Alzheimer’s disease and periodontitis
Received: 21-Sep-2017 Accepted Date: Sep 28, 2017; Published: 05-Oct-2017
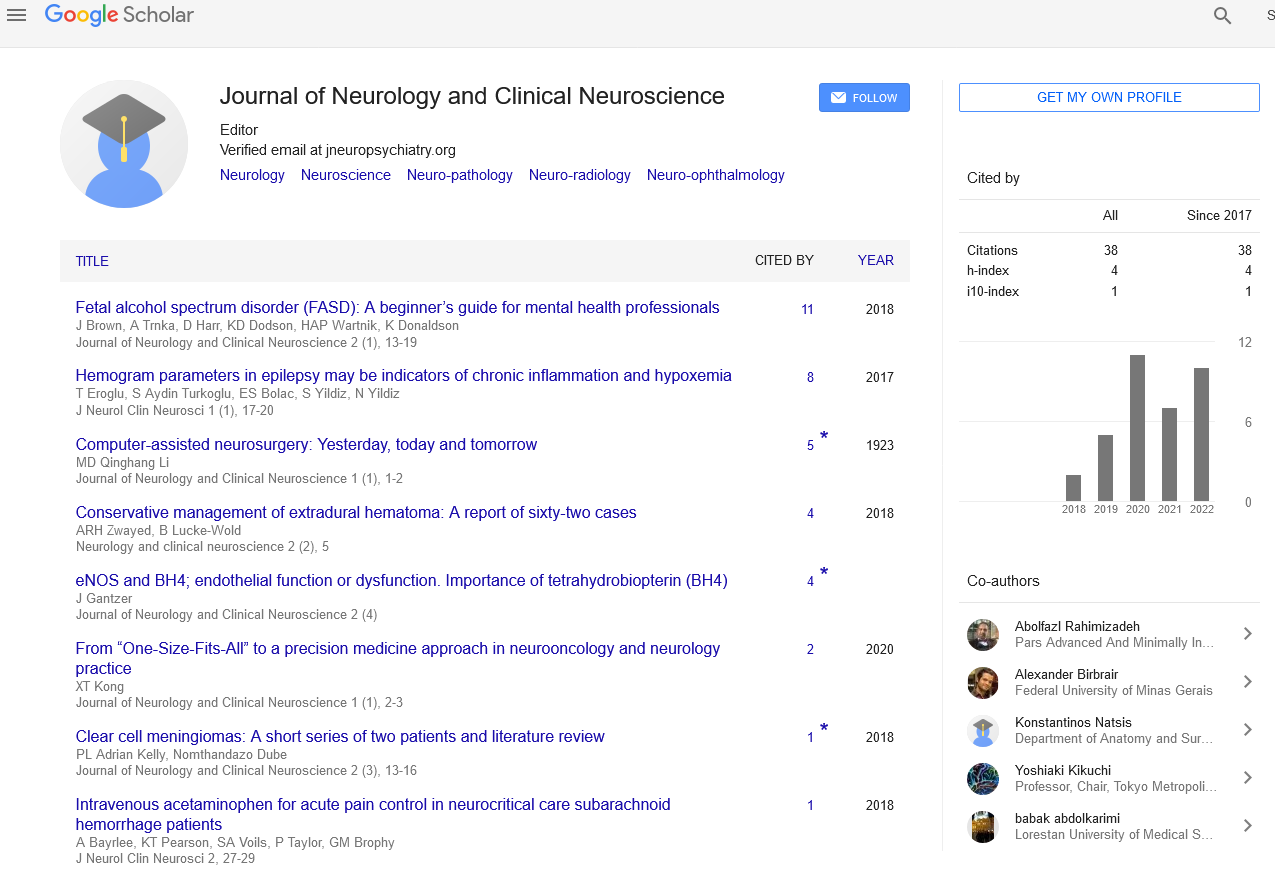
Citation: Palone MRT. Alzheimer’s disease and periodontitis. J Neurol Clin Neurosci. 2017;1(1): 7.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Commentary
Alzheimer’s Disease (AD) is a neurological disorder that affects million people worldwide. Generally, the symptoms of AD first appear in their mid-60s. Clinically, they include unpredictable behavior, memory loss and language problems [1].
With the disease progression, patients may experience more severe symptoms such as hallucinations, delusions and paranoia. Moreover, in more advanced stages of AD, the people often cannot communicate and they depend on caregivers for their survival [1].
It should be noted that the brain of a patient with AD is characterized by presence of amyloid plaques, neurofibrillary tangles, chronic inflammation, vascular problems and extensive neuronal loss [2]. The presence of neurofibrilary tangles and amyloid plaques in the brain are considered the hallmarks of this neurological disorder [1].
Concerning the etiology of AD, a combination of genetic, environmental and lifestyle factors has been described [2]. In this sense, even oral diseases (periodontitis) have been reported in the literature as a risk factor for AD [3].
Another relevant point is that patients with AD have poor oral health when compared with those without the disease. A higher number of oral pathologies and a lower number of natural teeth have also been reported in this case [4]. In addition, the periodontal health status of such patients deteriorates with the disease progression, due to damages in their cognitive function [4,5].
Thus, the present article discusses briefly about a possible relationship between periodontitis and AD.
First of all, it is important to know that periodontitis has been associated with an increase in cognitive decline in AD, which may be mediated through effects on systemic inflammation [6].
It is also worth highlighting that periodontal pathogens, such as Porphyromonas gingivalis, Tannerella forsythia and Treponema denticola, have been implicated in the development of AD. In this context, one of the possible explanations is the existence of a vicious cycle of sustained local inflammatory milieu in the brain that results in the loss of cytoarchitectural integrity and vital neurons. Consequently, there is also a subsequent loss of function, that is, memory deterioration in patients with AD [7].
Furthermore, a causal relationship between periodontal bacteria and nonoral Treponema species of bacteria via the amyloid-beta and inflammatory links has been suggested. Thereby, periodontitis could be a risk factor for AD, since that it can provide harmful bacteria to the brain [8].
According to Shoemark and Allen (2015) such entry of bacteria occurs in the following manner: aging favors the overgrowth of oral anaerobes established earlier in life. This, in turn, provokes a pro-inflammatory innate response that weakens of the blood-brain barrier. Therewith, bacteria can spread in the brain [9].
On top of this, given the evidence of high levels of antibodies to periodontal pathogens in people with AD years before cognitive impairment, it is highly likely, in fact, that periodontitis can be related to both the onset and progression of this neurological disease [10].
In conclusion, (in the same way as for the Parkinson’s disease) dentists should also be included in the multidisciplinary teams for treatment of AD [11], in order to delay the progression of such disorder and improve the quality of live of these patients. Moreover, dental plaque control may help prevent AD in the general population. Therefore, oral health promotion initiatives are a crucial subject matter for planning public health activities aiming prevention and treatment of this serious disease.
REFERENCES
- National Institute on Aging. Alzheimer's disease fact sheet. 2017.
- National Institute on Aging. What happens to the brain in Alzheimer's disease. 2017.
- Ganesh P, Karthikeyan R, Muthukumaraswamy A, et al. A potential role of periodontal inflammation in Alzheimer's disease: a review. Oral Health Prev Dent. 2017;15(1):7-12.
- Ribeiro GR, Costa JL, Ambrosano GM, et al. Oral health of the elderly with Alzheimer's disease. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(3):338-43.
- Martande SS, Pradeep AR, Singh SP. Periodontal health condition in patients with Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2014;29(6):498-502.
- Ide M, Harris M, Stevens A. Periodontitis and cognitive decline in Alzheimer's disease. PLoS One. 2016;11(3):e0151081.
- Singhrao SK, Harding A, Simmons T. Oral inflammation, tooth loss, risk factors, and association with progression of Alzheimer's disease. J Alzheimers Dis. 2014;42(3):723-37.
- Olsen I, Singhrao SK. Can oral infection be a risk factor for Alzheimer's disease?. J Oral Microbiol. 2015;7:29143.
- Shoemark DK, Allen SJ. The microbiome and disease: reviewing the links between the oral microbiome, aging, and Alzheimer's disease. J Alzheimers Dis. 2015;43(3):725-38.
- Sparks Stein P, Steffen MJ, Smith C. Serum antibodies to periodontal pathogens are a risk factor for Alzheimer's disease. Alzheimers Dement. 2012;8(3):196-203.
- Palone MRT. Parkinson’s disease and oral health status: an approach to the public health aspect. J Neurol Clin Neurosci. 2017;1(1):1-1.