An Unusual Case of Accessory Spleen Found During Laparoscopic Surgery: A Clinical Anatomy Case Report
Received: 24-Mar-2023, Manuscript No. ijav-23-6234; Editor assigned: 27-Mar-2023, Pre QC No. ijav-23-6234 (PQ); Accepted Date: Apr 14, 2023; Reviewed: 10-Apr-2023 QC No. ijav-23-6234; Revised: 14-Apr-2023, Manuscript No. ijav-23-6234 (R); Published: 21-Apr-2023, DOI: 10.37532/1308-4038.16(4).255
Citation: Karl M. An Unusual Case of Accessory Spleen Found During Laparoscopic Surgery: A Clinical Anatomy Case Report. Int J Anat Var. 2023;16(4):284-284.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Accessory spleens are rare anatomical variants that can be found in up to 16% of the population. They are usually discovered incidentally during radiologic imaging or autopsy. However, they can also be encountered during surgical procedures, especially laparoscopy. Here we present a case of an accessory spleen found during laparoscopic surgery for an unrelated condition. The patient was a 43-year-old female with a history of chronic pelvic pain who underwent laparoscopic surgery for endometriosis. During the procedure, an accessory spleen was found near the splenic hilum. The anatomy and function of accessory spleens are discussed, along with their clinical relevance and potential implications for laparoscopic surgery.
Keywords
Laparoscopic surgery; Spleen; Fetal; Splenic hilum
INTRODUCTION
Accessory spleens are small, ectopic nodules of splenic tissue that are separate from the main spleen. They are thought to arise from embryonic splenic tissue that fails to migrate to the left upper quadrant during fetal development. Accessory spleens are usually asymptomatic and are discovered incidentally during radiologic imaging or autopsy [1-2]. However, they can also be encountered during surgical procedures, especially laparoscopy. While accessory spleens are generally benign and do not require treatment, their presence can have clinical implications for certain surgical procedures, including splenectomy and laparoscopic surgery [3].
CASE REPORT
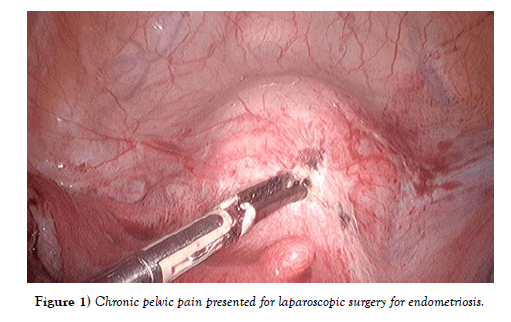
A 43-year-old female with a history of chronic pelvic pain presented for laparoscopic surgery for endometriosis. During the procedure, the surgeon identified a small nodule near the splenic hilum. After careful dissection, it was determined that the nodule was an accessory spleen. The accessory spleen was removed and sent for pathological examination, which confirmed the diagnosis. The patient had an uneventful recovery and was discharged home the following day [Figure 1].
Figure 1) Chronic pelvic pain presented for laparoscopic surgery for endometriosis.
DISCUSSION
Accessory spleens are relatively common anatomical variants, occurring in up to 16% of the population [4-5]. While they are usually asymptomatic and do not require treatment, their presence can have clinical implications for certain surgical procedures. For example, accessory spleens can be mistaken for lymph nodes during lymph node dissection, leading to incomplete removal of the accessory spleen. Similarly, accessory spleens can be mistaken for a tumor or metastasis during laparoscopic surgery, leading to unnecessary procedures or delays in diagnosis [6-7].
CONCLUSION
The presence of accessory spleens is an important consideration during laparoscopic surgery. Surgeons should be aware of the anatomy and potential locations of accessory spleens, especially near the splenic hilum. In cases where an accessory spleen is identified, careful dissection and removal are recommended to prevent confusion with other structures and ensure complete removal.
ACKNOWLEDGEMENT:
None.
CONFLICTS OF INTEREST:
None.
REFERENCES
- Brian M, Jared PB, Laura E. Thoracic surgery milestones 2.0: Rationale and revision. J Thorac Cardiovasc Surg. 2020 Nov; 160(5):1399-1404.
- Amy LH, Shari LM. Obtaining Meaningful Assessment in Thoracic Surgery Education . Thorac Surg Clin. 2019 Aug;29(3):239-247.
- Kuo-Shyang J, Shu-Sheng L, Chiung-FC. The Role of Endoglin in Hepatocellular Carcinoma. Int J Mol Sci. 2021; 22(6):3208.
- John C, Christian J. Commentary: Thoracic surgery residency: Not a spectator sport. J Thorac Cardiovasc Surg. 2020 Jun; 159(6):2345-2346.
- Anri S, Masayoshi O, Shigeru H. Glomerular Neovascularization in Nondiabetic Renal Allograft Is Associated with Calcineurin Inhibitor Toxicity. Nephron. 2020; 144 Suppl 1:37-42.
- Mamikonyan VR, Pivin EA, Krakhmaleva DA. Mechanisms of corneal neovascularization and modern options for its suppression. Vestn Oftalmo. 2016; 132(4):81-87.
- Farid MS, Kristin W, Gilles B. The History and Evolution of Surgical Instruments in Thoracic Surgery. Thorac Surg Clin. 2021 Nov; 31 (4): 449- 461.
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at , Google Scholar , Crossref
Indexed at, Google Scholar, Crossref
Indexed at , Google Scholar, Crossref
Indexed at , Google Scholar, Crossref