Anatomical variants of the hepatic artery: An Australian perspective
Received: 16-Nov-2019 Accepted Date: Mar 06, 2020; Published: 13-Mar-2020, DOI: 10.37532/1308-4038.20.13.89
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Aims and Objective: This cadaver-based study aimed to identify variants of the hepatic artery within the Australian population. Currently, original research toward the Australian population is limited.
Methods: Two hundred cadavers were donated over five years to The University of Melbourne. Each cadaver was dissected by experienced anatomists. A range of variants were described, and the rates in this study were compared to the rates observed in global literature.
Results: One hundred and eighty one (90.5%) specimens demonstrated normal anatomy (typically 55-81%). Of those with variant anatomy 9 (4.5%) had accessory arteries (typically 5.4- 20%), 5 (2.5%) had an aberrant right hepatic artery (typically 3.7- 11%), and 6 (3%) had an early branching of the common hepatic artery which is not typically independently reported.
Conclusion: This study demonstrated that Australian cadavers have a unique distribution of hepatic artery variants. This further emphasizes the dissimilarity of the rates of anatomical variation found globally and in turn the benefit of international exposure
Keywords
Hepatic artery; Anatomical variation; Australia, General surgery; Transplant surgery; Pancreatic surger
Abbreviations
CHA: Common Hepatic Artery; LHA: Left Hepatic Artery; RHA: Right Hepatic Artery; SMA: Superior Mesenteric Artery; LGA: Left Gastric Artery
Introduction
The hepatic artery is a structure of great significance in surgical pathology. A clear delineation of its course is paramount prior to its manipulation. Thus, intimate knowledge of both its typical course and common variants is imperative. Variants of the hepatic artery have been described extensively in both radiology and general surgery. In the global literature, variations of the hepatic artery have a reported incidence of 20-50% [1]. If encountered intraoperatively without prior identification and knowledge, they may predispose to significant complications, morbidity and mortality.
Variations have been studied across a wide variety of cohorts, with the rates of the most common variants becoming well established [2]. Despite this, the ethnic diversity intrinsic to the Australian population denotes that often Australian prevalence does not correlate with that found internationally. Hence, a study within an Australian cohort is needed for further refinement.
Normal anatomy
The liver is unique in that it receives blood from two sources, the majority being received venously (70-80%) [3]. Venous blood from the intestinal tract is carried to the liver for detoxification by the portal vein, whereas oxygenated blood is carried to the liver by the hepatic artery [4].
At the level of the twelfth thoracic vertebrae, the coeliac trunk emerges from the aorta and divides in to the splenic, left gastric and common hepatic arteries. After a variable length, the common hepatic artery gives off the gastroduodenal artery, at which point the continuing common hepatic artery is now referred to as the hepatic artery proper. The hepatic artery proper then bifurcates into the left and right hepatic arteries supplying the left and right lobes of the liver respectively. The cystic artery supplies the gall bladder and the biliary tree post branching off the right hepatic artery; as such variations of the right hepatic artery have additional surgical implications for the biliary tree (Table 1).
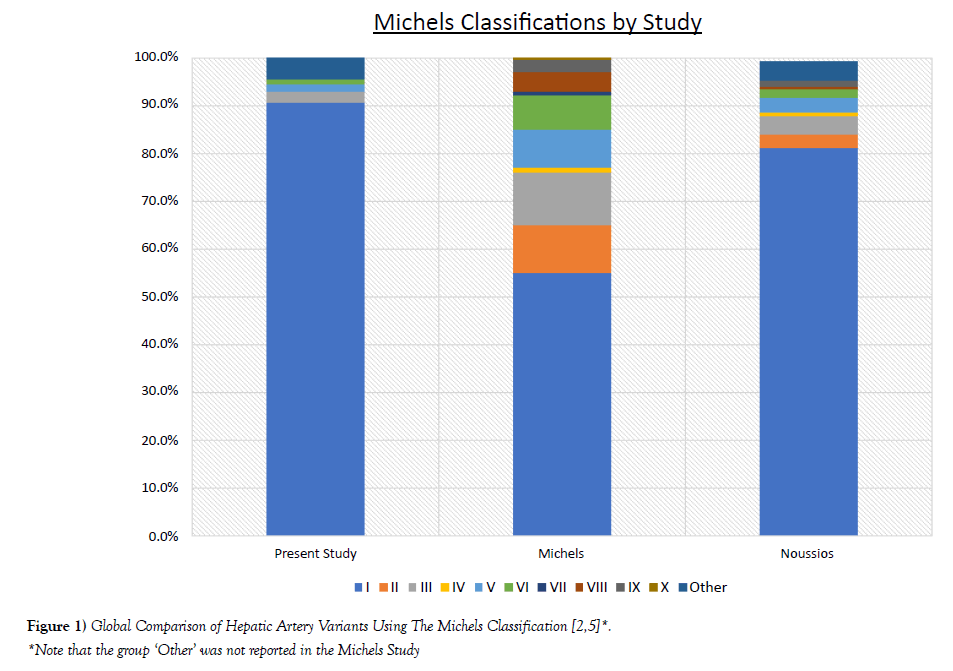
TABLE 1 Global comparison of hepatic artery variants using the Michels Classification [2,5].
| Michels Type | Description | Present Study | Michels (n=200) | Noussios (n=19,013) |
|---|---|---|---|---|
| I | Normal | 181 (90.5%) | 55% | 81% |
| II | Replaced LHA | 0 (0.0%) | 10% | 3% |
| III | Replaced RHA | 5 (2.5%) | 11% | 3.7% |
| IV | Replaced LHA and RHA | 0 (0.0%) | 1% | 0.8% |
| V | Accessory LHA | 3 (1.5%) | 8% | 3.2% |
| VI | Accessory RHA | 2 (1.0%) | 7% | 1.6% |
| VII | Accessory LHA and RHA | 0 (0.0%) | 1% | 0.2% |
| VIII | Accessory and Replaced | 0 (0.0%) | 4% | 0.4% |
| IX | CHA from SMA | 0 | 2.5% | 1.2% |
| X | CHA from LGA | 0 | 0.5% | 0.0% |
| Other | 10 (5.0%) | Not Reported | 4.1% |
Abbreviations: LHA: Left Hepatic Artery; RHA: Right Hepatic Artery; CHA: Common Hepatic Artery; SMA: Superior Mesenteric Artery; LGA: Left Gastric Artery
Academically, a lymph node may arise within this triangle and may act as an added structure to help identify this triangle (eponymously known as Lund’s or Mascagni’s Lymph node). It is commonly enlarged with cholecystitis and diseases of the biliary tree [4]. Furthermore, and outside the scope of this review, the cystic artery was the original superior boundary of this triangle as classically described by Calot, rather than the liver margin. Hence the descriptor of the triangle as “cystohepatic” is regarded a misnomer [5]. It has been suggested to rename this structure the “hepatobiliary” triangle after observed variations in this region were better described when bordered by the liver edge rather than the cystic artery [6].
Embryology
It is prudent to discuss the underlying embryology of the liver’s vasculature and thus how these variants typically arise [4].
From early gestational life, the arterial supply to the liver is from three main sources:
• The foetal left hepatic artery from the left gastric artery
• The middle hepatic artery or the common hepatic artery from the coeliac trunk
• The foetal right hepatic artery from the superior mesenteric artery
As the blood supply assumes the adult pattern, the foetal right and left hepatic arteries atrophy and the common hepatic artery supplies the whole liver by branching in to the adult right and left hepatic arteries (Figure 1).
The right and left foetal arteries may remain, with the absence or continuation of hepatic artery branching, hence the emergence of the variants described.
Variants
A wide range of variants can occur at each point along this arterial tree, as described by McMinn et al.:
• Rather than from the coeliac trunk, the common hepatic artery may emerge from the superior mesenteric artery or directly off the aorta [4].
• The right hepatic artery may arise from the superior mesenteric artery.
• The left hepatic artery may arise from the left gastric artery
Regarding the aforementioned foetal left and right hepatic artery, they may exist in addition to the normal anatomy and are thus described as “accessory” or completely replace the normal branches and be described as “aberrant”. Of course, in addition to this, many wild variations exist, though they are rare. One such rare variant is the early branching of the common hepatic artery.
Classification
Many classification systems have emerged over time. Michels is commonly seen as the first author to described variant hepatic anatomy, though some denote this honour to Adachi who in 1926 discussed variations of the coeliac axis with some attention given to hepatic artery variants [6]. Michels described ten different variations in his series of 200 cadavers [5]. Hiatt furthered this in 1994 by simplifying this list to six groups [7]. This was then reduced further into three groups by Abdulluh in 2006 [8]. However, as these variants are very diverse there are still some rare hepatic variations which defy classification. Hence these classification systems, though versatile, are not all encompassing. The Michels classification is described below and is the most common throughout literature.
Michels Classification: Proposed by Michels et al. in 1956 [5].
• I: Typical anatomy
• II: Replaced Left Hepatic Artery from Left Gastric Artery
• III: Replaced Right Hepatic Artery from Superior Mesenteric Artery
• IV: Replaced Right Hepatic Artery and Left Hepatic Artery
• V: Accessory Left Hepatic Artery (usually from the Left Gastric Artery)
• VI: Accessory Right Hepatic Artery (usually from the Superior Mesenteric Artery)
• VII: Accessory Right Hepatic Artery and Left Hepatic Artery
• VIII: Replaced RHA and accessory LHA or vice versa
• IX: Common Hepatic Artery from Superior Mesenteric Artery
• X: Common Hepatic Artery from Left Gastric Artery
Methods
This was a cadaver-based study conducted over five years from 2007 to 2012, with forty cadavers donated each year to the University of Melbourne for the teaching of surgical anatomy. Thus, a total of 200 cadavers were examined. Ethics approval was given by The University of Melbourne Ethics Committee and this study is consistent with the declaration of Helsinki [9].
Dissection was performed by experienced anatomists with direct and meticulous examination of anatomical variants. The dissection of the hepatobiliary tree in each specimen was performed by subspecialist anatomists with a particular interest in abdominal anatomy.
A description of the anatomical variants for each system within each specimen was compiled. Specimens with variants in the hepatic artery were selected and de-identified; findings were then described in detail, particularly:
1. The presence of accessory arteries
2. The presence of aberrant right hepatic artery anatomy as classified by Michels et al.
3. The presence of a common hepatic artery that was considered to branch early
The data was then collated as a percentage and discussed in comparison to the rates observed in the global literature. ‘Normal’ anatomy was considered a common hepatic artery originating from the celiac trunk and diverging into the left hepatic artery and right hepatic artery at an adequate length with no accessory vessels.
Selection for global rates
After a comprehensive literature review, two studies were selected that described the Michels classification. The first study was the original study performed by Michels et al. on his dissection of 200 cadaver specimens [5]. The second study was a meta-analysis provided by Noussious in which the cohort was substantially larger synthesizing data from the collation of over 19,000 specimens [2]. A number of articles were used which classified hepatic artery variants using the Michel’s classification in cadaver, both radiological and surgical studies.
Results
Of the 200 cadavers examined, 76 specimens demonstrated variations of the Hepatobiliary architecture. Nineteen of these involved the hepatic artery, with the remaining variants relating to venous, biliary or viscous anatomy.
Accessory arteries occurred in eight (4%) of the specimens, specifically:
• Three of these accessory arteries were left hepatic arteries arising from the left gastric artery corresponding to a rate of 1.5%, this is a Michels type V occurring with a rate of 3.2-8% in the literature.
• Two of these accessory right hepatic arteries arose from the superior mesenteric artery corresponding to a rate of 1.0%, this is a Michels type VI occurring with a rate of 1.6-7% in the literature.
• Two of the accessories came off the common hepatic artery and were deemed a “middle hepatic artery” and have thus been classified as ‘Other’
• An accessory common hepatic artery was also observed
Five of the specimens in the study had a right hepatic artery originating away from the common hepatic trunk (2.5%).
• These five specimens displayed a single replaced right hepatic artery on to the superior mesenteric artery corresponding to a Michels Type III with a rate of 3.7-11% quoted in the literature.
• There were no examples of an aberrant left hepatic artery within our cohort, corresponding to a Michels type II which occurs with a rate of 3-10% in the literature.
Further, six specimens were described to have early bifurcation of the common hepatic artery into left and right branches corresponding to a rate of 3.0%.
Discussion
The variant anatomy of the hepatic artery is widely discussed in the literature in relation to its surgical significance [2]. The two related major surgeries are liver transplantation and the Whipple’s procedure (pancreaticoduodenectomy) for head of pancreas tumours [10,11].
In hepatic transplantation, a detailed knowledge of the hepatic artery and its variants has facilitated the development of advanced techniques such as living-donor transplantation and reduced liver or “split liver” transplant. In the split liver technique described by Pilchlmayer et al., the right and left lobes of one organ can be used to benefit two separate recipients or facilitate live donation [12]. As such, adequate knowledge of the entire hepatic vascular system is of utmost importance [13].
Furthermore, intimate knowledge of the hepatic artery is needed for the administration of non-curative intra-arterial therapies in hepatocellular carcinoma such as trans-arterial chemoembolization and for therapeutic ligations of the hepatic artery as used in operations for hepatic neoplasms, trauma and liver arterial lesions [14]. Due to collateral portal circulation a normal liver can withstand ligation of the hepatic artery. These procedures are contraindicated in patients with limited hepatopedal flow such as liver transplant patients, as graft harvesting interrupts all routes of collateral circulation rendering the transplant devastatingly susceptible to ischaemic injury, as well as those with complete portal vein thrombosis or macrovascular invasion in to the portal vein.
A replaced right hepatic artery is the most commonly described variant in the literature and our study was consistent with this. Aberrant arteries in general are broadly considered to “increase the complexity of surgery” [14]. The primary surgical risk is accidental ligation of aberrant arteries leading to end organ ischemia.
Knowledge of aberrant right hepatic artery anatomy is most integral to the surgical procedure of pancreaticoduodenectomy (Whipple’s procedure) in the treatment of head of pancreas cancer [15]. The gastroduodenal artery is routinely sacrificed during the Whipple’s procedure and the bile duct therefore becomes entirely dependent on the integrity of the right hepatic artery for its blood supply. An aberrant right hepatic artery, if present, tends to be the origin of the cystic artery, this leads to increased need for manipulation and further risk of biliary complications [15]. An aberrant right hepatic artery originating from the superior mesenteric artery will have a close relationship to the head of the pancreas making the vessel even more susceptible to complications in this variant. With this, attempts to preserve the right hepatic artery would then result in compromised resection of the head of pancreas. Due to the high significance of this variation to the Whipple’s procedure it has been well examined and has its own subclassification [15]:
• Type 1: Artery lies posterolateral to the head of pancreas.
• Type 2: Artery runs intra-parenchymal.
• Type 3: Artery lies in the superior mesenteric groove.
A further complication of this variant is that the right artery arising from the superior mesenteric artery usually runs behind the portal vein, therefore requiring a more technical approach.
This study and most of the literature describes variations primarily surrounding the right and left hepatic arteries, with limited data on variations to the common hepatic artery. In our series we were able to demonstrate the prevalence of variants in the branching of the common hepatic artery, particularly early branching. We are however limited in the fact that discreet measurements were not recorded and instead this was based on the dissector’s acumen and experience. However, this is consistent with a recent Indian study that demonstrated this variant radiologically [10]. The shorter course may prove challenging in the difficult anastomoses of transplants. Indeed, increased arterial tension has been shown to cause turbulent blood flow and in turn promote hepatic artery thrombosis, one of the major complications of liver transplantation [16]. Other consequences of a short common hepatic artery include graft failure, anastomotic breakdown, hepatic artery stenosis and pseudoaneurysm [16].
Studies regarding variants of the hepatic artery are largely from a radiological perspective with CT angiography identifying variations pre-operatively. Indeed, in Noussios et al. only 8 of the 21 studies reported where based on variants found by examining cadavers and of these one was a case report and one included live patients as well [2]. Having a cadaverous cohort rather than one preselected by the presence of disease is more reflective of the general population. Conversely, for this same reason this approach may not be as effective at reporting variants that Australian surgeons will commonly encounter. This is of course assuming that anatomical variants increase the risk of requiring surgery and thus are over represented in said cohort, this is likely not the case.
Additionally, selection bias may have played a role in the lower prevalence of variants observed in this study as cadavers must pass through selection criteria before being provided for educational purposes, though again it is unclear how this would directly affect the representation of anatomical variants. Regardless, even when focusing on the atypical variants themselves, rather than their frequency in relation to normal anatomy, we can see a dissimilate trend in our population compared to international studies.
Conclusion
There was far less variation observed in this cohort compared to that which has been observed in international studies. This emphasis the benefit of overseas fellowships, in that they provide exposure to conditions, procedures and variants not common to Australia. However, the fact that there were multiple additional variants of the Hepatic Artery outside of the Michels classification in our cohort denotes that there is a wide variety of possible variants. It would be impractical to expect to be exposed to every possible variant. The ultimate focus is for pre-operative planning and safe surgical technique.
REFERENCES
- Fonseca-Neto OCLd, Lima HCdS, Rabelo P, et al. Anatomic Variations of the Hepatic Artery: A study in 479 Liver Transplantations. Arq Bras Cir Dig. 2017;30:35-7.
- Noussios G, Dimitriou I, Chatzis I, et al. The Main Anatomic Variations of the Hepatic Artery and Their Importance in Surgical Practice: Review of the Literature. J Clin Med Res. 2017;9:248-52.
- Kan Z, Madoff DC. Liver anatomy: microcirculation of the liver. Semin Intervent Rad. 2008;25:77.
- McMinn RMH. Last’s Anatomy: Regional and Applied (9th ed). United Kingdom, Churchill Livingstone. 1994; 348-50.
- Michels NA. The hepatic, cystic and retroduodenal arteries and their relations to the biliary ducts: with samples of the entire celiacal blood supply. Ann Surg. 1951;133:503-24.
- Yamamoto M, Zaima M, Yamamoto H, et al. Liver necrosis shortly after pancreaticoduodenectomy with resection of the replaced left hepatic artery. World J Surg Onc. 2017;15:77.
- Hiatt J, Gabbay J, Busuttil R. Surgical Anatomy of the Hepatic Arteries in 1000 Cases. Ann Surg. 1994;220:50-52.
- Abdullah S, Mabrut J, Garbit V, et al. Anatomical variations of the hepatic artery: study of 932 cases in liver transplantation. Surg Radiol Anat. 2006;28:468-73.
- World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191-4.
- Pallavi, Sripathi S, Ravichandra V. A radiological evaluation of the length of the hepatic artery and its practical implications during liver transplantation. GJRA. 2015;4:9.
- Bhardwaj N. Anomalous Origins of Hepatic Artery and Its Significance for Hepatobiliary Surgery. J Anat Soc India. 2010;59:173-176.
- Hackl C, Schmidt K, Susal C, et al. Split liver transplantation: Current developments. World Journal of Gastroenterology. 2018;24:5312-21.
- Chaib E, Ribeiro M, Saad W, et al. The Main Hepatic Anatomic Variations for The Purpose of Split-Liver Transplantation. Hepatogastroenterology. 2004;78:355-6.
- Madhu Y, Harish K. Accessory Right Hepatic Artery and Its Implications for a Surgeon. Indian Journal of Surgery. 2013;75:492-4.
- Stauffer J, Bridges M, Turan N, et al. Aberrant right hepatic arterial anatomy and pancreaticoduodenectomy: recognition, prevalence and management. HPB. 2009;11:161-5.
- Ramanadham S, Toomay S, Yopp A, et al. Rare Hepatic Arterial Anatomic Variants in Patients Requiring Pancreatoduodenectomy and Review of the Literature. Case Rep Surg. 2012;2012:953195.