A young adult presenting with ST elevation myocardial infarction due to a persistent spasm of proximal left descending artery: An image focus
Received: 07-Oct-2020 Accepted Date: Nov 17, 2020; Published: 24-Nov-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Coronary Artery Vasospasm (CVS) is an important mechanism of myocardial ischemia and produces any of the manifestations of coronary artery disease from silent myocardial ischemia, to effort-induced angina and variant angina, to acute coronary syndrome including myocardial infarction or sudden cardiac death. We report a case of a 28-year-old-patient, smoker, who presented with ST segment myocardial infarction (STEMI). Coronary angiography revealed a persistent spasm in proximal segment of left descending artery resolved after injecting intracoronary nitroglycerine. Intra and extra-hospital outcome were favorable.Keywords
Young adult; STEMI; Coronary spasm; Nitroglycerine
Introduction
Coronary artery vasospasm (CVS) is an important mechanism of myocardial ischemia and produces any of the manifestations of coronary artery disease from silent myocardial ischemia, to effort-induced angina and variant angina, to acute coronary syndrome including myocardial infarction or sudden cardiac death. We report a case of a 28 year-old-patient, smoker, who presented with ST segment myocardial infarction (STEMI) immediately after cigarette smoking. In this article, we elucidate our clinical case in which coronary angiography, revealed a persistent coronary vasospasm 24 hours after patient’s admission, with a spasm relief after intracoronary injection of nitroglycerine.
Case Report
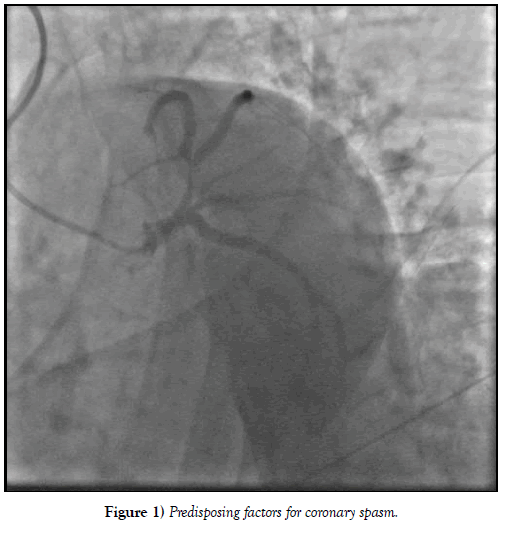
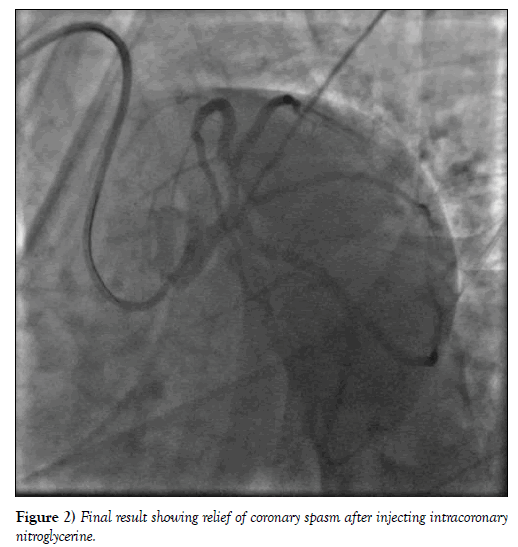
A 28-year-old patient, smoker, with no familial or personal history of heart disease, presented to the emergency room with an acute coronary syndrome immediately after cigarette smoking. At his admission, on 7 hours from chest pain onset, the patient was hemodynamicaly stable, physical examination showed no sign of complication. Electrocardiogram revealed ST segment elevation in anterior leads with Q wave in antero septal leads and negative T waves in lateral leads. Transthoracic echocardiography showed a normal left ventricular ejection fraction of 60% with apical hypokinesia and alteration of global longitudinal strain at -12% and segmental longitudinal strain (severe alteration at the apex, apical segments of anterior and septal wall, mid and basal segments of anteroseptal wall and mild alteration of mid and basal segments of inferior wall). Biological analysis showed an elevated white cells amount of 26800 elements/mm3, a mild cytolysis with GOT à 778 UI/L, GPT at 137 UI/L. Highly sensitive C-reactive protein, renal function and lipid profile were normal. Viral serologies testing including HIV, syphilis, hepatitis virus (B and C), EBV and CMV were negative. Coronary angiography, performed 24 hours after, revealed a persistent coronary spasm localized to proximal segment of left descending artery with normal coronary arteries and no sign of atherosclerosis (Figure 1). We used intracoronary injection of nitroglycerine and the result was remarkable (Figure 2). Our patient was discharged on verapamil treatment. Extra-hospital outcome was favourable especially after smoking cessation and no angina recurrence was noted during two years of follow-up.
Discussion
Coronary spasm, also known as variant or Printzmetal’s angina, represents a syndrome characterised by sudden chest pain due to epicardial coronary artery spasm which usually leads to transient myocardial ischemia, with chest pain and ECG changes. It differs from traditional stable angina pectoris, symptomatically in that it is not directly related to effort and pathologically as it is not driven by atherosclerosis and lumen encroachment within the coronary vasculature (Table 1) [1].
TABLE 1 Common differences between coronary spasm and chronic coronary angina.
| Variables | Coronary spasm | Chronic stable angina | |
|---|---|---|---|
| Frequency | Less | More frequent | |
| Age | Younger | Older | |
| Sex | Female | Male | |
| Ethnicity | Japanese | No specific prevalence | |
| Risk factors | Smoking, drug addiction, alcohol, hyperventilation, beta blockers | Classic cardiovascular risk factor | |
| Circadian pattern | Night-early morning | No | |
| Exertion/Rest | Exertion/ rest | Exertion | |
| ECG | ST segment elevation | ST segment depression | |
The actual prevalence of the condition in the general population remains largely unknown, primarily due to challenges in diagnosis. However, in contrast to traditional angina pectoris, it appears to be less frequent, afflicts younger patients and females more than males [2,3].
Coronary spasm is also associated with smoking, cocaine, amphetamine, marijuana and alcohol consumption, which can often explain myocardial infarction in young patients with few traditional cardiovascular risk factors.
Notably, chemotherapy and anti-migraine drugs may also induce coronary spasm and cautions are listed for these agents (Table 2) [4,5].
TABLE 2 Recognized predisposing factors for coronary spasm.
| Predisposing factors for coronary spasm |
| Alcohol (especially alcohol withdrawal ) |
| Emotional stress |
| Exposure to cold |
| Vasoconstrictor agents (e.g. beta blockers, anti-migraine drugs) |
| Stimulant drugs (e.g. amphetamines and cocaine) |
| Chemotherapy |
Patients with chest pain, ECG ST segments elevation and normal coronary arteries are usually considered to be affected by spasm if the clinical scenario is consistent with the characteristics of coronary spasm [6]. Myocardial infarction can develop if the spasm and ischemia are sufficiently prolonged to induce myocyte death. Following an acute presentation as described, patients are usually discharged on a medication with anti-spasm properties, along with any other therapies for co-existent atherosclerosis or LV impairment, lifestyle modification advice and subsequent re-evaluation in clinic. If full control of symptoms has been achieved, no further investigations are pursued at this stage.
Pharmacological interventions (long-acting calcium antagonists, long-acting nitrates, nicorandil, magnesium, antioxidants…) have the potential to reduce or prevent spasm attacks, symptoms and life-treating arrhythmias. Aside from compliance with treatment, identification and avoidance of precipitants are an essential component of any management plan. In this regard it is essential to advise patients to quit smoking. Despite a wide consensus on the role of nitrates and calcium channel antagonist, in treating patients with coronary spasm, there remain uncertainties about how to best manage these patients, from which agent to use through to when to consider the use of ICD for primary prevention. Prospective double-blind studies with calcium channel antagonists compared with nitrates have reported efficacy for both agents to a similar degree, in reducing spasm occurrence [7].
Conclusion
Our case shows a persistent coronary vasospasm leading to myocardial infarction presentation. Smoking alone can be responsible of coronary vasospasm. Along with medical treatment, changing lifestyle and avoiding known precipitating factors are very important to prevent spasm recurrence.
Conflict of Interest
The authors declare that they have no conflict of interest.
REFERENCES
- Slavich M, Patel RS. Coronary artery spasm: Current knowledge and residual uncertainties. IJC Heart & Vasculature. 2016;10:47-53.
- Prinzmetal M, Kennamer R, Merliss R, et al. A variant form of angina pectoris: A preliminary report. Am J Med. 1959;27(3):375-88.
- Yasue H, Nakagawa H, Itoh T, et al. Coronary artery spasm—clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008;51(1):2-17.
- Lanza GA, Careri G, Crea F. Mechanisms of coronary artery spasm. Circulation. 2011;124(16):1774-82.
- Sestito A, Sgueglia GA, Pozzo C, et al. Coronary artery spasm induced by capecitabine. J Cardio Med. 2006;7(2):136-8.
- JCS Joint Working Group, Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008): digest version. Circ J. 2010;74:1745-62.
- Hung MJ, Cherng WJ, Cheng CW, et al. Effect of antispastic agents (calcium antagonists and/or isosorbide dinitrate) on high-sensitivity C-reactive protein in patients with coronary vasospastic angina pectoris and no hemodynamically significant coronary artery disease. Am J Cardiol. 2005;95(1):84-7.