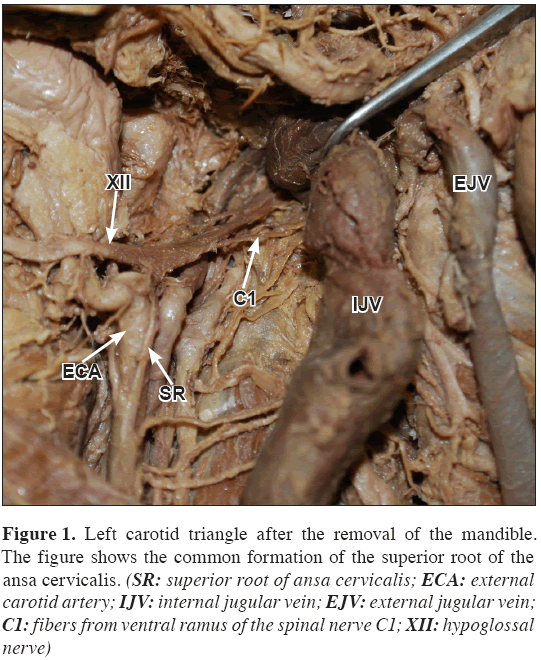
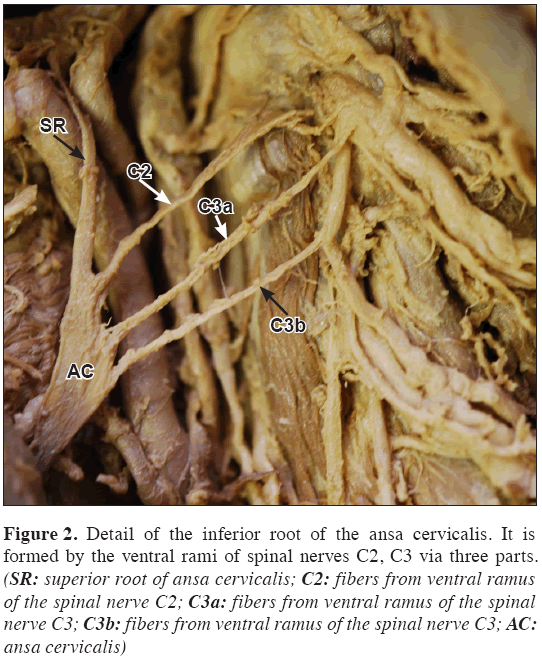
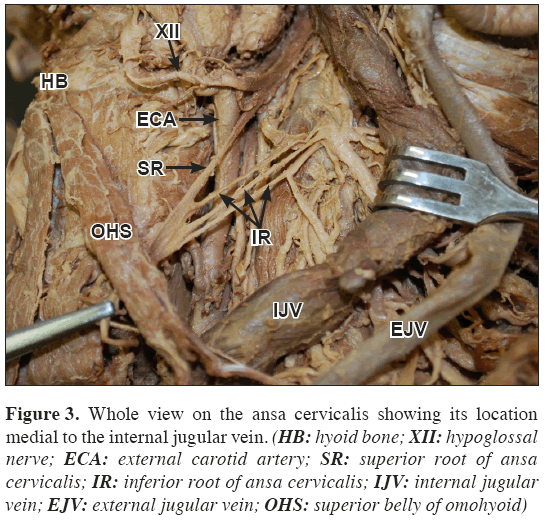
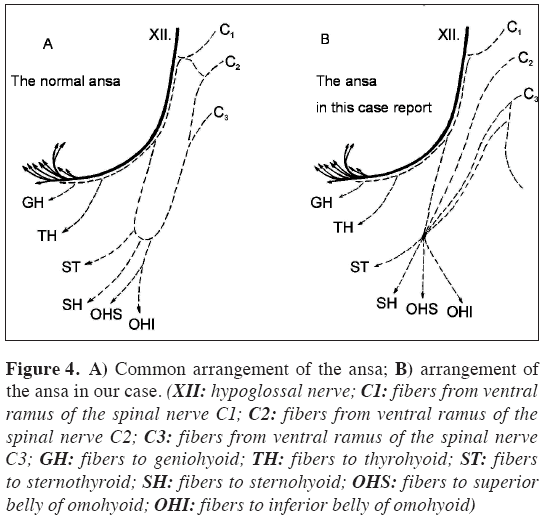
Our findings describe bilateral occurrence of a unique variation of a deep cervical loop in the cadaver (Figure 4B). As usual, the superior root of ansa cervicalis (Figure 1) originated from ventral branch of the C1 spinal nerve, joined in the hypoglossal nerve under the internal jugular vein, and when crossing the hypoglossal nerve and occipital artery it separated from the hypoglossal nerve (descending branch of hypoglossal nerve). Branches from the spinal nerves C2 - C3 (two branches stem from C3) traveled anterior to the prevertebral muscles caudally and joined the superior root, making an acute angle (Figure 2). However, this connection was, in contrast to the common form of ansa cervicalis, placed medially to the internal jugular vein, and was gradual (Figure 3). All roots were connected posterior to the carotid sheath and the produced nerve trunk ran through this sheath. The terminal branching towards the infrahyoid muscles was standard (Figure 4).
Figure 1: Left carotid triangle after the removal of the mandible. The figure shows the common formation of the superior root of the ansa cervicalis. (SR: superior root of ansa cervicalis; ECA: external carotid artery; IJV: internal jugular vein; EJV: external jugular vein; C1: fibers from ventral ramus of the spinal nerve C1; XII: hypoglossal nerve)
Figure 2: Detail of the inferior root of the ansa cervicalis. It is formed by the ventral rami of spinal nerves C2, C3 via three parts. (SR: superior root of ansa cervicalis; C2: fibers from ventral ramus of the spinal nerve C2; C3a: fibers from ventral ramus of the spinal nerve C3; C3b: fibers from ventral ramus of the spinal nerve C3; AC: ansa cervicalis)
Figure 3: Whole view on the ansa cervicalis showing its location medial to the internal jugular vein. (HB: hyoid bone; XII: hypoglossal nerve; ECA: external carotid artery; SR: superior root of ansa cervicalis; IR: inferior root of ansa cervicalis; IJV: internal jugular vein; EJV: external jugular vein; OHS: superior belly of omohyoid)
Figure 4: A) Common arrangement of the ansa; B) arrangement of the ansa in our case. (XII: hypoglossal nerve; C1: fibers from ventral ramus of the spinal nerve C1; C2: fibers from ventral ramus of the spinal nerve C2; C3: fibers from ventral ramus of the spinal nerve C3; GH: fibers to geniohyoid; TH: fibers to thyrohyoid; ST: fibers to sternothyroid; SH: fibers to sternohyoid; OHS: fibers to superior belly of omohyoid; OHI: fibers to inferior belly of omohyoid)
Discussion
The procedures to improve the phonation malfunctions caused by a loss of laryngeal muscle innervations include the vocal cords medialization procedures – thyroplasty type I, arytenoid adduction, teflon injection into vocal cords, or re-innervation procedures. In 1926, Frazeir and Mosser first described the use of anastomosis with ansa cervicalis when treating recurrent laryngeal nerve paralysis. They used the superior root of ansa cervicalis and were successful in improving the phonation at 5 out of 10 patients. Over the time, there have developed modifications of the reinnervation procedures using ansa cervicalis as the source of anastomosis with recurrent laryngeal nerve or with a part of the innervated infrahyoid muscle as the nerve-muscle pedicle [5,6]. With the improvement of recurrent laryngeal nerve monitoring during thyroid operations, the occurrence of iatrogenic damage to the aforementioned nerve decreases. It is interesting that damage to ansa cervicalis may lead to a change in the voice quality. The exact cause to this phenomenon is not known, it is probably because the infrahyoid muscles cease to support the larynx [4].
In the usual arrangement, ansa cervicalis is formed by a union of two roots – radix superior (ramus descendens nervi hypoglossi) and radix inferior. Some authors prefer the term radix anterior and posterior [7,8]. The radix superior originates from the fibers of C1 (or C2) spinal nerve, joins the hypoglossal nerve, and after nerve XII crosses the occipital artery, ansa cervicalis leaves the nerve, runs down along or inside carotid sheath, and at a variable height it connects with radix inferior. Prior to the connection, radix superior provides a branch for the superior belly of the omohyoid muscle. In 75 %, radix inferior of ansa cervicalis originates independently by the union of fibers from the C2 and C3 spinal nerves; in 15 % from the C2 - C4 spinal nerves; in 5 % only from C3; and occasionally it may originate only from C2 or C1-3. Muscular branches for the inferior belly of omohyoid, sternohyoid, and sternothyroid muscles leave from ansa. Other small branches may descend along the vessels into the chest and connect with phrenic nerve and cardiac nerves. The thyrohyoid muscle along with the geniohyoid muscle are innervated also from the C1 spinal nerves, which had joined nerve XII and leave the hypoglossal nerve directly, ventrally from the superior root [5].
The origin, location, and distribution of ansa cervicalis branches document a significant variability level. In their recent study of 100 cadavers, Loukas et al. described the following frequency of some ansa parameters. In 92 %, the origin of radix superior was superficial to the digastrics muscle; in 72 % it descended along external carotid artery and in 28 % along internal carotid artery. In 38 % of cases, radix inferior originated from the C2 and C3 primary branches, in 10 % from C2 - C4, in 40 % from C3, in 12 % from C2, and in 74 % of cases it run postero-laterally from the internal jugular vein and in 26 % antero-laterally. Seventy per cent of ansa roots were so long that they merged under the omohyoid muscle, and 30% were short, connecting above the omohyoid muscle. Most frequently, the location of ansa in relation to carotid sheath was externally from both the large vessels. In literature, there is a case of radix superior running medially from the internal jugular vein with an ansa loop between the common carotid artery and the internal jugular vein; rarely does it lay dorsally from carotid sheath [9].
Apart from the “standard” variability of origin, atypical cases of ansa origin have been described. For instance, a unilateral occurrence of “ramus descendens nervi vagi” at a 40-year-old male: fibers from the first cervical nerve did not join nerve XII, but nerve X, leaving it as the ansa superior root [3]. A similar case was a unilateral finding of a doubled ansa cervicalis in a 55-year-old male cadaver: a part of fibers from C1 connected normally to nerve XII and a smaller part of them to nerve X. The connected fibers then separated as ramus descendens nervi hypoglossi and ramus descendens nervi vagi [4]. Noteworthy is also a discovery of pseudo ansa cervicalis with the superior root rising from the superior sympathetic ganglion and the inferior root rising from the vagus nerve. Both roots connected dorsomedially from the carotid sheath. This pseudo-loop did not issue any muscle branches for infrahyoid muscles but, instead, two branches, which connected in the chest to the vagus nerve. In this case, the infrahyoid muscles innervated the branches from nerve XII and the branches coming out of the loop between C1 and C2. Fibers from C1 in the proximity of the skull base formed anastomoses with nerves X, XII and with sympathetic trunk [6]. Extraordinarily rare is also bilateral absence of ansa cervicalis and its replacement by vagocervical complex, which is formed by C1 and C2 ventral branches and from nerve X [10].
The variety we have described ranks among the irregular placement of ansa cervicalis, and we have not found statistics assessment of such occurrence in literature.
References
- Standring S. Gray’s Anatomy, The Anatomical Basic of Clinical Practice. 39th Ed., London, Elsevier Churchil Livingstone. 2005; 532.
- Williams PL. Gray’s Anatomy. 38th Ed., Edinburgh, Churchil Livingstone. 1995; 1258, 1286.
- Vollala VR, Bhat SM, Nayak S, Raghunathan D, Samuel VP, Rodrigues V, Mathew JG. A rare origin of upper root of ansa cervicalis from vagus nerve: a case report. Neuroanatomy. 2005; 4: 8–9.
- Rao TR, Shetty P, Rao SR. A rare case of formation of double ansa cervicalis. Neuroanatomy. 2007; 6: 26–27.
- Chhetri DK, Berke GS. Ansa cervicalis nerve: review of the topographic anatomy and morphology. Laryngoscope. 1997; 107: 1366–1372.
- Indrasingh I, Vettivel S. A rare pseudo ansa cervicalis: a case report. J Anat Soc India. 2000; 49: 178–179.
- Feneis H, Dauber W. Pocket Atlas of Human Anatomy Based on the International Nomenclature. 4th Ed., New York, Thieme Stuttgart. 2000; 334.
- Putz R, Pabst R. Sobotta Atlas anatomii człowieka. Wyd. II Polskie, Wrocław, Urban & Partner. 1997; 23.
- Loukas M, Thorsell A, Tubbs RS, Kapos T, Louis RG Jr, Vulis M, Hage R, Jordan R. The ansa cervicalis revisited. Folia Morphol (Warsz). 2007; 66: 120–125.
- Abu-Hijleh MF. Bilateral absence of ansa cervicalis replaced by vagocervical plexus: case report and literature review. Ann Anat. 2005; 187: 121–125.
Libor Machalek*, Jiri Charamza, Katerina Kikalova, Milada Bezdekova
Department of Normal Anatomy, Faculty of Medicine and Dentistry, Palacky University Olomouc, Czech Republic.
- *Corresponding Author:
- Libor Machalek, MD
Assistant Professor, Department of Normal Anatomy, Faculty of Medicine and Dentistry, Palacky University Olomouc, Hnevotinska 3, Olomouc 779 00, Czech Republic.
Tel: +42 585 632 206
E-mail: machlib@tunw.upol.cz
Date of Received: July 1st, 2009
Date of Accepted: November 5th, 2009
Published Online: December 24th, 2009
© IJAV. 2009; 2: 150–152.
Abstract
Ansa cervicalis is a nerve anastomosis innervating infrahyoid muscles. Due to its topographic and functional relationship to the larynx, it is used for re-innervating surgical procedures with a damaged recurring laryngeal nerve. Being familiar with the variations in terms of the origin, placement, and branching is important for surgeons. The casuistics described above concerns the location of ansa cervicalis medial to the carotid sheath.
-Keywords
ansa cervicalis, variation, deep location
Introduction
Ansa cervicalis (ansa cervicalis profunda, ansa nervi hypoglossi) is one of the nerve connections in the human body. Two roots make up the ansa cervicalis –radix superior and radix inferior. Its sources include the ventral rami of the cervical spinal nerves; ansa innervates all infrahyoid muscles except for the thyrohyoid muscle [1,2]. In the past few years, there has been a development in the techniques using ansa cervicalis to innervate muscles of the larynx paralyzed due to surgical procedures performed in the area of the chest and neck (surgeries of esophagus, thyroid). Ansa is used during nerve anastomosis with the recurrent laryngeal nerve or, thanks to its proximity to the larynx and its activity during phonation, as a neuromuscular pedicle [3,4]. Good knowledge of topographical relationships existing in the area, including possible deviations, is one of the key prerequisites for successful surgery.
Case Report
During the dissection practice we found an unusually placed ansa cervicalis in a 68-year-old male cadaver. With standard macroanatomical dissection procedures, we clarified the location and origin of ansa cervicalis. For the purposes of photo documentation we used the digital camera NIKON D60, objective Nikon 60 mm ED AF-S.
Our findings describe bilateral occurrence of a unique variation of a deep cervical loop in the cadaver (Figure 4B). As usual, the superior root of ansa cervicalis (Figure 1) originated from ventral branch of the C1 spinal nerve, joined in the hypoglossal nerve under the internal jugular vein, and when crossing the hypoglossal nerve and occipital artery it separated from the hypoglossal nerve (descending branch of hypoglossal nerve). Branches from the spinal nerves C2 - C3 (two branches stem from C3) traveled anterior to the prevertebral muscles caudally and joined the superior root, making an acute angle (Figure 2). However, this connection was, in contrast to the common form of ansa cervicalis, placed medially to the internal jugular vein, and was gradual (Figure 3). All roots were connected posterior to the carotid sheath and the produced nerve trunk ran through this sheath. The terminal branching towards the infrahyoid muscles was standard (Figure 4).
Figure 1: Left carotid triangle after the removal of the mandible. The figure shows the common formation of the superior root of the ansa cervicalis. (SR: superior root of ansa cervicalis; ECA: external carotid artery; IJV: internal jugular vein; EJV: external jugular vein; C1: fibers from ventral ramus of the spinal nerve C1; XII: hypoglossal nerve)
Figure 2: Detail of the inferior root of the ansa cervicalis. It is formed by the ventral rami of spinal nerves C2, C3 via three parts. (SR: superior root of ansa cervicalis; C2: fibers from ventral ramus of the spinal nerve C2; C3a: fibers from ventral ramus of the spinal nerve C3; C3b: fibers from ventral ramus of the spinal nerve C3; AC: ansa cervicalis)
Figure 3: Whole view on the ansa cervicalis showing its location medial to the internal jugular vein. (HB: hyoid bone; XII: hypoglossal nerve; ECA: external carotid artery; SR: superior root of ansa cervicalis; IR: inferior root of ansa cervicalis; IJV: internal jugular vein; EJV: external jugular vein; OHS: superior belly of omohyoid)
Figure 4: A) Common arrangement of the ansa; B) arrangement of the ansa in our case. (XII: hypoglossal nerve; C1: fibers from ventral ramus of the spinal nerve C1; C2: fibers from ventral ramus of the spinal nerve C2; C3: fibers from ventral ramus of the spinal nerve C3; GH: fibers to geniohyoid; TH: fibers to thyrohyoid; ST: fibers to sternothyroid; SH: fibers to sternohyoid; OHS: fibers to superior belly of omohyoid; OHI: fibers to inferior belly of omohyoid)
Discussion
The procedures to improve the phonation malfunctions caused by a loss of laryngeal muscle innervations include the vocal cords medialization procedures – thyroplasty type I, arytenoid adduction, teflon injection into vocal cords, or re-innervation procedures. In 1926, Frazeir and Mosser first described the use of anastomosis with ansa cervicalis when treating recurrent laryngeal nerve paralysis. They used the superior root of ansa cervicalis and were successful in improving the phonation at 5 out of 10 patients. Over the time, there have developed modifications of the reinnervation procedures using ansa cervicalis as the source of anastomosis with recurrent laryngeal nerve or with a part of the innervated infrahyoid muscle as the nerve-muscle pedicle [5,6]. With the improvement of recurrent laryngeal nerve monitoring during thyroid operations, the occurrence of iatrogenic damage to the aforementioned nerve decreases. It is interesting that damage to ansa cervicalis may lead to a change in the voice quality. The exact cause to this phenomenon is not known, it is probably because the infrahyoid muscles cease to support the larynx [4].
In the usual arrangement, ansa cervicalis is formed by a union of two roots – radix superior (ramus descendens nervi hypoglossi) and radix inferior. Some authors prefer the term radix anterior and posterior [7,8]. The radix superior originates from the fibers of C1 (or C2) spinal nerve, joins the hypoglossal nerve, and after nerve XII crosses the occipital artery, ansa cervicalis leaves the nerve, runs down along or inside carotid sheath, and at a variable height it connects with radix inferior. Prior to the connection, radix superior provides a branch for the superior belly of the omohyoid muscle. In 75 %, radix inferior of ansa cervicalis originates independently by the union of fibers from the C2 and C3 spinal nerves; in 15 % from the C2 - C4 spinal nerves; in 5 % only from C3; and occasionally it may originate only from C2 or C1-3. Muscular branches for the inferior belly of omohyoid, sternohyoid, and sternothyroid muscles leave from ansa. Other small branches may descend along the vessels into the chest and connect with phrenic nerve and cardiac nerves. The thyrohyoid muscle along with the geniohyoid muscle are innervated also from the C1 spinal nerves, which had joined nerve XII and leave the hypoglossal nerve directly, ventrally from the superior root [5].
The origin, location, and distribution of ansa cervicalis branches document a significant variability level. In their recent study of 100 cadavers, Loukas et al. described the following frequency of some ansa parameters. In 92 %, the origin of radix superior was superficial to the digastrics muscle; in 72 % it descended along external carotid artery and in 28 % along internal carotid artery. In 38 % of cases, radix inferior originated from the C2 and C3 primary branches, in 10 % from C2 - C4, in 40 % from C3, in 12 % from C2, and in 74 % of cases it run postero-laterally from the internal jugular vein and in 26 % antero-laterally. Seventy per cent of ansa roots were so long that they merged under the omohyoid muscle, and 30% were short, connecting above the omohyoid muscle. Most frequently, the location of ansa in relation to carotid sheath was externally from both the large vessels. In literature, there is a case of radix superior running medially from the internal jugular vein with an ansa loop between the common carotid artery and the internal jugular vein; rarely does it lay dorsally from carotid sheath [9].
Apart from the “standard” variability of origin, atypical cases of ansa origin have been described. For instance, a unilateral occurrence of “ramus descendens nervi vagi” at a 40-year-old male: fibers from the first cervical nerve did not join nerve XII, but nerve X, leaving it as the ansa superior root [3]. A similar case was a unilateral finding of a doubled ansa cervicalis in a 55-year-old male cadaver: a part of fibers from C1 connected normally to nerve XII and a smaller part of them to nerve X. The connected fibers then separated as ramus descendens nervi hypoglossi and ramus descendens nervi vagi [4]. Noteworthy is also a discovery of pseudo ansa cervicalis with the superior root rising from the superior sympathetic ganglion and the inferior root rising from the vagus nerve. Both roots connected dorsomedially from the carotid sheath. This pseudo-loop did not issue any muscle branches for infrahyoid muscles but, instead, two branches, which connected in the chest to the vagus nerve. In this case, the infrahyoid muscles innervated the branches from nerve XII and the branches coming out of the loop between C1 and C2. Fibers from C1 in the proximity of the skull base formed anastomoses with nerves X, XII and with sympathetic trunk [6]. Extraordinarily rare is also bilateral absence of ansa cervicalis and its replacement by vagocervical complex, which is formed by C1 and C2 ventral branches and from nerve X [10].
The variety we have described ranks among the irregular placement of ansa cervicalis, and we have not found statistics assessment of such occurrence in literature.
References
- Standring S. Gray’s Anatomy, The Anatomical Basic of Clinical Practice. 39th Ed., London, Elsevier Churchil Livingstone. 2005; 532.
- Williams PL. Gray’s Anatomy. 38th Ed., Edinburgh, Churchil Livingstone. 1995; 1258, 1286.
- Vollala VR, Bhat SM, Nayak S, Raghunathan D, Samuel VP, Rodrigues V, Mathew JG. A rare origin of upper root of ansa cervicalis from vagus nerve: a case report. Neuroanatomy. 2005; 4: 8–9.
- Rao TR, Shetty P, Rao SR. A rare case of formation of double ansa cervicalis. Neuroanatomy. 2007; 6: 26–27.
- Chhetri DK, Berke GS. Ansa cervicalis nerve: review of the topographic anatomy and morphology. Laryngoscope. 1997; 107: 1366–1372.
- Indrasingh I, Vettivel S. A rare pseudo ansa cervicalis: a case report. J Anat Soc India. 2000; 49: 178–179.
- Feneis H, Dauber W. Pocket Atlas of Human Anatomy Based on the International Nomenclature. 4th Ed., New York, Thieme Stuttgart. 2000; 334.
- Putz R, Pabst R. Sobotta Atlas anatomii człowieka. Wyd. II Polskie, Wrocław, Urban & Partner. 1997; 23.
- Loukas M, Thorsell A, Tubbs RS, Kapos T, Louis RG Jr, Vulis M, Hage R, Jordan R. The ansa cervicalis revisited. Folia Morphol (Warsz). 2007; 66: 120–125.
- Abu-Hijleh MF. Bilateral absence of ansa cervicalis replaced by vagocervical plexus: case report and literature review. Ann Anat. 2005; 187: 121–125.