Absence of musculocutaneous nerve in the left axilla
Rajendrakumar D. Virupaxi*, Veereshkumar S. Shirol, Suresh P. Desai and Mathad V. Ravishankar
Department of Anatomy, Jawaharlal Nehru Medical College, KLE University, Belgaum, Karnataka State, India.
- *Corresponding Author:
- Dr. Rajendrakumar D. Virupaxi
Associate Professor, Department of Anatomy, Jawaharlal Nehru Medical College, KLE University, Belgaum – 590 010, Karnataka State, India
Tel: +91-94491-40591
E-mail: virupaxi@yahoo.co.in
Date of Received: June 25th, 2009
Date of Accepted: October 21st, 2009
Published Online: November 13th, 2009
© IJAV. 2009; 2: 140–142.
[ft_below_content] =>Keywords
brachial plexus, musculocutaneous nerve, median nerve, axilla
Introduction
Brachial plexus is formed by ventral divisions of cervical 5, 6, 7, 8 and thoracic 1 segment of spinal cord roots. These roots then divide into trunks as upper, middle and lower. Ventral divisions of upper and middle trunks form lateral cord and ventral division of lower trunk form medial cord. Posterior divisions of all trunks form posterior cord. These cords give rise to different branches. Lateral cord gives rise to first, lateral pectoral nerve that supplies the pectoralis major. Then this cord divides into musculocutaneous nerve and lateral root of median nerve. The musculocutaneous nerve (cervical 5, 6 and 7 roots) pierces the coracobrachialis muscle and then passes obliquely down to the lateral side of the arm, between biceps brachii and brachialis muscles. Then it pierces the deep fascia lateral to the tendon of biceps brachii near elbow and is continued as the lateral cutaneous nerve of the forearm. It supplies coracobrachialis, biceps brachii and brachialis in its course. First a branch is given to corachobrachialis, then to biceps and brachialis.
The median nerve is formed by (C5 to T1 roots) anterior or anterolateral to the third part of axillary artery by the union of its medial root from medial cord and lateral root from the lateral cord of brachial plexus. The median nerve crosses from lateral to medial side at the level of insertion of coracobrachialis. It descends in the cubital fossa posterior to the bicipital aponeurosis and anterior to the brachialis muscle.
Variations in origin, divisions and branches of brachial plexus in relation to subclavian and axillary arteries were reported by several authors [1–8].
Case Report
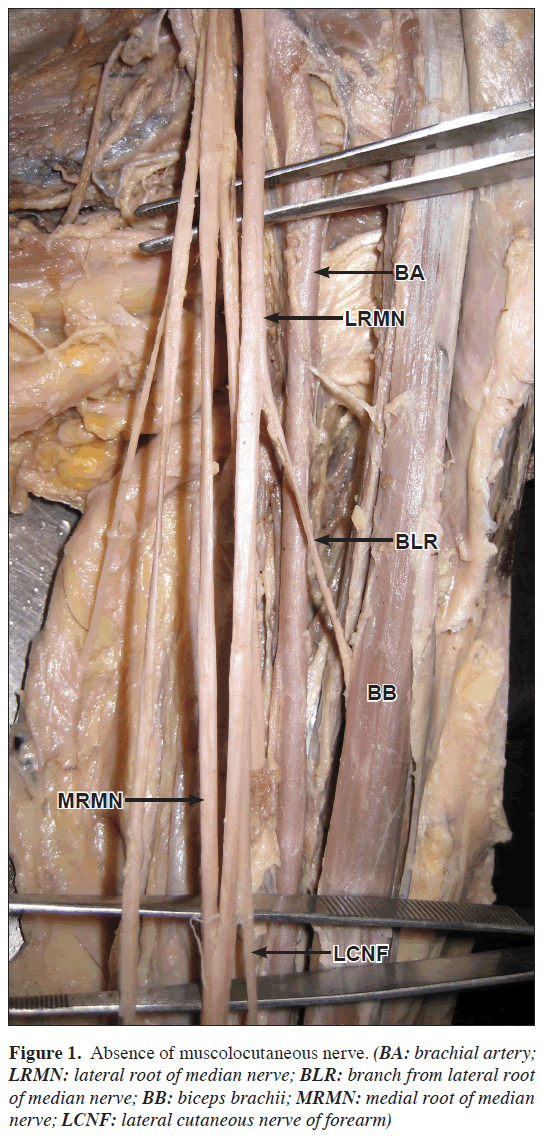
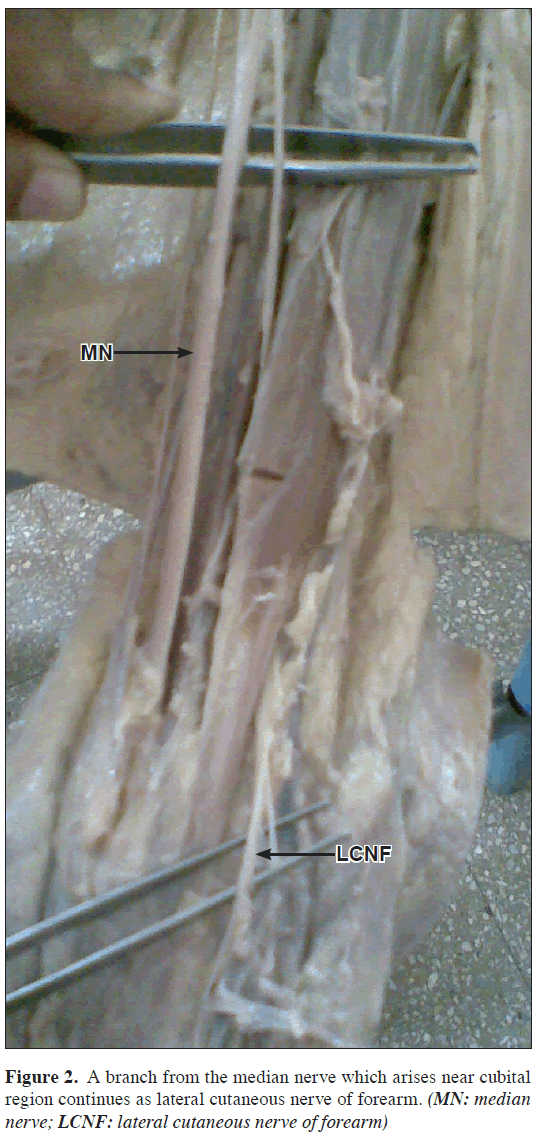
During routine dissection of the axilla and arm regions of 40-year-old male Indian cadaver in the Department of Anatomy Jawaharlal Nehru Medical College attached to KLES University Belgaum, Karnataka State India, it is observed in the infraclavicular part of brachial plexus that the musculocutaneous nerve was absent in the left axilla and arm (Figure 1). A branch from median nerve supplied the coracobrachialis muscle. This branch was higher in origin. Other branch, which was lower in origin, supplied the biceps brachii (Nerve to muscle biceps brachii). In the lower part a branch arising from the median nerve in the cubital fossa continued as lateral cutaneous nerve of forearm (Figure 2).
In the right axilla and arm the course and origin of musculocutaneous nerve was as usual.
Discussion
Musculocutenaous nerve arises from the lateral cord (cervical 5 to 7 roots) opposite the lower border of pectoralis minor. It pierces the coracobrachialis and descends laterally between biceps and brachialis to the lateral side of the arm. Variations may be frequent. It may run behind the coracobrachilalis muscle or adhere for some distance to the median nerve and pass behind the biceps or may be accompanied by fibers from the median nerve as it transits coracobrachialis [9,10]. Less frequently median nerve may send a branch to musculocutaneous nerve.
During shoulder surgery it is important to identify or palpate the musculocutaneous nerve, as it is vulnerable to injury from retractors placed under the coracoid process. During coracoid process grafting, shoulder dislocation and frequent arthroscopies may damage the muscle as well as the nerve [11]. The lesion of the musculocutaneous nerve leads to weakness of elbow flexion because biceps and coracobrachialis are paralyzed and sensory impairment on the extensor aspect of the forearm in the distribution of the lateral cutaneous nerve of forearm. Pain and parasthesia may be aggravated by elbow extension.
Brachial plexus injuries may occur following trauma, traction, compression of nerves and shoulder dislocation during traumatic delivery in infants and malposition of the patient during anesthesia [12]. This result in complete or partial palsy of the musculature innervated. Via nerve grafting recovery can be achieved. The priority of the restoration of function is also an important consideration. Elbow flexion should be given first priority followed by wrist extension, finger flexion and shoulder abduction in the order [13].
The knowledge of the variations of the course and distribution of the lateral cord of brachial plexus is important while performing neurotization of brachial plexus lesions, shoulder arthroscopy by anterior glenohumeral portal and shoulder reconstructive surgery so that these structures can be identified and protected.
References
- Abhaya A, Khanna J, Prakash R. Variation of the lateral cord of brachial plexus piercing coracobrachialis muscle. J Anat Soc India. 2003; 52: 168–170.
- Linell EA. The distribution of nerves in the upper limb, with reference to varaibilities and their clinical significance. J Anat. 1921; 55: 79–112.
- Miller RA. Comparative studies upon the morphology and distribution of the brachial plexus. Am J Anat. 1934; 54: 143–147.
- Iwamoto S, Kimura K, Takahashi Y, Konishi M. Some aspects of the communicating branch between the musculocutaneous and median nerves in man. Okajimas Folia Anat Jpn. 1990; 67: 47–52.
- Nakatani, Tanaka S, Mizukami S. Absence of the musculocutaneous nerve with innervation of coracobrachialis, biceps brachii, brachialis and the lateral border of the forearm by branches from the lateral cord of the brachial plexus. J Anat. 1997; 191: 459–460.
- Sud M, Sharma A. Absence of musulocutaneous nerve and the innervations of coracobrachialis, biceps brachii and brachialis from the median nerve. J Anat Soc India. 2000; 49: 176–177.
- Chauhan, R, Roy TS. Communication between the median and musculocutaneous nerve – a case report. J Anat Soc India. 2002; 51: 72–75.
- Abhaya A, Khanna J, Prakash R. Variation of the lateral cord of brachial plexus piercing coracobrachialis muscle. J Anat Soc India. 2003; 52: 168–170.
- Kaus M, Wotowicz Z. Communicating branch between the musculocutaneous and median nerves in human. Folia Morphol (Warsz) 1995, 54: 273–277.
- Kabak S, Ekinci N, Halici M, Karaoglu S, Unur E, Ulger H. Formation variations of median nerve. Joint Dis Relat Surg. 2001; 12: 183–185.
- Flatow EL, Bigliani LU, April EW. An anatomic study of the musculocutaneous nerve and its relationship to the coracoid process. Clin Orthop Relat Res. 1989; 244: 166–171.
- Cooper DE, Jenkins RS, Bready L, Rockwood CA Jr. The prevention of injuries of the brachial plexus secondary to malposition of the patient during surgery. Clin Orthop Relat Res. 1988; 228: 33–41.
- Sedel L. Repair of severe traction lesions of the brachial plexus. Clin Orthop Relat Res. 1988; 237: 62–66.
Rajendrakumar D. Virupaxi*, Veereshkumar S. Shirol, Suresh P. Desai and Mathad V. Ravishankar
Department of Anatomy, Jawaharlal Nehru Medical College, KLE University, Belgaum, Karnataka State, India.
- *Corresponding Author:
- Dr. Rajendrakumar D. Virupaxi
Associate Professor, Department of Anatomy, Jawaharlal Nehru Medical College, KLE University, Belgaum – 590 010, Karnataka State, India
Tel: +91-94491-40591
E-mail: virupaxi@yahoo.co.in
Date of Received: June 25th, 2009
Date of Accepted: October 21st, 2009
Published Online: November 13th, 2009
© IJAV. 2009; 2: 140–142.
Abstract
Variations of the arrangement and distribution of the lateral cord and its branches in the infraclavicular part of the brachial plexus are common in one or both axillae. These variations are important to the surgeons, neurologists, anesthetists and anatomists during surgery and dissection in the region of axilla. The present case report describes the absence of musculocutaneous nerve in the infraclavicular part of left brachial plexus, observed during routine dissection of a 40-year-old male Indian cadaver. On the right side usual origin and course of musculocutaneous nerve was seen. The clinical importances of these variations are discussed.
-Keywords
brachial plexus, musculocutaneous nerve, median nerve, axilla
Introduction
Brachial plexus is formed by ventral divisions of cervical 5, 6, 7, 8 and thoracic 1 segment of spinal cord roots. These roots then divide into trunks as upper, middle and lower. Ventral divisions of upper and middle trunks form lateral cord and ventral division of lower trunk form medial cord. Posterior divisions of all trunks form posterior cord. These cords give rise to different branches. Lateral cord gives rise to first, lateral pectoral nerve that supplies the pectoralis major. Then this cord divides into musculocutaneous nerve and lateral root of median nerve. The musculocutaneous nerve (cervical 5, 6 and 7 roots) pierces the coracobrachialis muscle and then passes obliquely down to the lateral side of the arm, between biceps brachii and brachialis muscles. Then it pierces the deep fascia lateral to the tendon of biceps brachii near elbow and is continued as the lateral cutaneous nerve of the forearm. It supplies coracobrachialis, biceps brachii and brachialis in its course. First a branch is given to corachobrachialis, then to biceps and brachialis.
The median nerve is formed by (C5 to T1 roots) anterior or anterolateral to the third part of axillary artery by the union of its medial root from medial cord and lateral root from the lateral cord of brachial plexus. The median nerve crosses from lateral to medial side at the level of insertion of coracobrachialis. It descends in the cubital fossa posterior to the bicipital aponeurosis and anterior to the brachialis muscle.
Variations in origin, divisions and branches of brachial plexus in relation to subclavian and axillary arteries were reported by several authors [1–8].
Case Report
During routine dissection of the axilla and arm regions of 40-year-old male Indian cadaver in the Department of Anatomy Jawaharlal Nehru Medical College attached to KLES University Belgaum, Karnataka State India, it is observed in the infraclavicular part of brachial plexus that the musculocutaneous nerve was absent in the left axilla and arm (Figure 1). A branch from median nerve supplied the coracobrachialis muscle. This branch was higher in origin. Other branch, which was lower in origin, supplied the biceps brachii (Nerve to muscle biceps brachii). In the lower part a branch arising from the median nerve in the cubital fossa continued as lateral cutaneous nerve of forearm (Figure 2).
In the right axilla and arm the course and origin of musculocutaneous nerve was as usual.
Discussion
Musculocutenaous nerve arises from the lateral cord (cervical 5 to 7 roots) opposite the lower border of pectoralis minor. It pierces the coracobrachialis and descends laterally between biceps and brachialis to the lateral side of the arm. Variations may be frequent. It may run behind the coracobrachilalis muscle or adhere for some distance to the median nerve and pass behind the biceps or may be accompanied by fibers from the median nerve as it transits coracobrachialis [9,10]. Less frequently median nerve may send a branch to musculocutaneous nerve.
During shoulder surgery it is important to identify or palpate the musculocutaneous nerve, as it is vulnerable to injury from retractors placed under the coracoid process. During coracoid process grafting, shoulder dislocation and frequent arthroscopies may damage the muscle as well as the nerve [11]. The lesion of the musculocutaneous nerve leads to weakness of elbow flexion because biceps and coracobrachialis are paralyzed and sensory impairment on the extensor aspect of the forearm in the distribution of the lateral cutaneous nerve of forearm. Pain and parasthesia may be aggravated by elbow extension.
Brachial plexus injuries may occur following trauma, traction, compression of nerves and shoulder dislocation during traumatic delivery in infants and malposition of the patient during anesthesia [12]. This result in complete or partial palsy of the musculature innervated. Via nerve grafting recovery can be achieved. The priority of the restoration of function is also an important consideration. Elbow flexion should be given first priority followed by wrist extension, finger flexion and shoulder abduction in the order [13].
The knowledge of the variations of the course and distribution of the lateral cord of brachial plexus is important while performing neurotization of brachial plexus lesions, shoulder arthroscopy by anterior glenohumeral portal and shoulder reconstructive surgery so that these structures can be identified and protected.
References
- Abhaya A, Khanna J, Prakash R. Variation of the lateral cord of brachial plexus piercing coracobrachialis muscle. J Anat Soc India. 2003; 52: 168–170.
- Linell EA. The distribution of nerves in the upper limb, with reference to varaibilities and their clinical significance. J Anat. 1921; 55: 79–112.
- Miller RA. Comparative studies upon the morphology and distribution of the brachial plexus. Am J Anat. 1934; 54: 143–147.
- Iwamoto S, Kimura K, Takahashi Y, Konishi M. Some aspects of the communicating branch between the musculocutaneous and median nerves in man. Okajimas Folia Anat Jpn. 1990; 67: 47–52.
- Nakatani, Tanaka S, Mizukami S. Absence of the musculocutaneous nerve with innervation of coracobrachialis, biceps brachii, brachialis and the lateral border of the forearm by branches from the lateral cord of the brachial plexus. J Anat. 1997; 191: 459–460.
- Sud M, Sharma A. Absence of musulocutaneous nerve and the innervations of coracobrachialis, biceps brachii and brachialis from the median nerve. J Anat Soc India. 2000; 49: 176–177.
- Chauhan, R, Roy TS. Communication between the median and musculocutaneous nerve – a case report. J Anat Soc India. 2002; 51: 72–75.
- Abhaya A, Khanna J, Prakash R. Variation of the lateral cord of brachial plexus piercing coracobrachialis muscle. J Anat Soc India. 2003; 52: 168–170.
- Kaus M, Wotowicz Z. Communicating branch between the musculocutaneous and median nerves in human. Folia Morphol (Warsz) 1995, 54: 273–277.
- Kabak S, Ekinci N, Halici M, Karaoglu S, Unur E, Ulger H. Formation variations of median nerve. Joint Dis Relat Surg. 2001; 12: 183–185.
- Flatow EL, Bigliani LU, April EW. An anatomic study of the musculocutaneous nerve and its relationship to the coracoid process. Clin Orthop Relat Res. 1989; 244: 166–171.
- Cooper DE, Jenkins RS, Bready L, Rockwood CA Jr. The prevention of injuries of the brachial plexus secondary to malposition of the patient during surgery. Clin Orthop Relat Res. 1988; 228: 33–41.
- Sedel L. Repair of severe traction lesions of the brachial plexus. Clin Orthop Relat Res. 1988; 237: 62–66.