Analysis of maxillofacial and neck spaces infection in diabetic and non-diabetic patients
2 Department of Periodontal, IBB University, Yemen, Email: dentist123@gmail.com
Received: 26-Feb-2018 Accepted Date: Mar 17, 2018; Published: 30-Mar-2018
Citation: Holkom MA, Fu-Qiang X, Alkadasi B, et al. Analysis of Maxillofacial and Neck Spaces Infection in Diabetic and Non Diabetic Patients. J Dent Oral Res 2018;2(1):7-14.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
PURPOSE: Before the advent of antibiotics, upper respiratory infections were the most common, but now the prevalence of odontogenic infection is on the increase in spite of developments in medicine and improvements in dental care. So, the aim of this study is to analyze the maxillofacial spaces' infection, especially those with dental origin in diabetic patients, in comparison with non-diabetic patients.
MATERIALS AND METHODS: This was a 4 years retrospective study from June 2013 to December 2016. The authors analyzed 120 cases which were treated for oro-facial spaces infections. The cases were divided into two groups: diabetic (Group-A), which included 47 patients and non-diabetic (Group-B), which included 73 patients. We compared the patients’ demography, chief complaints, laboratory values (Wbcs, microbiology), sources of infection (odontogenic, non-odontogenic) and the types of space and treatments (tooth involved, surgical approaches, complications and duration of hospital stay). Statistical analyses in both groups were conducted utilizing Student’s t test, Chi square test, and ANOVA test utilizing SPSS (IBM SPSS statistics 21 version).
RESULTS: Among the study population, 55% were female and 45.0% were male. WBCs in diabetic patients at admission time were higher than in non-diabetic patients, which was significantly (p=0.041). The diabetic patients were admitted to hospital later than non-diabetic patients p=0.0001, with more multiple spaces infection. The diabetic patients underwent more surgeries (p=0.017) underwent hospitalization and had more complications. In this study, no patient died from both groups.
CONCLUSION: For good prognosis the tooth involved should be as soon as possible treated to minimize possibility of infection recurrent.
Keywords
Maxillofacial spaces; Treatment; Diabetic; Complication; Antibiotics; Bacteria.
In the second century, cases of deep neck infection (DNI) were described and recognized by the gallon [1]. Infection of the deep neck has been known under some names, including angina, suffocation and malignant cancer [2]. Maxillofacial spaces have been defined and described by Urns in 1811 as potential spaces between the layers of Fascia. These spaces are filled with loose connective tissues and numerous anatomical structures like veins, arteries, glands, and lymph nodes [3-5].
Oro-facial infection can be spread by direct contact through tissue, lymphatic system or by blood stream. Various factors contribute to the spread of infection which can be divided into general and local factors. The general factors include (host resistance, virulence of the micro-organism and compromised host defenses. The local factors depend on a balance between host resistance and bacterial pathogenicity [6]. The most common primary sources of oro-facial infection are dentition, tonsils, salivary glands and retained foreign bodies [7-9]. Prior to the use of antibiotics, 70% of cases of DNS were either tonsilla or peritonsillar infection, but now the most common cause originates from the dental region [10]. Early Egyptians were noticed with signs of dental abscesses and evidence signifies osteomyelitis [11]. At the beginning of the 20th century, dental infections were associated with a mortality rate of 10–40%, but this percentage declined after the use of antibiotics. Odontogenic infections have been one of the most common diseases in the oral and maxillofacial regions especially in developing countries [12-14]. Periapical lesion and periodontal lesion are considered as the foremost dental causes of facial infection which may arise as an iatrogenic complication of tooth extraction or local anesthesia [15]. According to Zamiri, et al., [11], the periapical lesion is the most common one. On the other hand, Jansisyanont, et al., [16], reported dental caries as the most frequent cause of odontogenic infection. Odontogenic abscess, which extends into masticatory spaces, is a sequence indicated by facial pain, swelling, and truisms [17]. The higher rates of odontogenic infections, such as Ludwig’s angina, result from low socio-economic status and poor oral hygiene [18]. Maxillofacial infection may range from low-grade, localized (self-limiting) to severe, lifethreatening infections, which spread downward to the mediastinum, pleural cavities, and pericardium [19]. The mortality ratio can reach 40-50% in circumstances involving mediastinitis. The most feared complication from a retropharyngeal extension of infection into the posterior mediastinum is descending necrotizing mediastinitis [20]. A patient with poorly controlled Diabetes mellitus (DM) faces the likelihood of virulent bacterial and fungal infections [21-24]. According to “Diabetes mellitus related to degenerative complications comprise of micro angiopathy, macroangiopathy, and neuropathy [25]. Lower production of interleukins in response to infection; reduces chemotaxis and phagocytic activity, immobilization of polymorphonuclear leukocytes and dysfunction in neutrophil bactericidal function, cellular immunity, and complement activation. For this reason, diabetic patients tend to have a higher incidence and increased severity of infections than non-diabetic patients [26]. Continuity of recurrent infection in systemic complication with diabetes patients occur as a result of impaired host defense [27]. The risk of mortality related to infection in a diabetic adult patient is greater than that of a cardiovascular disease patient [28]. Deep neck infection in diabetic patients when compared with the non-diabetic patients have many differences. It was reported that diabetic patients have more complications than other populations when it comes to deep facial infections and extended stay in hospital [29]. Before the use antibiotics, upper respiratory infections were most common but now odontogenic infection is most prevalent in spite of developments in medicine and improvements in dental care. So, this study was designed to analyze the maxillofacial spaces infection, especially originating from dental origin, in diabetic patients and compare them with non-diabetic patients and to share our experiences regarding presentations, common sites involved, clinical trends, management, bacteriology, complications, and outcomes.
Patients and Methods
Study design and sample
This is a retrospective (cohort study) in which we analyzed 120 treated cases admitted to the department of maxillofacial surgery in the second hospital of Lanzhou University in Lanzhou city of Gansu province in China, between June 2013 and December 2016. The cases were divided into two groups: diabetic (Group-A) included 47 patients and non-diabetic (Group-B) included 73 patients. Patients who were diagnosed with oro-facial spaces infection that originated from the upper respiratory or odontogenic infection and were treated as in-patients. Patients who had an infection related to malignancy, inhalant injuries or had not enough information, or treated as outpatients were excluded from this study. The state of the patient determines the treatment to be offered when the patient arrives in our department, we do ordinary examination such as extra-oral, intra-oral, laboratory and radiographic examinations. The diabetic group of patients arrive with a recognized history of diabetes, or diagnosed with blood sugar level above 7 mol/L fasting. Those with regular blood glucose concentrations or less than of 7 mol/L while glucose level fasting at the time of admission, and those with no past medical history of Diabetes mellitus were included in the non-diabetic group. The diabetic patient, controlling his blood sugar is very important to obtain a good result with less complication. According to that, we can estimate the seriousness of a patient’s condition so as to choose the suitable treatment. Some patients came to our department with serious complications like sever truisms, dyspnea, Ludwig angina, and mediastinitis; those patients underwent surgery (incision and drainage) on the first day. The previous protocol had been applied for the patient who arrived with an abscess. Aspiration and intravenous antibiotic and observation for 48 hours have been applied for patients who came with normal fever and without abscess. If the patient’s condition, during 48 hours improves we continue giving him the drug. But if the condition deteriorates with temperature increasing, infection extending, abscess forming we recommend doing CT scan to determine the space involved after that patient underwent surgery. This study has been approved by the Medical Ethical Committee of Lanzhou University.
Variables
To distinguish between the two groups of diabetic (Group-A) and non-diabetic (Group-B) patients with severe multi-space infections in the head and neck regions, we compared variables such as patients information, etiology of the condition, clinical variables, laboratory values, and treatments.
Data collection
Data collection included demography (age, sex, and address ), chief complaint, history of pain, clinical feature, intra-oral examination, routine blood test (WBC, platelets count, HB test, PT, TT test), some biochemistry test, social habits (smoking and alcoholic drinking), and information on associated diseases, type of bacteria (specimen cultures were taken from some patients under local or general anaesthesia for three consecutive days either by aspiration or by swabbing of open wounds) source of infection (odontogenic, non-odontogenic) site of infection (maxilla, mandible or both and right or left), number of teeth, type of spaces involved in infection (primary or multiple spaces) type of antibiotic, type of treatment (use of antibiotics alone or with incision and drainage) type of anesthesia (general, local), time of incision, period of stay in hospital, calculating the period from first incident into admission date, and complication.
Data analysis
The data of the 120 cases included 47 (Group-A) diabetic patients and (Group-B) non-diabetic included 73 patients were analyzed using SPSS (IBM SPSS statistics 21 version). We performed a descriptive statistical analysis. We used t-test and chi-square test to compare between the two groups and to evaluate the significance of the difference between them, with differences set to be significant if the p value is less than 0.005.
Results
Demographic status of a patient
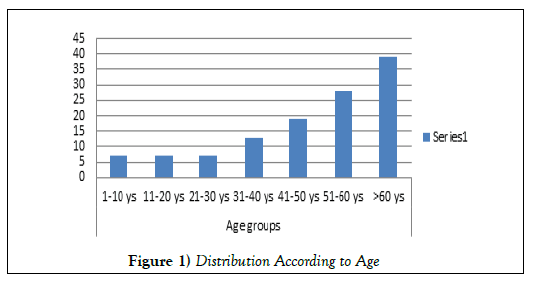
The mean age in Group-A (diabetic patients) was 55 ± 18.039 years, with minimum as nine years and maximum 82 years. The mean age in Group-B was 47.10 ± 20.951 years, with minimum as four years and maximum 92 years. The age difference between the two groups was statically significant (P=0.036). From among the study population, 55% were female (25 Group-A, 41 Group-B) and 45.0% were male (22 from Group-A, 32 from Group-B). About 65% of the sample came from rural areas, and 35% from urban settings. A majority of 72.5% patients had no occupation while those with occupations were engaged in different jobs such as farming (15%,). There are students (10%) and some (2.5%) who have no fixed jobs. Most of the patients were from HAN ethnic group which form 85% of the population as (80.9%) patients were from Group-A and (87.7%) patients were from group B. The second ethnic group, HUI forms 10.8% of the population with patients from both (12.8%) and (9.6%) are of group B. The third ethnic group is DONG XIAN group which form in this research 2.5% of the population with patients from (2.1%) from Group-A, (2.7%) and from Group-B. ZANG, the fourth ethnic group forms 1.7 of the population with patients from (4.3%) group-A and none from group-B (Figure 1).
Disease period
In this study, we refer to the disease’s period as the date of incidence, date of hospitalization, and date of discharge from the hospital. The mean of an interval between the date of infection and date of hospitalization in Group-A was 9.04+13.275 days, with minimum one day as and 61 days as maximum. In Group B, the mean was 8.73+9.506, with one day as minimum and 61 days as maximum p=0.001 was significant. The mean of an interval between the date of hospitalization and date of discharge in Group-A was 10.51+6.295, with a minimum of three days and a maximum of 36 days. In Group B the mean was 9.25+4.471 with a minimum of five days and a maximum of 22 days. No significant between two groups p=199.
Pre-hospitalization treatment
About 45.0% of patients consumed medications on their own before admission to hospitals. About 68.3%went to local hospital or clinics to receive treatment with comprising both from Group-A (74.5%) and Group B (64.4%) patients. In the hospital, some patients 53.3% were treated with medicine and 2.5% were treated with surgery (I & D), while 5.8% were treated with combination of drug and surgery. Drug & Root canal treatment was given to 2.5% of patients.
Chief complaint
In the case of most of the patients (45.8%) from both groups the chief complaint was swelling and pain while in 39.2% the complaint was restricted to some 8.3% suffered from pain, swelling and toothache. Swelling and difficulty swallowing were seen in 2.5%. Pain was the complaint in 1.7%, pain, swelling and difficulty opening mouth were observed in 1.7% of patients and 0.8% suffered from toothache (Table 1).
| Pain history | Group A (n) | Group B (n) | Total 100% | |
|---|---|---|---|---|
| Toothache | 2 | 2 | 4.1% | |
| Toothache, use drug by self, go to clinic | 13 | 15 | 23.3% | |
| Toothache and use drug | 8 | 16 | 20.0% | |
| Toothache and go to clinic | 19 | 20 | 32.5% | |
| Toothache, swelling, difficulty swallowing and go to clinic | 0 | 3 | 2.5% | |
| Swelling and pain | 0 | 5 | 4.2% | |
| Swelling, pain and use drug | 2 | 3 | 4.2% | |
| Swelling, pain and go to clinic | 2 | 6 | 6.7% | |
| Swelling, use drug and go to clinic | 1 | 2 | 2.5% | |
| total | 47 | 73 | 120 100% | |
| Clinic feature | Group A(n) | Group B(n) | Total 100% | |
| Color of skin | Normal | 19 | 42 | 50.8% |
| Redness | 27 | 29 | 46.7% | |
| flushing | 1 | 2 | 2.5% | |
| 120 100% | ||||
| asymmetry | yes | 45 | 71 | 96.7% |
| no | 2 | 2 | 3.3% | |
| 120 100% | ||||
| Border clear | Yes | 13 | 14 | 22.5% |
| no | 34 | 59 | 77.5% | |
| 47 | 73 | 120 100% | ||
| Mobility | Yes | 12 | 19 | 25.8% |
| no | 35 | 54 | 74.2% | |
| 120 100% | ||||
| Fixed | Yes | 27 | 43 | 58.3% |
| no | 20 | 30 | 41.7% | |
| 120 100% | ||||
| Pain in touch | Yes | 35 | 45 | 66.7% |
| no | 12 | 28 | 33.3% | |
| 120 100% | ||||
| High Skin temperature | Yes | 36 | 45 | 67.5% |
| no | 11 | 28 | 32.5% | |
| 120 100% | ||||
| Difficulty opining | Yes | 37 | 50 | 72.5% |
| no | 10 | 23 | 27.5% | |
| 120 100% | ||||
| Numbness | Yes | 3 | 1 | 3.3% |
| no | 44 | 72 | 96.7% | |
| 120 100% | ||||
| Intra oral seen | Yes | 34 | 63 | 80.8% |
| no | 13 | 10 | 19.2% | |
| 120 100% | ||||
| Gingivitis | yes | 34 | 50 | 70% |
| No | 1 | 13 | 11.7% | |
| Not see | 12 | 10 | 22% | |
| 120 100% | ||||
| Intra oral fistula | Yes | 8 | 8 | 13.3% |
| No | 26 | 55 | 67.5% | |
| Not see | 13 | 10 | 19.2% | |
| 120 100% | ||||
| Occlusal normal | Yes | 23 | 58 | 75.0 |
| No | 2 | 5 | 5.8 | |
| Not see | 13 | 10 | 19.2 | |
| 120 100% | ||||
| Lost teeth | Yes | 19 | 20 | 32.5% |
| No | 15 | 43 | 48.3% | |
| Not see | 13 | 10 | 19.2% | |
| 120 100% | ||||
| Swelling floor of mouth | Yes | 7 | 12 | 15.8% |
| No | 28 | 51 | 65.8% | |
| Not see | 12 | 10 | 18.3% | |
| 120 100% | ||||
| Prosthesis appliance | Yes | 11 | 8 | 15.8% |
| No | 24 | 55 | 65.8% | |
| Not see | 12 | 10 | 18.3% | |
| 120 100% |
Table 1: History of pain and clinical features
Eighty-six samples of pus were taken for culture examination from the two groups, which included 38 samples from the diabetic group, and 48 from the non-diabetic group. These samples were collected by incision and drainage or aspiration. The growth results were obtained in 41 samples (21 from Group-A and 20 from Group-B). Forty-six had no growth (17 from Group-A and 28 from Group-B). Streptococcus spp. was found as the most prevalent bacteria in the two groups (Table 2).
| Type of bacteria | Diabetic group A(n=47) | Non diabetic group B(n=73) | Total (n=120) |
|---|---|---|---|
| Streptococcus hemolytic | 6 (12.3%) | 3 ( 4.1%) | 7.5% |
| Streptococcus viridance | 14 (29.8%) | 15 (20.5%) | 24.2% |
| Proteus mirabilis | 0 (0.0%) | 1 (1.4%) | 0.8% |
| Staphylococcus aureus | 0 (0.0%) | 1 (1.4%) | 0.8% |
| Grace green streptococcus | 1 (2.1%) | 0 (0.0%) | 0.8% |
Table 2: Bacteriology
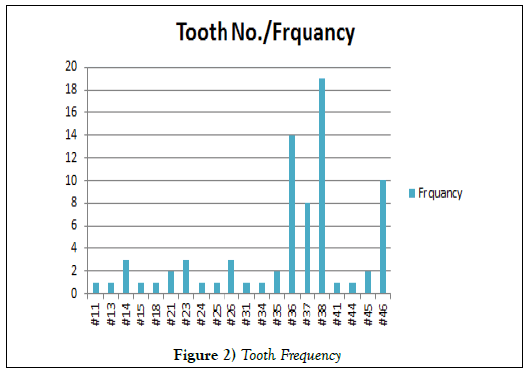
Odontogenic infection was considered the most common cause of maxillofacial spaces infection in both groups which formed 90% from all cases in our study. While non-odontogenic causes were found in 10%, odontogenic formed 93.6% cases in Group-A and 87.7% cases in Group-B. Most of the cases occurred on the right side of the mandible 45.0%, 46.8%in Group-A and 43.8%in Group-B. And left side form 40.0%; 36.2%in Group-A and 42.4%in Group-B. Which upper of jaw form 15.0% left side more than right side 6.4% in Group-A and 9.6% in Group-B. Right side in Group-A 8.5% and from Group-B 6.8%. Conversely, with some previous studies, we did not find any cases with unknown causes (Table 3 and Figure 2).
| Origin of infection | Group A(n=47) | Group B(n=73) | Total (n=120) | ||
|---|---|---|---|---|---|
| Non odontogenic | Lymphatic organ | 3 (6.4%) | 6 (8.2%) | 7.5% | |
| Others | 0 (0.0%) | 3 (4.1%) | 2.5% | ||
| Odontogenic dental causes | Caries | 7 (14.9%) | 17 (23.3%) | 20.0% | |
| Postoperative | 0 (0.0%) | 5 (6.8%) | 4.2% | ||
| Periapical lesion | 19 (40.4%) | 14 (19.2%) | 27.5% | ||
| Caries & preapiacal lesion | 5 (10.6%) | 9 (12.3%) | 11.7% | ||
| Residual root | 0 (0.0%) | 2 (2.7%) | 1.7% | ||
| Odontogenic Periodontal causes | periodentitis | 7 (14.9%) | 10 (13.7%) | 14.2% | |
| periocoronitis | 2 (4.3%) | 3 (4.1%) | 4.2% | ||
| impacted teeth | 4 (8.5%) | 6 (8.2%) | 8.3% | ||
| Periodontal & impacted teeth | 1 (2.1%) | 0 (0.0%) | 0.8% | ||
Table 3. Causes of deep neck infections
Spaces involvement
We divided spaces in this study into two categories; single space and multiple spaces (more than one space). In our study, we found 53.3 cases % were multiple spaces with 63.8% cases in a diabetic Group and 46.6% cases in non-diabetic Group. Single space form 46.7%, of which 36.2% were in the diabetic group, and 53.4% cases in the non-diabetic group. The submandibular and buccal spaces were the most common in both groups. Multiple spaces infection it is more evident in the diabetic group which forms 63.8% (Table 4).
| Location | Diabetic group A(n=47) | Non diabetic group B(n=73) |
|---|---|---|
| submandibular | 28 (59.6%) | 33 (45.2%) |
| Buccal | 18 (38.3%) | 33 (45.2%) |
| Masseteric | 14 (29.8%) | 18 (24.7%) |
| Sublingual | 10 (21.3%) | 10 (13.7%) |
| Infraorbital | 10 (21.3%) | 8 (11.0%) |
| Pterygomandibular | 3 (6.4%) | 9 (12.3%) |
| Lateralpharngial | 4 (8.5%) | 5 (6.8%) |
| Submental | 5 (10.6%) | 4 (5.5%) |
| Canine | 3 (6.4%) | 3 (4.1%) |
| Infratemporal | 3 (6.4%) | 3 (4.1%) |
| Parotid | 2 (4.3%) | 1 (1.4%) |
| Retropharngial | 1 (2.1%) | 3 (4.1%) |
Table 4. Neck-facial infection sites
Radiographical examination
Most of patients underwent panoramic x-ray, 32.5% 18 (38.3%) from Group-A, 41 (28.8%) from Group-B. CT scan formed 30.0% with 12 (25.5%) from Group-A, 24 (32.9%) from Group-B. CT scan and panoramic x-ray constituted 16.7% with 9 (19.1%) from Group-A and 11 (15.1%) from Group-B. MRI was done for two patients, ultrasound was done for one patient, CT scan with chest x-ray for three patients and CT scan and MRI were performed for one patient.
Treatment
Treatment constituted mostly extraction of teeth (51.1%), root canal (30.8%), periodontal treatment (6.7%), periodontal and extraction for (0.8%). We made tracheotomy for seven cases; four (8.5%) from Group-A, three (4.1%) from Group-B with no significant differences between both groups. We did surgery once for 78.3%, and twice for 2.5% patients from both groups. Most of the surgery was performed on the first day (33.3%) on the second day 24.2% and on the third day 16.7% underwent surgery. Local anesthesia used on 70.8% patients with 72.3% from Group-A and 69.9% from Group-B. General anesthesia constituted 10.0% with 17.0% from in Group-A and 5.5% from Group-B patients. Surgical approaches from extra oral were formed on 55.0% patients with 63.8% from Group-A and 49.3% cases from Group-B. Ceftriaxone antibiotic (IV) was mostly prescribed in both the groups (43.3%) and ceftriaxone with ornidazole on 36.7% patients and some patients (50%) were given ceftriaxone with metronidazole.
Complication & outcome
About 72.5% of patients from the two groups had complication before treatment; 78.7% from Group-A and 68.5% from Group-B. The follow up was very good in the years following our study and so the mortality rate was zero (Table 5).
| Complications | Group A (n=47) | Group B (n=73) | Total (n=120) | |
|---|---|---|---|---|
| Trismus | 38 (80.9%) | 50 (68.5%) | 73.3% | |
| Dysphagia | 12 (25.55) | 13 (17.3%) | 20.8% | |
| Dyspanea | 4 (8.5%) | 4 (5.5%) | 6.7% | |
| Phonation change | 4 (8.5%) | 2 (2.7%) | 5.0% | |
| Tongue elevation | 3 (6.4%) | 2 (2.7%) | 4.2% | |
| Mediastnitis | 1 (2.1%) | 3 (4.1%) | 3.3% | |
| Ludweg angina | 1 (2.1%) | 0 | 0.8% | |
Table 5. Complications of deep neck and facial infections
DISCUSSION
Despite the availability of effective antibiotic, development of sophisticated protocols, and surgical techniques, the deep and facial spaces of infection remain one of the most severe emergencies faced daily by dentists and otolaryngologists. Diabetes mellitus (DM) is considered a major community health problem worldwide. In China, the incidence of diabetes is about 9.7% of the total population [30]. DM is documented as the most common systemic disease that is associated with deep neck infections. The incidence and severity of infection can exacerbate in a patient with poor controlled blood sugar. The difficulty in controlling infection, and poor progress of wound healing in Diabetes mellitus is related to many alterations in hematologic such as red cell aggregation, red cell deformity, plasma viscosity, and 2, 3 diphosphoglycerate concentrations leading to poorly controlled diabetes. Diabetic not only face high hazard where infection is concerned but they are also believed to often react poorly to infection [31].
The diabetic patient’s age in our study was more in order than non-diabetic patients which was significantly p<0.036 (chi-square test, ANOVA test T-test) which coincides with previous studies [32] and Rao et al. Study reported to be insignificant. Aging patients are highly vulnerable to declined immune function, mostly T cell-mediated activity, which contributes to increased infection [33]. Also diabetic patients are more susceptible to infection as a result of degenerative complications in the immune system, especially if blood sugar is not controlled.
In addition, xerostomia increasing in elderly patients leads to a high incidence of dental caries and salivary gland diseases [34]. In our study had more female patients than male, whereas other previous studies have shown a male domination or slightly equal distribution. Hong-Ying et al. [35] reported that caries were high in female than male patients; it is so for old people also from rural areas. In this study, the HAN ethnic group form about 85% of the cases which form 93% of the Chinese population [36]. In this study most of the patients came from the Ural but, statistically not significant. Das R, G Nath, and A Mishra reported that the rural distribution was significant.
The sources of maxillofacial space infections were 90% due to odontogenic causes in both groups; the second cause was lymphatic organ. This result is similar to many previous studies. However, this study does not have cases with unknown sources which disagree with other studies [37,38]. Caries was the most reported cause for deep neck and facial spaces infections while Marioni et al. reported that periapical infection was often causing facial spaces infections. In this study, the periapical lesion was found to be principal cause. Recently, odontogenic origin has been considered to be the most common cause which results from poor oral hygiene, patient indifference, high-cost dental treatment, which is not covered by insurance. Also, a patient with dental problem always depends on self-medication or a doctor to relieve only the pain and not for treating the cause. So he/she comes for treatment advanced stages of the disease.
In this study, the lower left third molar has been found to cause most infection The mandible right third molar is the most commonly tooth affected which is vulnerable to odontogenic infections while Marioni et al. [39] reported that lower first molar is the principal cause of infection. Shah, A. et al. attributed it to lower right first molar tooth. Wabik et al. study shows that lower third molar tooth is most often involved. In our study, we saw nine patients with lymphatic origin most of whom had multiple spaces infection, there are six cases, and three cases with single space. Lateral pharyngeal space is considered to be the most space involved in a patient with lymphatic origin.
Multiple spaces involvement was more in diabetic patients group than in non-diabetic patients but the result is not significant p=0.065. This result agrees with many previous studies but studies showed a statistically significant difference. Also in our study, the multiple spaces infection were more common than single space in both groups which is similar to results reported by Chang et al. Sub-mandibular space was the most often involved in both groups, followed by buccal space and masteric space ; this result is similar to previously reported. Another study reported that the common space was parapharyngeal space.
Streptococcus species organisms were the common bacteria isolated from facial spaces infection in both groups in this study, where is this result concerns with many previously reported studies.
But Juncar et al. [40] reported that Staphylococcus aureus was the most prevalent microorganism, followed by Streptococcus pyrogens Another study reported that a different isolated bacteria in a diabetic and non-diabetic patient. Those studies showed that the K. pneumonia was common in diabetic, followed by Streptococcus spp. and most common bacteria isolated in non-diabetic was Streptococcus spp, followed by Staphylococcus aureus.
Forty-six cultured samples exhibited no growth; this may be referred to the samples collection following giving the patient antibiotics and/or laboratory error through steppes of a technician of culturing such as sample handling, transporting, and processing. Jang et al. reported that white blood cells (WBCs) were significant between diabetic with HbA1c ≥7% and HbA1c <7%. In this study, the WBCs at admission were significant p=0.041 by use (T-test, ANOVA test & CHI-square test). The mean in a diabetic group is 11.69, and it is 10.01 in a non-diabetic group (where is this result conversely previous studies.
The hospitalization period in the diabetic group is longer than a non-diabetic group. This is mostly because the diabetic group had more complications; more spaces were involved and more time was required to control blood sugar. Though not statistically significant, this result agrees with the previous study and disagrees with other studies which reported significant association.
Jang et al. documented that uncontrolled patients residing in a hospital was more than controlled patients. The interval between the incidences resulted in infection and leading to hospitalization between two groups is significant p<0.05. This result agreed with Juncar et al.
Tracheotomy used in four cases from the diabetic group and three cases in the non-diabetic group was statistically not significant. While this result is similar to previous studies. Lin et al. and Huang et al. reported that tracheotomy was performed in a diabetic group more often than a non-diabetic group with a statistical difference. Rao et al. said no patient underwent tracheotomy in their study.
In our study, we have 72% of patients with complications; diabetic groups complication was more than non-diabetic; but not statistically significant. These complications were related to disturbance of immune system inclusive neutrophils function, cellular immunity, and complement function. Also, in aged patients with reduced neutrophil adhesion is described by a reduction in Fcgamma receptor-mediated neutrophil effector. Increasing of glucose level led to compromised of phagocytic function. Whereas this result agrees with previous studies another study reported that this relation it was significant between two groups. Jang et al. reported statistically significance between controlling patient and nu monitoring patient. The major complication in our study was Mediastinitis which occurred in four patients, one from diabetic group, and three from non-diabetic group. Also, one case of Ludwig angina occurred in diabetic group accounting for 4.1%. Odontogenic or lymphatic infection may spread down to retropharyngeal space leading to acute mediastinitis also cervical necrotizing fasciitis may result in polymicrobial infection with a prevalence of Streptococcus species and anaerobic Bacteroides in synergistic coexistence [41]. The seriousness of infection depends on the number, type of spaces implicated and also the general condition of a patient. Trismus constituted the biggest complication in both groups accounting for 73.3%. Another study showed that Trismus was the biggest clinical sign in odontogenic infection.
According to the nature of the complication and multiple areas of facial spaces infection involved in diabetic patients makes them less suitable to conventional treatment. Therefore, a diabetic group with multiple spaces infection of the oral maxillofacial region should get more attention, good diagnosis and more aggressive treatment than the other groups. Controlling of blood sugar at a normal level is essential for treating maxillofacial spaces infection to activate or stimulate the immune response; some patients may need to consult with a specialist.
It has been documented that diabetic patients were affected with more pyretic than non-diabetic patients [25,27] whereas our study showed that patient presented to us very late had no Pyrexia because they were given prescribed medical treatment. This result is similar to Das R, G Nath, and A Mishra.
In comparison with non-diabetic group in our study, a diabetic patient underwent surgery more than non-diabetic, with the difference being statically significant p<0.017, whereas this result reported in studies previously. For a patient with extended space infection, surgical treatment remains an appropriate treatment. Abscess formation with facial spaces infection, especially in diabetic patients, must be opened as soon as possible. An extra oral surgical approach in diabetic patients occurred in 63.8% more than non-diabetic patients (49.3%) which was significant statistically p<.046.
From the under 12 year group, we had ten cases, two children with diabetic Mellitus type 1, and eight non-diabetic children. Caries was considered the biggest source of children patients. Buccal space was the most common space involved in children patients. The first deciduous molar, and first permanent molar teeth were found as the most prevalent origin of infection. Six cases were undergoing surgery, and conventional treatment was in accorded to four cases
Ceftriaxone antibiotics were often used to treat facial spaces infection in this study. The third-generation of cephalosporin antibiotic contained Ceftriaxone which is considered as belonging to B-lactam family of antibiotics. This type of antibiotic characteristic, long half-life, a broad spectrum against gram-negative, gram-positive and some anaerobic bacteria. It is also used to treat bacteria that tend to be resistant to many other antibiotics. Ceftriaxoneact inhibits bacterial cell wall synthesis by binding to transpeptidase these catalyze the cross-linking of the peptidoglycan polymers to form bacteria cell wall. Shah et al. showed that the ceftriaxone could be used in odontogenic infection, which had 82.4% efficacy against all organisms (gram-negative, gram-positive). Metronidazole or ornidazole are highly active against anaerobic organisms, but a single use in facial infection makes it poorly effective [42]. So, in our study we used it within combination with ceftriaxone.
Conclusion
In conclusion, this study highlights diabetes mellitus as a leading risk factor for facial space infection, despite the availability of effective antibiotics and inspite of developing diagnostic tools. In our study, the diabetic patient underwent extended hospitalization. The more multiple spaces infections, the more complication and seriously in older patients. Neglecting to treat a toothache at the first incidence of infection leads to complication. This clearly emphasizes the importance of proper oral hygiene and regular check-ups for dental infections. The diabetic patient is more exposed to complication and so, doctors should give more attention to treat these cases. Four points are significant for treatment, namely, control the airway, use efficiently antibiotic, surgical drainage and involved tooth treatment as soon as possible. This study added empirical data to support clinical imitation and to afford serve as a database for future prospective study.
Funding
None.
REFERENCES
- Shah A, Ramola V, Nautiyal V. Aerobic microbiology and culture sensitivity of head and neck space infection of odontogenic origin. Natl J Maxillofac Surg 2016;7:56.
- Bakir S, Tanriverdi MH, Gun R, et al. Deep neck space infections: A retrospective review of 173 cases. Am J Otolaryngol 2012;33:56-63.
- Lee JK, Kim HD, Lim SC. Predisposing factors of complicated deep neck infection: An analysis of 158 cases. Yonsei Med J 2007;48:55-62.
- Huang TT, Liu TC, Chen PR, et al. Deep neck infection: Analysis of 185 cases. Head & neck. 2004;26:854-860.
- Das R, Nath G, Mishra A. Clinico-pathological profile of deep neck space infection: A prospective study. Indian J Otolaryngol Head Neck Surgn 2017:1-9.
- Wang LF, Kuo WR, Tsai SM, et al. Characterizations of life-threatening deep cervical space infections: A review of one hundred ninety-six cases. Am J Otolaryngol 2003;24:111-117.
- Chen MK, Wen YS, Chang CC, et al. Deep neck infections in diabetic patients. Am J Otolaryngol 2000;21:169-173.
- Chi TH, Tsao YH, Yuan CH. Influences of patient age on deep neck infection clinical etiology and treatment outcome. Otolaryngology--Head and Neck Surgery 2014;151:586-590.
- Malik NA. Textbook of Oral and Maxillofacial Surgery: JP Medical Ltd; 2012.
- Gujrathi AB, Ambulgekar V, Kathait P. Deep neck space infection–A retrospective study of 270 cases at tertiary care center. WJOHNS 2016.
- Zamiri B, Hashemi SB, Hashemi SH, et al. Prevalence of odontogenic deep head and neck spaces infection and its correlation with length of hospital stay. J Dent (Shiraz) 2012;13:29-35.
- Farmahan S, Tuopar D, Ameerally PJ. A study to investigate changes in the microbiology and antibiotic sensitivity of head and neck space infections. The Surgeon 2015;13:316-320.
- Kinzer S, Pfeiffer J, Becker S, et al. Severe deep neck space infections and mediastinitis of odontogenic origin: Clinical relevance and implications for diagnosis and treatment. Acta Otolaryngol 2009;129:62-70.
- Eftekharian A, Roozbahany NA, Vaezeafshar R, et al. Deep neck infections: A retrospective review of 112 cases. Eur Arch Otorhinolaryngol 2009;266:273-277.
- Wabik A, Hendrich BK, Nienartowicz J, et al. Odontogenic inflammatory processes of head and neck in computed tomography examinations. Pol J Radiol 2014;79:431.
- Jansisyanont P, Kasemsai W, Bamroong P. Factors related to the treatment outcome of maxillofacial fascia space infection. J Oral Maxillofac Surg Med Pathol 2015;27:458-464.
- Schuknecht B, Stergiou G, Graetz K. Masticator space abscess derived from odontogenic infection: Imaging manifestation and pathways of extension depicted by CT and MR in 30 patients. European radiology 2008;18:1972-1979.
- Vieira F, Allen SM, Stocks RMS, et al. Deep neck infection. Otolaryngologic clinics of North America 2008;41:459-483.
- Huang SM, Wu RC. Rare type of deep neck infection: Two cases of descending necrotizing mediastinitis. Tzu Chi Medical Journal 2009;21:348-351.
- Suehara AB, Gonçalves AJ, Alcadipani FAMC, et al. Deep neck infection-analysis of 80 cases. Braz J Otorhinolaryngol 2008;74:253-259.
- Jang JW, Kim CH, Kim MY. Analysis of glycosylated hemoglobin (HbA1c) level on maxillofacial fascial space infection in diabetic patients. J Korean Assoc Oral Maxillofac Surg 2015;41:251-258.
- Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: A review of pathogenesis. Indian J Endocrinol Metab 2012;16:27.
- Chang JS, Yoo KH, Yoon SH, et al. Odontogenic infection involving the secondary fascial space in diabetic and non-diabetic patients: A clinical comparative study. J Korean Assoc Oral Maxillofac Surg 2013;39:175-181.
- Harrison GA, Schultz T, Schaberg S. Deep neck infection complicated by diabetes mellitus: Report of a case. Oral Surgery, Oral Medicine, Oral Pathology 1983;55:133-137.
- Rao DD, Desai A, Kulkarni R, et al. Comparison of maxillofacial space infection in diabetic and nondiabetic patients. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2010;110:e7-e12.
- Zheng L, Yang C, Kim E, et al. The clinical features of severe multi-space infections of the head and neck in patients with diabetes mellitus compared to non-diabetic patients. Br J Oral Maxillofac Surg 2012;50:757-761.
- Kamat RD, Dhupar V, Akkara F, et al. A comparative analysis of odontogenic maxillofacial infections in diabetic and nondiabetic patients: An institutional study. J Korean Assoc Oral Maxillofac Surg 2015;41:176-180.
- Bertoni AG, Saydah S, Brancati FL. Diabetes and the risk of infection-related mortality in the US. Diabetes Care 2001;24:1044-1049.
- Huang TT, Tseng FY, Liu TC,et al. Deep neck infection in diabetic patients: comparison of clinical picture and outcomes with nondiabetic patients. Otolaryngol Head Neck Surg 2005;132:943-947.
- Zheng L, Yang C, Zhang W, et al. Is there association between severe multispace infections of the oral maxillofacial region and diabetes mellitus? J Oral Maxillofac Surg 2012;70:1565-1572.
- Hidaka H, Yamaguchi T, Hasegawa J, et al. Clinical and bacteriological influence of diabetes mellitus on deep neck infection: Systematic review and metaâ€Âanalysis. Head & neck 2015;37:1536-1546.
- Lin H, Tsai CS, Chen Y, et al. Influence of diabetes mellitus on deep neck infection. JLO 2006;120:650-654.
- Pae M, Meydani SN, Wu D. The role of nutrition in enhancing immunity in aging. Aging and disease 2012;3:91.
- Favaretto N, Fasanaro E, Staffieri A, et al. Deep neck infections originating from the major salivary glands. Am J Otolaryngol 2015;36:559-564.
- Hong YW, Petersen PE, Ji YB, et al. The second national survey of oral health status of children and adults in China. Int Dent J 2002;52:283-290.
- Zhang S, Lo ECM, Liu J, et al. A review of the dental caries status of ethnic minority children in China. J Immigr Minor Health 2015;17:285-297.
- Marioni G, Rinaldi R, Staffieri C, et al. Deep neck infection with dental origin: Analysis of 85 consecutive cases (2000–2006). Acta Otolaryngol 2008;128:201-216.
- Parhiscar A, Har-El G. Deep neck abscess: A retrospective review of 210 cases. Ann Otol Rhinol Laryngol 2001;110:1051-1054.
- Storoe W, Haug RH, Lillich TT. The changing face of odontogenic infections. J Oral Maxillofac Surg 2001;59:739-748.
- Juncar M, Popa AR, BaciuÅ£ MF, et al. Evolution assessment of head and neck infections in diabetic patients–A case control study. J Craniomaxillofac Surg 2014;42:498-502.
- Leyva P, Herrero M, Eslava J, et al. Cervical necrotizing fasciitis and diabetic ketoacidosis: Literature review and case report. Int J Oral Maxillofac Surg 2013;42:1592-1595.
- Boscolo-Rizzo P, Stellin M, Muzzi E, et al. Deep neck infections: a study of 365 cases highlighting recommendations for management and treatment. Eur Arch Otorhinolaryngol 2012;269:1241-1249.