An incidental finding of the accessory inferior thyroid artery
Jiri Sedy*
Institute of Experimental Medicine, Academy of Sciences of the Czech Republic, Prague, Czech Republic.
- *Corresponding Author:
- Jiri Sedy, MD
Institute of Experimental Medicine, Academy of Sciences of the Czech Republic, Videnska 1083, 142 20, Prague 4, Czech Republic.
Tel: +420 241062717
Fax: +420 241062783
E-mail: jirisedy@hotmail.com
Date of Received: June 24th, 2008
Date of Accepted: July 18th, 2008
Published Online: July 19th, 2008
© IJAV. 2008; 1: 10–11.
[ft_below_content] =>Keywords
inferior thyroid artery, variability, accessory, anatomy
Introduction
Inferior thyroid artery is one of the main arteries supplying thyroid gland and laryngeal muscles. It also supplies pharynx, esophagus, trachea and thymus. It emerges from the thyrocervical trunk of the subclavian artery at the level of C6 vertebra. Then, it rapidly curves inferomedially, crossing the bundle of common carotid artery, internal jugular vein and vagus nerve. Further, it continues to lower pole of the thyroid gland, crossing the recurrent laryngeal nerve. The main branches of inferior thyroid artery are inferior laryngeal artery, supplying mainly laryngeal musculature; glandular branches, supplying thyroid gland; and branches entering pharynx, esophagus, trachea and thymus. The knowledge of the anatomy of the inferior thyroid artery is important for neck surgeons, mainly during operations on thyroid and parathyroid glands [1,2].
Case Report
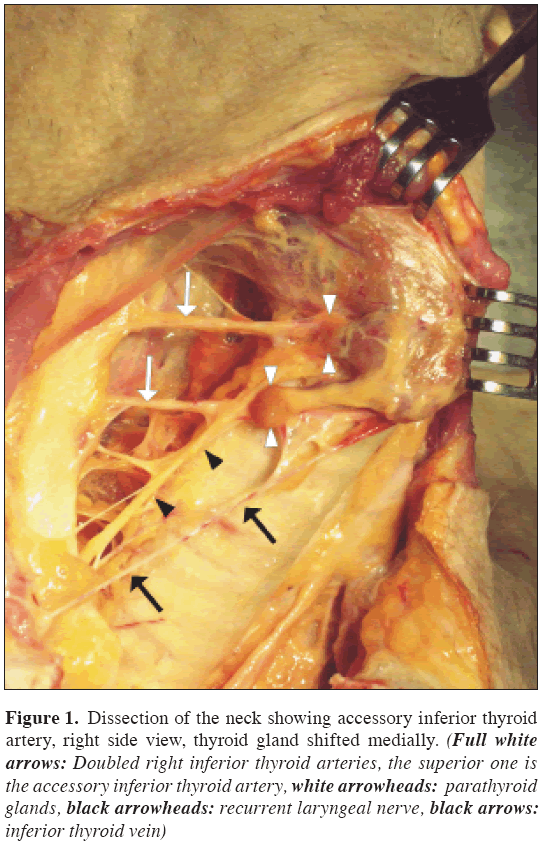
During the training of parathyroidectomy on cadavers at the Department of Pathology, First Faculty of Medicine, Charles University, Prague; in an adult male, where pathology of neck structures have been excluded, an accessory inferior thyroid artery was observed. On neck, collar skin incision followed by midline incision and sternotomy was performed. Thorax was opened. Superficial neck fascia was cut in midline; infrahyoid muscles pulled laterally, lobes of the thyroid gland were detached from surrounding structures and pulled medially. Both recurrent laryngeal nerve and inferior thyroid artery were cleaned. Parathyroid glands were found close to the site of crossing of recurrent laryngeal nerve and inferior thyroid artery. On the right side, doubled inferior thyroid artery was found (Figure 1), both arising separately from thyrocervical trunk. The lower artery was in a typical location, whereas the upper was recognized as accessory. On the left side, only single inferior thyroid artery was present. Only one inferior thyroid vein was found on each side. Preparation continued on the dorsal surface of thyroid gland, under the capsule of thyroid gland, along the course of recurrent laryngeal nerve and inferior thyroid artery, in the cervical and mediastinal lipothymic tissue, in the anterior mediastinum and in the parapharyngeal and the paraesophageal space. Four parathyroid glands were found in typical localization, close to the crossing of inferior thyroid artery and recurrent laryngeal nerve. All four parathyroid glands were verified histologically - samples were removed, put in 4% paraformaldehyde, dehydrated in alcohol series of ascending concentration, embedded to paraffin, cut to 10 μm section, stained with hematoxyline-eosin and analyzed with optic microscope.
Figure 1: Dissection of the neck showing accessory inferior thyroid artery, right side view, thyroid gland shifted medially. (Full white arrows: Doubled right inferior thyroid arteries, the superior one is the accessory inferior thyroid artery, white arrowheads: parathyroid glands, black arrowheads: recurrent laryngeal nerve, black arrows: inferior thyroid vein)
Discussion
Anatomical variability of neck vasculature is quite high. Venous variability is much higher than arterial. Arteries of the thyroid and parathyroid glands include superior thyroid artery, emerging from external carotid artery and inferior thyroid artery, emerging from the thyrocervical trunk. In a small percentage of cases, anomalous arteries to the thyroid occur [3]. The most important anatomical variety of thyroid arteries is the thyroidea ima artery, present in 1.5% - 12.2% of cases. In majority of cases, it emerges from brachiocephalic trunk, less often from right common carotid artery, aortic arch, internal thoracic artery or left common carotid artery [4]. Accessory inferior thyroid artery emerging from subclavian artery is very rare and often present more caudally to the inferior thyroid artery. The accessory inferior thyroid artery thus rather represents a rare variety of the thyroidea ima artery, emerging from subclavian artery than a typical accessory inferior thyroid artery. In our case, the inferior thyroid artery, which we recognized as normal, had a typical course and relation to surrounding structures, including recurrent laryngeal nerve and parathyroid glands, which were subsequently verified histologically. Normal anatomical position of parathyroid glands was defined previously by Bonjer and Bruining as the presence of demanded parathyroid glands within a circumscribed area 2 cm in diameter, 1 cm cranially to intersection of internal thoracic artery and recurrent laryngeal nerve [5].
The knowledge of the course of inferior thyroid artery is important mainly for endocrine surgeons, for the proper performance of surgical removal of pathologically changed thyroid gland (thyroidectomy) or parathyroid adenoma or carcinoma (parathyroidectomy). During thyroidectomy, the inferior thyroid artery must be ligated. In both procedures, preservation of the recurrent laryngeal nerve is absolutely crucial. Contusion and/or neurotmesis of the recurrent laryngeal nerve, resulting in a vocal cord paralysis, are usually estimated as the most important complicating factors of the thyroid and parathyroid surgery [6,7]. Atypical branching of vessels can cause intra-operative bleeding and/or postoperative hematoma. Damage of inferior thyroid artery can lead to ischemia of all ipsilateral parathyroid glands [2,8].
Acknowledgements
The author thanks to Ivana Vítková, MD, for the opportunity to perform a dissection study on the Department of Pathology, First Faculty of Medicine, Charles University, Prague. This study was supported by grants IGA MZ NR/8308-5 and MZ ČR č. 64203.
References
- Adamek S, Libansky P, Nanka O, Sedy J, Pafko P. [Surgical therapy of primary hyperparathyroidism and it’s complications. Experience with 453 patients]. Zentralbl. Chir. 2005; 130: 109–113. German.
- Nanka O, Sedy J, Vitkova I, Libansky P, Adamek S. Surgical anatomy of parathyroid glands with emphasis on parathyroidectomy. Prague Med. Rep. 2006; 107: 261–272.
- Ziolkowski M, Bieganska-Dembowska D, Kurlej W. Variations in the number and in origin of the thyroid arteries. Folia Morphol. (Warsz) 1994; 53: 105–110.
- Krudy AG, Doppman JL, Brennan MF. The significance of the thyroidea ima artery in arteriographic localization of parathyroid adenomas. Radiology. 1980; 136: 51–55.
- Bonjer HJ, Bruining HA. Technique of parathyroidectomy. In: Clark O, Duh HQ, eds. Textbook of endocrine surgery. 1st Ed., Philadelphia, W.B. Saunders Company. 1997; 347–356.
- Carty SE. Prevention and management of complications in parathyroid surgery. Otolaryngol. Clin. North Am. 2004; 37: 897–907.
- Fewins J, Simpson CB, Miller FR. Complications of thyroid and parathyroid surgery. Otolaryngol. Clin. North Am. 2003; 36: 189–206.
- Libansky P, Astl J, Adamek S, Nanka O, Pafko P, Spackova J, Foltan R, Sedy J. Surgical treatment of primary hyperparathyroidism in children: Report of 10 cases. Int. J. Pediatr. Otorhinolaryngol. 2008; 72: 1177–1182.
Jiri Sedy*
Institute of Experimental Medicine, Academy of Sciences of the Czech Republic, Prague, Czech Republic.
- *Corresponding Author:
- Jiri Sedy, MD
Institute of Experimental Medicine, Academy of Sciences of the Czech Republic, Videnska 1083, 142 20, Prague 4, Czech Republic.
Tel: +420 241062717
Fax: +420 241062783
E-mail: jirisedy@hotmail.com
Date of Received: June 24th, 2008
Date of Accepted: July 18th, 2008
Published Online: July 19th, 2008
© IJAV. 2008; 1: 10–11.
Abstract
We report a case of an incidental finding of the right accessory inferior thyroid artery, emerging from the thyrocervical trunk together with a typical inferior thyroid artery, present in a normal position. On the left side, only single inferior thyroid artery was present. Only one inferior thyroid vein was found on each side. The accessory inferior thyroid artery entered the thyroid gland approximately 1 cm above the normal inferior thyroid, above the superior parathyroid gland. Although accessory vessels of thyroid gland are present in about 5% of cases, the accessory inferior thyroid artery, emerging from subclavian artery and located above the normal inferior thyroid artery, is very rare.
-Keywords
inferior thyroid artery, variability, accessory, anatomy
Introduction
Inferior thyroid artery is one of the main arteries supplying thyroid gland and laryngeal muscles. It also supplies pharynx, esophagus, trachea and thymus. It emerges from the thyrocervical trunk of the subclavian artery at the level of C6 vertebra. Then, it rapidly curves inferomedially, crossing the bundle of common carotid artery, internal jugular vein and vagus nerve. Further, it continues to lower pole of the thyroid gland, crossing the recurrent laryngeal nerve. The main branches of inferior thyroid artery are inferior laryngeal artery, supplying mainly laryngeal musculature; glandular branches, supplying thyroid gland; and branches entering pharynx, esophagus, trachea and thymus. The knowledge of the anatomy of the inferior thyroid artery is important for neck surgeons, mainly during operations on thyroid and parathyroid glands [1,2].
Case Report
During the training of parathyroidectomy on cadavers at the Department of Pathology, First Faculty of Medicine, Charles University, Prague; in an adult male, where pathology of neck structures have been excluded, an accessory inferior thyroid artery was observed. On neck, collar skin incision followed by midline incision and sternotomy was performed. Thorax was opened. Superficial neck fascia was cut in midline; infrahyoid muscles pulled laterally, lobes of the thyroid gland were detached from surrounding structures and pulled medially. Both recurrent laryngeal nerve and inferior thyroid artery were cleaned. Parathyroid glands were found close to the site of crossing of recurrent laryngeal nerve and inferior thyroid artery. On the right side, doubled inferior thyroid artery was found (Figure 1), both arising separately from thyrocervical trunk. The lower artery was in a typical location, whereas the upper was recognized as accessory. On the left side, only single inferior thyroid artery was present. Only one inferior thyroid vein was found on each side. Preparation continued on the dorsal surface of thyroid gland, under the capsule of thyroid gland, along the course of recurrent laryngeal nerve and inferior thyroid artery, in the cervical and mediastinal lipothymic tissue, in the anterior mediastinum and in the parapharyngeal and the paraesophageal space. Four parathyroid glands were found in typical localization, close to the crossing of inferior thyroid artery and recurrent laryngeal nerve. All four parathyroid glands were verified histologically - samples were removed, put in 4% paraformaldehyde, dehydrated in alcohol series of ascending concentration, embedded to paraffin, cut to 10 μm section, stained with hematoxyline-eosin and analyzed with optic microscope.
Figure 1: Dissection of the neck showing accessory inferior thyroid artery, right side view, thyroid gland shifted medially. (Full white arrows: Doubled right inferior thyroid arteries, the superior one is the accessory inferior thyroid artery, white arrowheads: parathyroid glands, black arrowheads: recurrent laryngeal nerve, black arrows: inferior thyroid vein)
Discussion
Anatomical variability of neck vasculature is quite high. Venous variability is much higher than arterial. Arteries of the thyroid and parathyroid glands include superior thyroid artery, emerging from external carotid artery and inferior thyroid artery, emerging from the thyrocervical trunk. In a small percentage of cases, anomalous arteries to the thyroid occur [3]. The most important anatomical variety of thyroid arteries is the thyroidea ima artery, present in 1.5% - 12.2% of cases. In majority of cases, it emerges from brachiocephalic trunk, less often from right common carotid artery, aortic arch, internal thoracic artery or left common carotid artery [4]. Accessory inferior thyroid artery emerging from subclavian artery is very rare and often present more caudally to the inferior thyroid artery. The accessory inferior thyroid artery thus rather represents a rare variety of the thyroidea ima artery, emerging from subclavian artery than a typical accessory inferior thyroid artery. In our case, the inferior thyroid artery, which we recognized as normal, had a typical course and relation to surrounding structures, including recurrent laryngeal nerve and parathyroid glands, which were subsequently verified histologically. Normal anatomical position of parathyroid glands was defined previously by Bonjer and Bruining as the presence of demanded parathyroid glands within a circumscribed area 2 cm in diameter, 1 cm cranially to intersection of internal thoracic artery and recurrent laryngeal nerve [5].
The knowledge of the course of inferior thyroid artery is important mainly for endocrine surgeons, for the proper performance of surgical removal of pathologically changed thyroid gland (thyroidectomy) or parathyroid adenoma or carcinoma (parathyroidectomy). During thyroidectomy, the inferior thyroid artery must be ligated. In both procedures, preservation of the recurrent laryngeal nerve is absolutely crucial. Contusion and/or neurotmesis of the recurrent laryngeal nerve, resulting in a vocal cord paralysis, are usually estimated as the most important complicating factors of the thyroid and parathyroid surgery [6,7]. Atypical branching of vessels can cause intra-operative bleeding and/or postoperative hematoma. Damage of inferior thyroid artery can lead to ischemia of all ipsilateral parathyroid glands [2,8].
Acknowledgements
The author thanks to Ivana Vítková, MD, for the opportunity to perform a dissection study on the Department of Pathology, First Faculty of Medicine, Charles University, Prague. This study was supported by grants IGA MZ NR/8308-5 and MZ ČR č. 64203.
References
- Adamek S, Libansky P, Nanka O, Sedy J, Pafko P. [Surgical therapy of primary hyperparathyroidism and it’s complications. Experience with 453 patients]. Zentralbl. Chir. 2005; 130: 109–113. German.
- Nanka O, Sedy J, Vitkova I, Libansky P, Adamek S. Surgical anatomy of parathyroid glands with emphasis on parathyroidectomy. Prague Med. Rep. 2006; 107: 261–272.
- Ziolkowski M, Bieganska-Dembowska D, Kurlej W. Variations in the number and in origin of the thyroid arteries. Folia Morphol. (Warsz) 1994; 53: 105–110.
- Krudy AG, Doppman JL, Brennan MF. The significance of the thyroidea ima artery in arteriographic localization of parathyroid adenomas. Radiology. 1980; 136: 51–55.
- Bonjer HJ, Bruining HA. Technique of parathyroidectomy. In: Clark O, Duh HQ, eds. Textbook of endocrine surgery. 1st Ed., Philadelphia, W.B. Saunders Company. 1997; 347–356.
- Carty SE. Prevention and management of complications in parathyroid surgery. Otolaryngol. Clin. North Am. 2004; 37: 897–907.
- Fewins J, Simpson CB, Miller FR. Complications of thyroid and parathyroid surgery. Otolaryngol. Clin. North Am. 2003; 36: 189–206.
- Libansky P, Astl J, Adamek S, Nanka O, Pafko P, Spackova J, Foltan R, Sedy J. Surgical treatment of primary hyperparathyroidism in children: Report of 10 cases. Int. J. Pediatr. Otorhinolaryngol. 2008; 72: 1177–1182.