Abducens nucleus projections: A literature review with case report
Received: 04-Apr-2020 Accepted Date: Jul 08, 2020; Published: 15-Jul-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Although neuroanatomical variants are rare, we acknowledge that variants account for different clinical presentations. These variants may be pathological, a new normal or a true variant, and clinical presentations should continue encouraging us to improve our understanding of neuroanatomy.
Keywords
Abducens; Fascicular; Nucleus; Neuroanatomy; Palsy.
Introduction
Our literature search of the terms “abducens” “nucleus” “anatomy” returned 465 results through PubMed database. Of these, only English articles identifying human participants, with full-text access were selected, yielding 56 results. These manuscripts were analysed for their discussion of the abducens nuclear projections, and only eleven of those relevant to the anatomy of abducens projection are discussed below. Physiologic variants in the course of the abducens nerve have been described previously, though no analysis of the anatomic variation of the projection angle of the human abducens nucleus was found in this literature search [1-10].
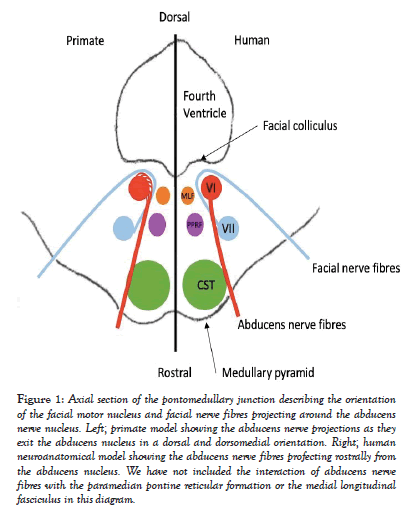
The abducens nucleus lies ventral to the floor of the fourth ventricle in the dorsal pons, lateral to the medial longitudinal fasciculus (Figure 1) [1,5]. Along with the oculomotor and trochlear nuclei and nerves, it projects motor fibres to the extraocular muscles of the eye [2]. Approximately forty percent of projection fibres from the abducens nucleus travel through the contralateral medial longitudinal fasciculus to the corresponding medial rectus subnucleus, oculomotor complex and medial rectus muscle [5,8].
Figure 1: Axial section of the pontomedullary junction describing the orientation of the facial motor nucleus and facial nerve fibres projecting around the abducens nerve nucleus. Left; primate model showing the abducens nerve projections as they exit the abducens nucleus in a dorsal and dorsomedial orientation. Right; human neuroanatomical model showing the abducens nerve fibres profecting rostrally from the abducens nucleus. We have not included the interaction of abducens nerve fibres with the paramedian pontine reticular formation or the medial longitudinal fasciculus in this diagram.
The remaining sixty percent of fibres continue ipsilaterally from the abducens nucleus to the lateral rectus muscle [5,8]. It has been suggested that these fibres originate from the abducens nucleus and move superiorly and then rostrally. From here they course rostrally through the brainstem to exit at the pontomedullary junction medially to the facial and vestibulocochlear nerves [5]. Along this pathway, the abducens nerve interacts with the paramedian pontine reticular formation [1]. The remaining intra- and extra-cranial course of the abducens nerve will not be discussed further.
Current representations of the abducens nucleus show fascicular projections coursing anteriorly to exit the rostral brainstem, however this information is not depicted in histological slides of the abducens nucleus and nerve [1,5,11]. The posterior surface of the abducens nucleus is histologically described as being enveloped in the facial nerve fibres [8].
By this description, lesions of the dorsal brainstem or floor of the fourth ventricle are unlikely to impact the abducens nerve without also involving both the facial nerve and underlying abducens nucleus.
This academic discussion followed a patient who presented to our institution with clinical signs that were not consistent with our understanding of current neuroanatomy. Below, we describe what may be an anatomical variant with splaying of the abducens nuclear fascicles dorsally and dorsomedially as they course medially around the abducens nucleus on a rostral course (Figure 1).
Case Report
An otherwise healthy twenty-five-year-old male presented for follow-up of a left dorsal pontomedullary CM that was resected in 2014 and 2017, with an associated and preserved transverse medullary developmental venous anomaly (DVA). The current problems are residual left facial weakness, left fascicular abducens palsy, and right upper limb paresthesia.
The patient has a well-documented history of a CM that was initially diagnosed after an acute left facial weakness when the patient was 12 years old. The CM size was 11mm * 8mm * 7mm in size, abutting the floor of the fourth ventricle, and hemorrhage was confirmed by MRI at the time. A conservative, non-surgical approach was followed, with unremarkable resolution of symptoms over the course of three months. Three more events of similar symptomatic resolution with stable CM size were experienced and radiologically documented over the following eight years.
In 2014, nine years after the first hemorrhagic insult, the patient experienced two radiologically confirmed bleeds within one week. Stereotactic suboccipital craniotomy for gross macroscopic resection of the CM and surrounding haematoma was completed without complication. The associated DVA was preserved. There was a post-operative eight-and-a-half-syndrome (one-and-ahalf syndrome with facial nerve palsy) [12]. The eight-and-a-half syndrome resolved within five days to a classic left fascicular abducens palsy [12]. The left abducens fascicular and LMN facial nerve palsies persisted beyond two years from surgery. In 2016, the patient underwent a left medial rectus recession and lateral rectus resection to improve an esotropia and abduction deficit of the left eye.
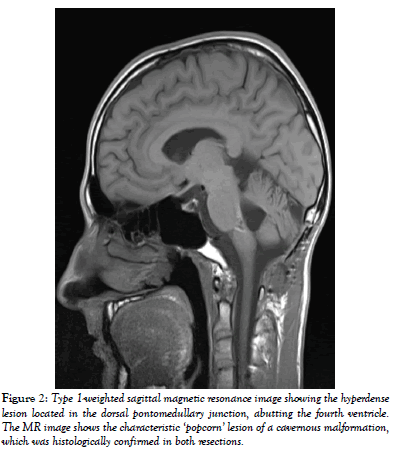
In 2017, the patient experienced acute worsening of the existing left LMN facial weakness and new onset right dorsal forearm paraesthesia. Recurrence of a CM measuring 12mm * 8mm * 9mm with surrounding hemorrhage was confirmed on MRI (Figures 2 and 3). A conservative approach was followed again. Four months later, another hemorrhage was radiologically confirmed and a repeat stereotactic suboccipital craniotomy was completed without complication.
Figure 2: Type 1-weighted sagittal magnetic resonance image showing the hyperdense lesion located in the dorsal pontomedullary junction, abutting the fourth ventricle. The MR image shows the characteristic ‘popcorn’ lesion of a cavernous malformation, which was histologically confirmed in both resections.
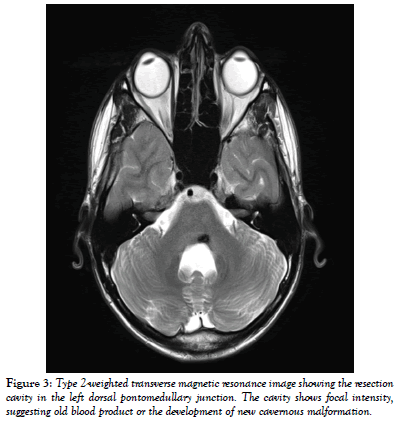
Figure 3: Type 2-weighted transverse magnetic resonance image showing the resection cavity in the left dorsal pontomedullary junction. The cavity shows focal intensity, suggesting old blood product or the development of new cavernous malformation.
Following the second surgery, the patient again experienced transient eightand- a-half syndrome, that progressed to a left abducens fascicular palsy, complete left lower motor neuron facial palsy and significant right upper limb paraesthesia. Since the second neurosurgical intervention, the patient has experienced two symptomatic events, and currently the left esotropia is managed with a Fresnel prism.
Discussion
Variant Anatomy
A fascicular abducens palsy is an inability to abduct the ipsilateral eye, resulting in an esotropia [13]. This patient presents with known left LMN facial palsy and progressive esotropia secondary to surgical resection of a pontomedullary CM with an associated transverse medullary DVA.
The lesion impacts on the location where the facial colliculus is, as shown on MRI (Figure 3) and according to anatomical conventions should compress the left abducens nucleus. In our patient, this should present as a left lateral rectus and ipsilateral conjugate gaze palsy, accompanied by an ipsilateral LMN facial nerve palsy. Alternatively, if the medial longitudinal fasciculus was also affected, this constellation of anatomical regions (ipsilateral medial longitudinal fasciculus and the facial colliculus) would cause an eight-anda- half syndrome [12,14]. Thus, we find the clinical manifestations of our patient puzzling.
Our current understanding of neuroanatomy is that the floor of the fourth ventricle borders the facial colliculus, which houses the facial nerve fibres [12]. Immediately rostral to the facial colliculus are the abducens nucleus and fascicular projections of the ipsilateral abducens nerve [2]. Based on the location of this patients lesion, the abducens nerve projections should not be affected without nuclear involvement. By this understanding, the clinical manifestations of our patient should not be limited to a left fascicular abducens palsy, rather include an ipsilateral conjugate gaze palsy.
While several explanations for this situation exist including incomplete understanding of neuroanatomy, it is most likely that the patient has deviant anatomy secondary to the DVA and CM. In light of the results of our literature review, we turned to evolutionary anatomy to assist in furthering our current understanding.
Evolutionary Development of the Abducens Nucleus
The central nervous system continues to develop well into the third decade of life. It is possible that this patient’s pathologies were congenital or present from early childhood, resulting in abnormal anatomical but normal physiological development of surrounding structures. This hypothesis of a congenital anatomical variant will remain unproven as a longitudinal study from birth is impractical, and we turn now to an academic discussion of evolutionary anatomy.
Primary embryology resources provide no explanation for the axial rotation of the brainstem accounting for the orientation of the fibres of the abducens and facial nerves [15,16]. While longitudinal rotation and in-folding of the neural plate and tube is well documented, it will not be discussed in more detail. The anatomical placement of the abducens nucleus, facial nerve fibres, and medial longitudinal fasciculus are almost identical in primate and human models [2,11]. However, primate fascicular projections of the abducens nucleus branch rostromedially (as opposed to rostrosuperiorly in humans), with projections deviating from the nucleus from dorsomedial, medial and rostro-medial locations [2]. Portions of these fibres exiting the abducens nucleus are in close proximity to the facial nerve fibres of the facial colliculus.
Embryologically, this is supported by the notion of the basal plate rotating medially throughout brainstem development, with subsequent alar and basal plate migration dorso-laterally [7]. This allows both the facial and abducens nerve projections to exit the brainstem from their rostral locations [7].
Conclusion
This primate model of abducens and facial nerve fibre arrangement may contribute to our understanding of this patient’s clinical presentation. While this patient may be an anomaly, they presented an interesting case and provided an opportunity to revisit our understanding of neuroanatomy. This case highlights the importance of recognizing collections of clinical signs to assist in isolation of brainstem lesions.
REFERENCES
- Azarmina M, Azarmina H. The six syndromes of the sixth cranial nerve. J Ophthalmic Vis Res. 2013;8:160.
- Büttner-Ennever J. The extraocular motor nuclei: organization and functional neuroanatomy. Prog Brain Res. 2006;151:95-125.
- Doepp F, Schreiber SJ, von Münster T, et al. How does the blood leave the brain? A systematic ultrasound analysis of cerebral venous drainage patterns. Neuroradiol. 2004;46:565-70.
- Moster ML, Savino PJ, Sergott RC, et al. Isolated sixth-nerve palsies in younger adults. Arch Ophthalmol. 1984;102:1328-30.
- Nguyen VD, SC. Neuroanatomy, Cranial Nerve 6, Abducens (CN VI, Abducent) 2017.
- Ohue S, Fukushima T, Kumon Y, et al. Surgical management of brainstem cavernomas: selection of approaches and microsurgical techniques. Neurosurg Rev. 2010;33:315-24.
- Pansky B. Review of medical embryology. Macmillan New York: Macmillan; 1982.
- Park HS, Chung MS, Shin DS, et al. Whole courses of the oculomotor, trochlear, and abducens nerves, identified in sectioned images and surface models. Anat Rec. 2015;298:436-43.
- Patel SV, Holmes JM, Hodge DO, et al. Diabetes and hypertension in isolated sixth nerve palsy: a population-based study. Ophthalmol. 2005;112:760-3.
- Tillack TW, Winer JA. Anomaly of the abducens nerve. Yale J Biol Med. 1962;34:620.
- Büttner-Ennever J, Akert K. Medial rectus subgroups of the oculomotor nucleus and their abducens internuclear input in the monkey. J Comp Neurol. 1981;197:17-27.
- Yadegari S, Aghsaei-Fard M, Akbari M, et al. "Eight and a half" and "nine syndrome" rare presentation of pontine lesions; case reports and review of literature. Iran J Neurol. 2018;17:189.
- Graham CM, Michael. Abducens Nerve (CN VI) Palsy. NCBI. 2019.
- Xia N-g, Chen Y-y, Li J, et al. Eight-and-a-half syndrome caused by a pontine haemorrhage: a case report and review of the literature. Int J Neurosci. 2018;128:746-50.
- Andreatta RD. neuroanatomy of the Human nervous System: Anatomical nomenclature, embryology, the Spinal Cord, and the Brainstem. NSCSD. 2018;85.
- Sadler TW. Langman's medical embryology: Lippincott Williams & Wilkins; 2011.