Actinomycosis of abdominal wall
Received: 02-Jan-2018 Accepted Date: Jan 15, 2018; Published: 10-Feb-2018
Citation: Loudjedi S, Bereksi A, Fandi B, et al. Actinomycosis of abdominal wall. Surg Case Rep. 2018;2(1):7-8.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Actinomycosis is a subacute pseudo-tumor suppurative disease due to Infection with an anaerobic Gram-positive bacillus, Actinomyces, the mostly saprophytic germ of ORL area and the digestive tract. Traditional abdominopelvic disorders are contiguity after a colic or rectal infection (sigmoiditis, appendicitis, for example). Actinomycosis makes a diagnostic problem in that it is present in the majority of cases in the form of an abdominal or pelvic tumor. Morphological examinations such as the scanner and bacteriological samples that facilitate the detection of the disease. In some cases surgical exploration is necessary and it is the biopsy and the examination Anatomopathology extemporaneous confirming the diagnosis. The authors report an exceptional observation to illustrate the polymorphous presentation and the difficulty of management of this disease.
Keywords
Actinomycosis; Abdominal wall tumor; Antibiotics; Surgery
Primary actinomycosis of the abdominal wall is a rare clinical entity. Only 7 adequately described cases have been reported in the English literature. We report an isolated case of abdominal wall actinomycosis involving the left lower quadrant of the abdominal wall in a 32-year-old diabetic male. Surgical drainage of the abscess followed by long-term administration of penicillin resulted in cure. The clinicopathological spectrum of actinomycosis is reviewed and isolated involvement of the abdominal wall is characterized in light of the knowledge acquired from the available literature on this rare clinical presentation. The significance of obtaining tissues for culture and histopathology in all inflammatory lesions is emphasized [1].
Case Report
A 25-year-old man came to the consultation for an abdominal mass.The onset of the symptomatology seemed to date back to few months. There was a small parietal mass of peri-umbilical seat. This mass increased in volume thus reaching the epigastric and pelvic region. There was no alteration in the general condition, weight loss and transit disorders. The palpation of the abdomen revealed the characteristics of this mass: hard heterogeneous, fuzzy boundaries, strongly adherent to the deep plane, fixed to the adjacent tissue structures with an induration of the facing wall, thus giving an almost cardboard-like appearance of the entire abdominal wall.
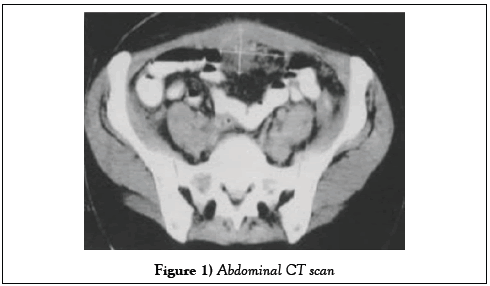
Biologically, there was a 23 × 109/l leukocytosis, 635 × 109/l thrombocythemia, a plasma C reactive protein (CRP) of 171 mg/l. The dosage of CA 125 was normal to 24 KU/l. CT scan (Figure 1) revealed the presence of a parietal mass. Abdominopelvic heterogeneous repressing digestive structures with multiple adhesions, without any other abnormalities in the intra-abdominal organs. In front of this picture strongly evocative of a parietal tumor probably malignant a surgical exploration was decided (Figure 1).
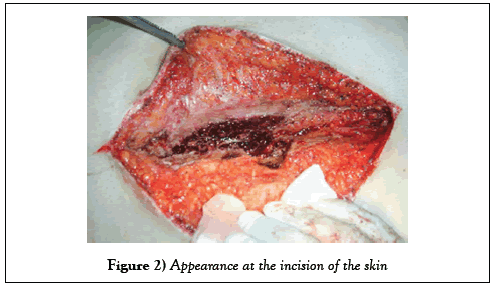
The patient was admitted to the operating room under general anesthesia. The incision started at scalpel opening the skin and subcutaneous tissue (Figure 2).
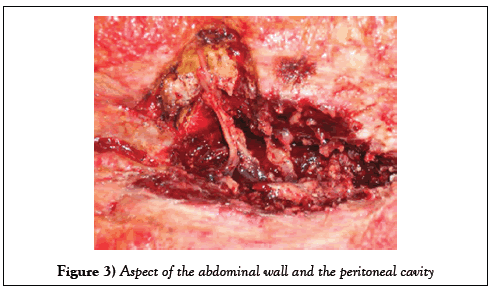
The remainder of the laparotomy was made with the electric bistoury. Unfortunatly the parietal mass was hard and invincible thus preventing any penetration into the abdominal cavity.
There were multiple adhesions and any manipulation of intra-abdominal viscera was hazardous. The macroscopic aspect was that of a solid tumor fixed at different elements of the abdominal wall (Figure 3).
A biopsy was performed; the wall was closed with Vicryl 1 by separated points. Finally the skin was sutured with nylon 2/0. Surgical follow-up was simple except for one surgical site infection that lasted two weeks. The patient was treated for 10 days with intravenous antibiotic therapy combining 12 g/day of Amoxicillin and 1.5 g of metronidazole. In view of the rapid improvement clinical and biological status, antibiotic therapy was continued orally, (3 g/ day of Amoxicillin alone), and for a period of three months. At five months of the intervention, the patient had no functional complaint, abdominal palpation were painless with flexible fabrics. The mass had completely disappeared.
Discussion
There are no studies that allow an accurate assessment of the frequency of probably very rare. However, identified Actinomyces infections are more common Cervico-facial (65%) than abdominopelvic (20%) or thoracopulmonary (15%) [2-4]. The parietal localization remains exceptional. Actinomycoses Abdominopelvic are therefore very rare, but their prevalence seems to increase with The use of IUDs for a contraceptive purpose. Actinomyces is a saprophytic germ of the oropharynx and the digestive tract. Abdominopelvic actinomycosis is most commonly due to Actinomyces Israeli. This bacterium is unable to infect its host in the absence of lesions of the mucous membranes. But Actinomycosis infiltrates the tissues extensively [2] (which is responsible for the induration of the tissues) [5]. Actinomyces form filamentous aggregates made from numerous germs, including extremities are swollen “in clubs”, glycoproteins and calcium phosphate which surround themselves with an inflammatory granuloma, thus forming abscesses that can fistulate.
How to make the diagnosis of abdominopelvic actinomycosis?
Although observations of abdominopelvic actinomycosis are abundantly regularly reported in the literature (259 references in the database of Medline with the interface “Pubmed”), the diagnosis is rarely evoked preoperatively. The clinic which is non-specific is also varied in its presentation as illustrated by our case. The clinic finds abdominal and/or pelvic mass, painful with a febrile state. There is often an alteration of the general condition with a consequent loss of weight. The Inflammatory biological syndrome is constant and marked. The rate of CA 125 is sometimes increased. Ultrasound, CT scan and nuclear magnetic resonance imaging (MRI) confirm the tumor syndrome, show its extension but do not make it possible to diagnosis actinomycosis. Differential diagnoses are abdominopelvic abdominal cancer or abdominopelvic lesions. In the first place, the diagnosis of cancer (colic, ovarian, uterine or bladder) is mentioned; Ignoring the diagnosis can lead to inappropriate, radical, morbid and mutilating surgical procedures. The presence of an IUD (intrauterine device) or its recent with-drawal when an abdominopelvic tumor syndrome is detected should suggest an abdominopelvic actinomycosis. In fact, in one isolated case, a mutilating surgery was performed on a patient who had worn an IUD and who caused an actinomycotic abscess simulating a malignant tumor [6]. There is no routine serological diagnosis. Pre-operative diagnosis could be bacteriological, it is however difficult to establish. It is obtained after puncturing any collections under ultrasound or under scanning [7,8].
In abdomino-pelvic or parietal actinomycosis, the therapeutic approach must be drug even if surgical resection of the abscessed lesions has not been performed or has been incomplete [9,10]. Conversely, if the surgery is satisfactory, antibiotic therapy can be alleviated after surgery (3 grams of Amoxicillin) and duration (1 to 2 months) without excessive risk of relapse [11].
The presented case is very rare for several reasons:
1. Diagnostic step: in this phase the iconography reveals an abdominal mass which looks like a leiomyosaroma. The examination by a needle puncture was required but any attempt was impossible given the hardness of the mass. Moreover the calcified appearance of the mass did not improve the diagnosis. The CT scan revealed a heterogeneous mass which gived rise to several possible diagnoses. Hence we had to use an invasive approach to confirm the final diagnosis. This was performed by biopsy.
2. Treatment step: The second pitfall that the surgeons encountered was the impossibility of dissecting the mass and the periphery of the latter because of the presence of very hard adhesions forming magma at the level of the wall. This magma has lost all the anatomical landmarks (peritoneal fasciae muscles) thus making any dissection or attempted resection risky or dangerous. This situation was a surgical stalemate and the only and final step that surgeons could make was to practice a small, limited resection and to make an anatomic pathological examination. Due to the impossibility of removing the tumor, no loss of substance was provoked and therefore no parietal replacement prosthesis was used as was the case in [12].
3. A similar case was reported in [13] but iconography was poor compared with ours’. In fact, there were no pictures representing the muscles and peritoneum aspect after actinomycosis colonisation.
Conclusion
Actinomycosis abscess can affect the colon, ileum, uterus and tract, liver, abdominal wall, pancreas, greater omentum, retroperitoneum and kidney. In the literature there are not many reports of actinomyces abscess of the abdominal wall. The diagnosis preoperative bacteriological is difficult to establish. Diagnosis is most often carried out retrospectively by pathological examination. Surgery is therefore most often necessary. The extemporaneous histological analysis of the surgical specimens limits the risks of surgery. Extensive, complicated digestive or urinary tract complication, even if the treatment of abdominopelvic actinomycosis relies on antibiotic therapy, surgery. In conclusion it happens that the surgeon, whatever his experience, finds his work very limited by extreme anatomical situations, thus preventing him from making a good diagnosis and thus the proper treatment.
Conflict of Interest
None.
Patient Consent
None.
REFERENCES
- Khalid K, Shabir A, Qazi MD, et al. Saudi Med J. 2004;25(2): 229-233.
- Bittar I, Solal CJL, Cabanis P. Abdominopelvic actinomycosis. Ann Chir. 2001;126:494-496.
- Huss M, Bongain A, Hofman P, et al. A difficult diagnosis: the abscess Actinomycotic pelvi-abdominal. J Gynecol Obstet Biol Reprod. 1993;22:843-847.
- Bercovich A, Guy M, Karayiannakis AJ, et al. Ureteral obstruction and reconstruction in Pelvic actinomycosis. Urology. 2003;61:224.
- Lee IJ, Ha HK, Park CM, et al. Abdominopelvic actinomycosis involving the gastrointestinal tract: CT features. Radiology. 2001;220:76-80.
- Acquaro P, Tagliabue F, Confalonieri G, et al. Abdominal wall actinomycosis simulating a malignant neoplasm: A case report and review of the literature. World J Gastrointest Surg? .2010 Jul 27;2(7):247–250.
- Lee YC, Min D, Holcomb K, et al. Computed tomography guided core needle biopsy diagnosis of pelvic actinomycosis. Gynecol Oncol. 2000;79:318-323.
- Longchampt E, Vessieres A, Fabre M. How fine needle aspiration biopsy makes it possible to avoid extensive surgery. A case of abdominopelvic actinomycosis. Ann Pathol. 2000;20:145-149.
- Nawroth F, Foth D, Schmidt T, et al. Differential diagnosis and non-surgical treatment of pelvic actinomycosis. Acta Obstet Gynecol Scand. 2000;79:1024-1025.
- Noomene F, Zouari K, Kallel W, et al. L’actinomycose Abdominal. 3 observations. Presse Med. 2003;32:698-700.
- Atad J, Hallak M, Sharon A, et al. Pelvic actinomycosis. Is long-term antibiotic therapy necessary? J Reprod Med. 1999;44:939-944.
- Ladurner R, Bogner JR, Drosse I, et al. A rare case of primary actinomycosis of the anterior abdominal wall: Diagnosis and treatment. Hernia. October 2008, 12(5),pp 549–552.
- Hefny AF, Joshi S, Saadeldin YA, et al. Primary anterior abdominal wall actinomycosis. Singapore Med J. 2006;47(5):419.