An aberrant right lateral branch from right internal thoracic arteryside
Vishal Manoharrao Salve* and Challa Ratnaprabha
Department of Anatomy, Dr. Pinnamaneni Siddhartha Institute of Medical Sciences & Research Foundation, Chinnaoutpalli, Gannavaram Mandal, Krishna District (AP), India
- *Corresponding Author:
- Vishal Manoharrao Salve, MBBS, MS
Assistant Professor, Department of Anatomy, Dr. Pinnamaneni Siddhartha Institute of Medical Sciences & Research Foundation Chinnaoutpalli, Gannavaram Mandal Krishna District (AP), 521286, India
Tel: +91-986-6379916
E-mail: salvevishal73@gmail.com
Date of Received: December 6th, 2009
Date of Accepted: July 11th, 2010
Published Online: August 10th, 2010
© Int J Anat Var (IJAV). 2010; 3: 114–116.
[ft_below_content] =>Keywords
internal thoracic artery, aberrant lateral branch, coronary artery by-pass grafting
Introduction
The internal thoracic artery is the largest artery of the thoracic wall. It arises from the first part of subclavian artery. It usually lays finger breadth lateral to the border of sternum. It should be avoided in intercostal paracentesis of pericardial sac by passing needle very close to sternal margin [1].
The internal thoracic artery usually gives pericardiophrenic, mediastinal, pericardial, sternal, anterior intercostal, perforating and terminal branches as described in various textbooks of anatomy [2–4]. The internal thoracic artery is often mobilized for coronary artery by-pass grafting. It is the main source of blood supply to sternum and any damage to this supply result in sternal wound complication [5].
Here we describe an unreported case of an aberrant right lateral branch from right internal thoracic artery.
Case Report
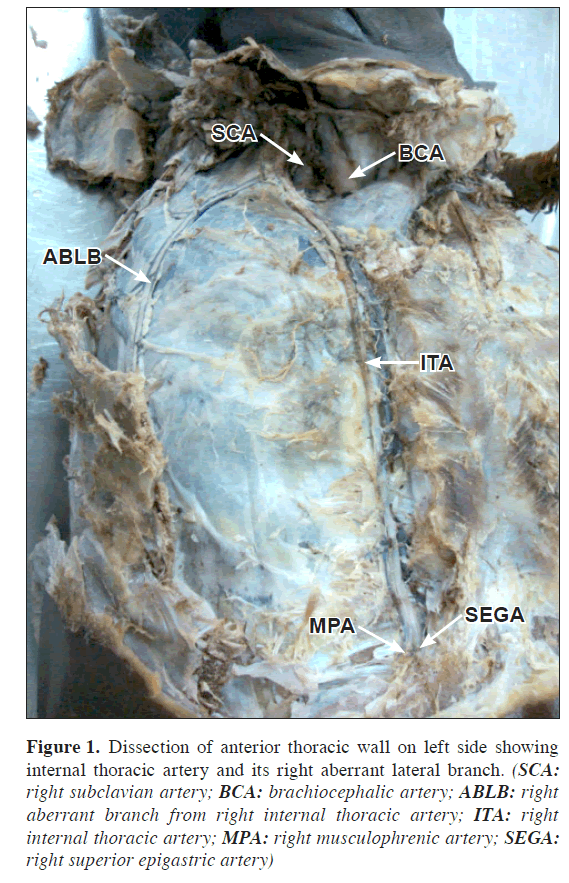
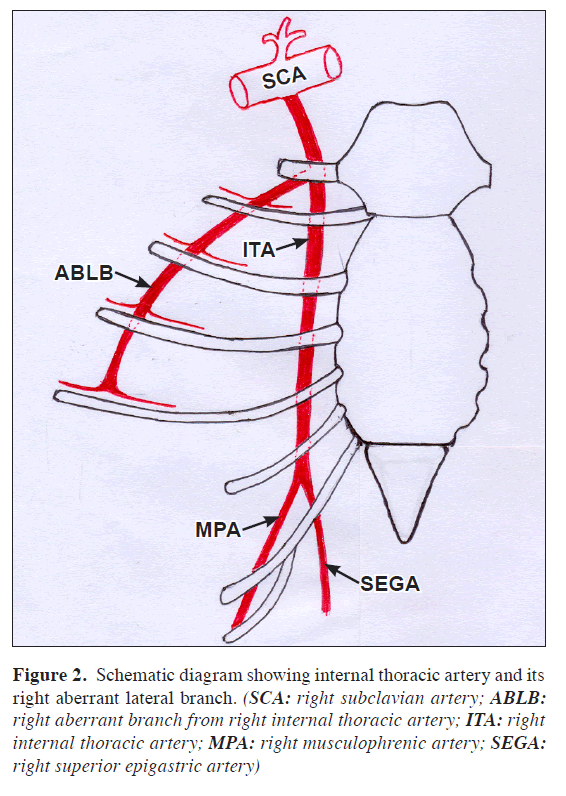
During routine dissection (MBBS Batch 2009-2010) of a middle aged male cadaver at the Dr. Pinnamaneni Siddhartha Institute of Medical Sciences & Research Foundation, Gannavaram, Krishna Dist. AP (INDIA); an aberrant right lateral branch from right internal thoracic artery was found. It arose from right internal thoracic artery behind right first rib about 5 mm below its origin from subclavian artery. It ran downward for first four intercostal spaces about 1 cm away from mid-axillary line. It terminated into two intercostal arteries on either arteryside in the 4th intercostal space. It gave one branch each on either side for first four intercostal spaces. The right internal thoracic artery terminated by bifurcating into superior epigastric and musculophrenic arteries in the 6th intercostal space. The length of right internal thoracic artery from its origin to bifurcation was 157 mm. The diameter of right internal thoracic artery at its origin was 3 mm and of an aberrant right lateral branch was 3 mm. There was no such branch on left side. The left internal thoracic artery terminated in the 6th intercostal space. The diameter of left internal thoracic artery at its origin was 3 mm.
Discussion
Occasionally the internal thoracic artery has an aberrant lateral branch which has been termed internal thoracic, lateral internal mammary, retrocostal, subcostal and lateral intracostal. It is usually small and arising from internal thoracic artery close to its origin or occasionally independently from the subclavian artery. It runs downwards only two or four intercostal spaces [1].
Gupta et al. studied 30 specimens of anterior thoracic wall obtained from adult cadavers, in the department of Anatomy, Postgraduate Institute of Medical Education and Research, Chandigarh [6]. The mean length of internal thoracic artery was same on the both side (right 158.0 ±2.6 mm, left 158.0 ±1.3 mm). The commonest level of termination of right (76.7%) and left (60%) internal thoracic artery was 6th rib or 6th intercostal space. The total number of trifurcation of both internal thoracic arteries was 8.3% and total bifurcation was 91.7%. In case of trifurcation the third branch was found to be supplying the diaphragm.
Puri et al. studied 100 (76 males, 24 females) adult cadavers [7]. In their study, 15% cases of internal thoracic artery took origin from a trunk in common with other branches of subclavian artery. Internal thoracic artery originated from first part of subclavian artery in 96 specimens on left side and in 88 specimens on right side. In 4 specimens on left side and 12 specimens on right side; it originated as branch of common trunk that gives origin to other branches of subclavian artery. The mean length of internal thoracic artery was 192.5 ±23.0 mm on left side and 195.4 ±22.4 mm on right side. Internal thoracic artery terminated in left 6th intercostal space in 52% cases and in right 6th intercostal space in 54% cases. Remaining specimens it terminated at variable level ranging from 4th intercostal space to 7th intercostal space.
Figure 1: Dissection of anterior thoracic wall on left side showing internal thoracic artery and its right aberrant lateral branch. (SCA: right subclavian artery; BCA: brachiocephalic artery; ABLB: right aberrant branch from right internal thoracic artery; ITA: right internal thoracic artery; MPA: right musculophrenic artery; SEGA: right superior epigastric artery)
Voster et al. studied internal thoracic and vertebral arteries in 60 cadavers from the department of Anatomy of University of Pretoria [8]. In 60 cadavers, the internal thoracic artery branched off the first part of the subclavian artery in all cases except one (0.83%). The variant artery was found on right side, originating 70.3 mm lateral to the division of common carotid artery from brachiocephalic trunk. Carrier et al. reported that after sternotomy and bilateral grafting of internal thoracic artery the decrease in blood supply to the sternum was only transient and completely reverted one month after the operation [5].
In revascularization of the myocardium, the coronary artery is surgically anastomosed with the internal thoracic artery by mobilizing latter [3]. This area is also used in patients for percutaneous subclavian vein catheterization to determine central venous pressure or to administer drugs and solutions in emergencies. It is also used in introducing a pacemaker [8].
The rare and unexpected variations of the internal thoracic artery such as the one reported here may complicate the entire procedure of coronary artery by-pass grafting. The embryological basis of present case is not known. The vertical part of the internal thoracic artery develops from the ventral anastomosis between the ventral divisions of thoracic intersegmental arteries [9]. Thus this rare variant of the internal thoracic artery is of great concern during any surgical procedure that involves this artery or this area.
Figure 2: Schematic diagram showing internal thoracic artery and its right aberrant lateral branch. (SCA: right subclavian artery; ABLB: right aberrant branch from right internal thoracic artery; ITA: right internal thoracic artery; MPA: right musculophrenic artery; SEGA: right superior epigastric artery)
References
- Hollinshead WH. Anatomy for surgeons. 2nd Ed., New York, Harper & Row Publishers. 1961; 8–9.
- Williams PL, ed. Gray’s Anatomy. The anatomical basis of medicine and surgery. 38th Ed., Edinburgh, Churchill Livingstone. 1995; 1529.
- Moore KL, Dalley AF. Clinically oriented Anatomy. 5th Ed., Philadelphia, Lipppincott Williams & Wilkins. 1999; 104, 161.
- McMinn RMH. Last’s Anatomy, Regional and applied. 9th Ed., Edinburgh, Churchill Livingstone. 1994; 248.
- Carrier M, Gregoire J, Tronc F, Cartier R, Leclerc Y, Pelletier LC. Effect of internal mammary artery dissection on sternal vascularization. Ann Thorac Surg. 1992; 53: 115–119.
- Gupta M, Sodhi L, Sahni D. The branching pattern of internal thoracic artery on the anterior chest wall. J Anat Soc India. 2002; 51: 194–198.
- Puri N, Gupta PK, Mahant TS, Puri D. Bilateral internal thoracic artery harvesting; anatomical variation to be considered. Ind J Thorac Cardiovasc Surg. 2007; 23: 192–196.
- Vorster W, du Plooy PT, Meiring JH. Abnormal origin of internal thoracic and vertebral arteries. Clin Anat. 1998; 11: 33–37.
- Rao KPS, Dutta S, Narayana K. A rare variant of the internal thoracic (mammary) artery. Eur J Anat. 2004; 8: 35–37.
Vishal Manoharrao Salve* and Challa Ratnaprabha
Department of Anatomy, Dr. Pinnamaneni Siddhartha Institute of Medical Sciences & Research Foundation, Chinnaoutpalli, Gannavaram Mandal, Krishna District (AP), India
- *Corresponding Author:
- Vishal Manoharrao Salve, MBBS, MS
Assistant Professor, Department of Anatomy, Dr. Pinnamaneni Siddhartha Institute of Medical Sciences & Research Foundation Chinnaoutpalli, Gannavaram Mandal Krishna District (AP), 521286, India
Tel: +91-986-6379916
E-mail: salvevishal73@gmail.com
Date of Received: December 6th, 2009
Date of Accepted: July 11th, 2010
Published Online: August 10th, 2010
© Int J Anat Var (IJAV). 2010; 3: 114–116.
Abstract
The internal thoracic artery is the largest artery of the thoracic wall. The internal thoracic artery is often mobilized for coronary artery bypass grafting. During routine dissection (MBBS Batch 2009-2010) of a middle aged male cadaver at Dr. Pinnamaneni Siddhartha Institute of Medical Sciences & Research Foundation, Gannavaram, (INDIA); an aberrant right lateral branch from right internal thoracic artery was found. It arose from right internal thoracic artery behind right first rib. It ran downward for first four intercostal spaces about 1 cm away from the mid-axillary line. It terminated into two intercostal arteries on either side in the 4th intercostal space. The rare and unexpected occurrence of variation of the internal thoracic artery such as the one reported here may complicate the entire procedure of coronary artery by-pass grafting. Thus this rare variant of the internal thoracic artery is of great concern during any surgical procedure that involves this artery.
-Keywords
internal thoracic artery, aberrant lateral branch, coronary artery by-pass grafting
Introduction
The internal thoracic artery is the largest artery of the thoracic wall. It arises from the first part of subclavian artery. It usually lays finger breadth lateral to the border of sternum. It should be avoided in intercostal paracentesis of pericardial sac by passing needle very close to sternal margin [1].
The internal thoracic artery usually gives pericardiophrenic, mediastinal, pericardial, sternal, anterior intercostal, perforating and terminal branches as described in various textbooks of anatomy [2–4]. The internal thoracic artery is often mobilized for coronary artery by-pass grafting. It is the main source of blood supply to sternum and any damage to this supply result in sternal wound complication [5].
Here we describe an unreported case of an aberrant right lateral branch from right internal thoracic artery.
Case Report
During routine dissection (MBBS Batch 2009-2010) of a middle aged male cadaver at the Dr. Pinnamaneni Siddhartha Institute of Medical Sciences & Research Foundation, Gannavaram, Krishna Dist. AP (INDIA); an aberrant right lateral branch from right internal thoracic artery was found. It arose from right internal thoracic artery behind right first rib about 5 mm below its origin from subclavian artery. It ran downward for first four intercostal spaces about 1 cm away from mid-axillary line. It terminated into two intercostal arteries on either arteryside in the 4th intercostal space. It gave one branch each on either side for first four intercostal spaces. The right internal thoracic artery terminated by bifurcating into superior epigastric and musculophrenic arteries in the 6th intercostal space. The length of right internal thoracic artery from its origin to bifurcation was 157 mm. The diameter of right internal thoracic artery at its origin was 3 mm and of an aberrant right lateral branch was 3 mm. There was no such branch on left side. The left internal thoracic artery terminated in the 6th intercostal space. The diameter of left internal thoracic artery at its origin was 3 mm.
Discussion
Occasionally the internal thoracic artery has an aberrant lateral branch which has been termed internal thoracic, lateral internal mammary, retrocostal, subcostal and lateral intracostal. It is usually small and arising from internal thoracic artery close to its origin or occasionally independently from the subclavian artery. It runs downwards only two or four intercostal spaces [1].
Gupta et al. studied 30 specimens of anterior thoracic wall obtained from adult cadavers, in the department of Anatomy, Postgraduate Institute of Medical Education and Research, Chandigarh [6]. The mean length of internal thoracic artery was same on the both side (right 158.0 ±2.6 mm, left 158.0 ±1.3 mm). The commonest level of termination of right (76.7%) and left (60%) internal thoracic artery was 6th rib or 6th intercostal space. The total number of trifurcation of both internal thoracic arteries was 8.3% and total bifurcation was 91.7%. In case of trifurcation the third branch was found to be supplying the diaphragm.
Puri et al. studied 100 (76 males, 24 females) adult cadavers [7]. In their study, 15% cases of internal thoracic artery took origin from a trunk in common with other branches of subclavian artery. Internal thoracic artery originated from first part of subclavian artery in 96 specimens on left side and in 88 specimens on right side. In 4 specimens on left side and 12 specimens on right side; it originated as branch of common trunk that gives origin to other branches of subclavian artery. The mean length of internal thoracic artery was 192.5 ±23.0 mm on left side and 195.4 ±22.4 mm on right side. Internal thoracic artery terminated in left 6th intercostal space in 52% cases and in right 6th intercostal space in 54% cases. Remaining specimens it terminated at variable level ranging from 4th intercostal space to 7th intercostal space.
Figure 1: Dissection of anterior thoracic wall on left side showing internal thoracic artery and its right aberrant lateral branch. (SCA: right subclavian artery; BCA: brachiocephalic artery; ABLB: right aberrant branch from right internal thoracic artery; ITA: right internal thoracic artery; MPA: right musculophrenic artery; SEGA: right superior epigastric artery)
Voster et al. studied internal thoracic and vertebral arteries in 60 cadavers from the department of Anatomy of University of Pretoria [8]. In 60 cadavers, the internal thoracic artery branched off the first part of the subclavian artery in all cases except one (0.83%). The variant artery was found on right side, originating 70.3 mm lateral to the division of common carotid artery from brachiocephalic trunk. Carrier et al. reported that after sternotomy and bilateral grafting of internal thoracic artery the decrease in blood supply to the sternum was only transient and completely reverted one month after the operation [5].
In revascularization of the myocardium, the coronary artery is surgically anastomosed with the internal thoracic artery by mobilizing latter [3]. This area is also used in patients for percutaneous subclavian vein catheterization to determine central venous pressure or to administer drugs and solutions in emergencies. It is also used in introducing a pacemaker [8].
The rare and unexpected variations of the internal thoracic artery such as the one reported here may complicate the entire procedure of coronary artery by-pass grafting. The embryological basis of present case is not known. The vertical part of the internal thoracic artery develops from the ventral anastomosis between the ventral divisions of thoracic intersegmental arteries [9]. Thus this rare variant of the internal thoracic artery is of great concern during any surgical procedure that involves this artery or this area.
Figure 2: Schematic diagram showing internal thoracic artery and its right aberrant lateral branch. (SCA: right subclavian artery; ABLB: right aberrant branch from right internal thoracic artery; ITA: right internal thoracic artery; MPA: right musculophrenic artery; SEGA: right superior epigastric artery)
References
- Hollinshead WH. Anatomy for surgeons. 2nd Ed., New York, Harper & Row Publishers. 1961; 8–9.
- Williams PL, ed. Gray’s Anatomy. The anatomical basis of medicine and surgery. 38th Ed., Edinburgh, Churchill Livingstone. 1995; 1529.
- Moore KL, Dalley AF. Clinically oriented Anatomy. 5th Ed., Philadelphia, Lipppincott Williams & Wilkins. 1999; 104, 161.
- McMinn RMH. Last’s Anatomy, Regional and applied. 9th Ed., Edinburgh, Churchill Livingstone. 1994; 248.
- Carrier M, Gregoire J, Tronc F, Cartier R, Leclerc Y, Pelletier LC. Effect of internal mammary artery dissection on sternal vascularization. Ann Thorac Surg. 1992; 53: 115–119.
- Gupta M, Sodhi L, Sahni D. The branching pattern of internal thoracic artery on the anterior chest wall. J Anat Soc India. 2002; 51: 194–198.
- Puri N, Gupta PK, Mahant TS, Puri D. Bilateral internal thoracic artery harvesting; anatomical variation to be considered. Ind J Thorac Cardiovasc Surg. 2007; 23: 192–196.
- Vorster W, du Plooy PT, Meiring JH. Abnormal origin of internal thoracic and vertebral arteries. Clin Anat. 1998; 11: 33–37.
- Rao KPS, Dutta S, Narayana K. A rare variant of the internal thoracic (mammary) artery. Eur J Anat. 2004; 8: 35–37.