Anatomical variation in the course of the phrenic nerve
2 Department of Anatomy, Alpha medical s.r.o, Diagnostic Center of Pathology, Member of the Unilabs Group, Prešov, Slovak republic
Received: 29-Jan-2020 Accepted Date: Jun 29, 2020; Published: 06-Jul-2020
Citation: Hvizdosova N, Mateffy S, Kovacova Z, et al. Anatomical variation in the course of the phrenic nerve. Int J Anat Var. 2020;13(3):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Anatomical variations of the phrenic nerve are classified as variation in the origin, course, or as the presence of the accessory phrenic nerve. Origins or combinations of branches may differ from patient to patient. Some variations of phrenic nerve are very common and can cause complications in performing very simple and standard procedures. We have detected an anatomical variation of phrenic nerve in the right lateral cervical region during routine dissection. The localization of the right phrenic nerve was detected ventrally from the right subclavian vein. Variation was not found on the left side of the same cadaver. The relationship of the subclavian vein and the phrenic nerve and their variations should be familiar to anesthesiologists during subclavian vein cannulation and practice of suprascapular nerve block.
Keywords
Phrenic nerve; Subclavian artery; Subclavian vein; Diaphragm; Variation
Introduction
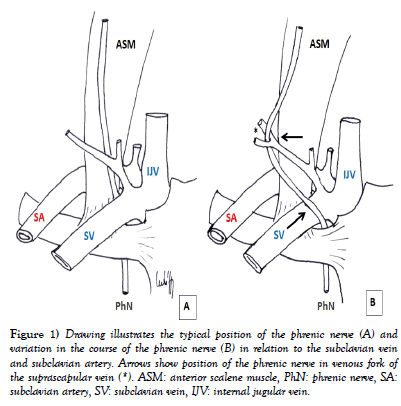
The phrenic nerve is a mixed motor/sensory nerve. According to established literature phrenic nerve arises in the cervical region mainly from the cervical plexus predominantly from the 4th segment, but also receives fibers from the 3rd and 5th cervical nerves (C3-C5) in humans [1]. However, recent studies pointed the segments C4 and C5 as the most common origin, with only 22% of the cases being from C3 [2]. In the lateral cervical region, the phrenic nerve descends vertically downwards, around the anterior scalene muscle within the prevertebral layer of cervical fascia, passes laterally to the ascending cervical artery to enter the superior thoracic aperture and continues to the diaphragm. It lies ventral to the vagus nerve in the inferior mediastinum [3]. In the subclavian triangle, the nerve is visible only in the lower part because it is covered by sternocleidomastoid muscle. Before entering the thoracic cavity, the phrenic nerve passes between the subclavian artery and the subclavian vein (Figure 1). The right phrenic nerve runs laterally and slightly posterior to the brachiocephalic vein and continues along the superior vena cava. On the left, the nerve continues to descend across the left lateral surface of the arch of aorta, passing superficially to the left vagus. Both nerves pass anterior to the hila of the lungs as they descend to the diaphragm between pericardial and pleural sacs [4]. The right phrenic nerve passes through the caval opening in the tendon of the diaphragm and leaves the thorax with inferior vena cava. The left phrenic nerve leaves the thorax by piercing the muscular part of the diaphragm near the apex of the heart [5]. The pericardiophrenic artery and vein accompany it through most of its course in the thorax [3].
Figure 1: Drawing illustrates the typical position of the phrenic nerve (A) and variation in the course of the phrenic nerve (B) in relation to the subclavian vein and subclavian artery. Arrows show position of the phrenic nerve in venous fork of the suprascapular vein (*). ASM: anterior scalene muscle, PhN: phrenic nerve, SA: subclavian artery, SV: subclavian vein, IJV: internal jugular vein.
It provides complete motor innervation of the diaphragm and sensation of the central tendon part of the diaphragm, also provides touch and pain sensory innervation of the mediastinal pleura, fibrous pericardium and parietal layer of serous pericardium [6,7], the parietal peritoneum below the diaphragm to the gallbladder and pancreas.
The topographical relationship between phrenic nerve and subclavian vessels is clinical important because phrenic nerve may be damaged during subclavian catheterization. In this report, we describe a variation of the phrenic nerve in relation to the subclavian vein and subclavian artery.
Case Report
This case involved the neck dissections of an approximately 70-year old female cadaver in the Department of Anatomy, Pavol Jozef Safarik University in Kosice, Slovakia. The dissection was carried out according to the instruction by Mráz (1995). The cadaver had been embalmed soon after death and preserved by the injection of formaline preservative solution. The dissection was performed in accordance with ethical standards.
During a routine anatomical dissection for educational purposes of general medicine students, we have dissected a unilateral variation of the phrenic nerve courses in the lateral cervical region on the right side of the neck.
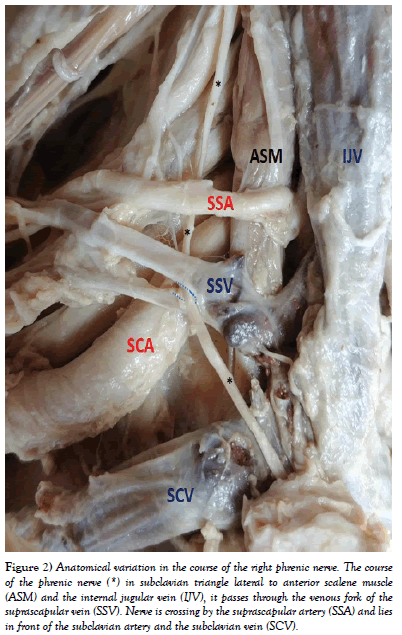
After the sternocleidomastoid muscle was lifted off and the inferior belly of omohyoid muscle identified, we cut the deep cervical fascia and separated the course of the muscle. After the removal of adipose tissue in the area of the subclavian triangle, we isolated the confluence of double suprascapular vein. Into its forked confluence immerged the right phrenic nerve (Figure 1), which has been thereby deflected laterally from its physiological course, outside the anterior scalene muscle. The nerve was in its course covered by the prevertebral layer of the cervical fascia up to the venous junction, from which the nerve descended caudally to the superior thoracic aperture, ventral to the right subclavian vein (Figure 2). With this lateral course, the nerve directly adhered to the dorsally located right subclavian artery. Except for the variation in the course in subclavian triangle, we did not notice other anomalies of the right phrenic nerve. The nerve was formed according to the characteristic norm by the cervical plexus branches C3 and C4 and received the fibers from the brachial plexus C5. In the thoracic cavity, it passed by the characteristic course, and the right diaphragm dome, compared to the contralateral one, was in position and without trophic abnormalities. The left phrenic nerve ran throughout its range without variation.
Figure 2: Anatomical variation in the course of the right phrenic nerve. The course of the phrenic nerve (*) in subclavian triangle lateral to anterior scalene muscle (ASM) and the internal jugular vein (IJV), it passes through the venous fork of the suprascapular vein (SSV). Nerve is crossing by the suprascapular artery (SSA) and lies in front of the subclavian artery and the subclavian vein (SCV).
Discussion
The phrenic nerve represents an important nerve that provides motor innervation of the diaphragm as the main inspiratory muscle. Knowing its exact course, which can demonstrate individual variation, is important in optimizing surgical approaches and applying anesthetics within the performance of a regional block.
The present case report describes the finding of variable course of the right phrenic nerve, which normally passes into the thoracic cavity, posterior to the subclavian vein. In our finding, the phrenic nerve was located ventral to the right subclavian vein. However, this variation was not found on the opposite side of the same cadaver. The presence of nerve ventral to subclavian vein may be the cause of its damage during insertion of the central venous catheter. Cannulation of the venous system is performed by a puncture through the venous access according to the guiding anatomical structures; therefore, in patients at risk, it is appropriate to perform it under ultrasound guidance due to anatomical variations [8-11]. The same unilateral finding on the right side of the neck was also found by Prakash Prabhu et al. (2007) at the anatomy dissection of a 30-year old man. Banneheka (2008) reported the incidence of this variation in 2.9% of the 206 cases. Paraskevas et al. (2011) focused on the topography of the phrenic nerve and subclavian vein, and from of 84 cases in only 2 cases the phrenic nerve was located in front of the subclavian vein and in one case passed through the wall of the subclavian vein. The incidence of variable nerve localization varies between 7.25% [12] to 9% [6]. Anomalies in nerve location can cause a wide range of clinical symptoms. The pulsation of the adjacent subclavian artery, or point pressure at the venous junction (confluence) site, may lead to chronic stimulation of the phrenic nerve.
The presence of the phrenic nerve in front of the subclavian vein leaves the nerve in a vulnerable position during puncture or cannulation of the subclavian vein, which may cause hemi diaphragmatic paralysis. This variation may be asymptomatic during a surgical intervention to the neck or in the interscalene and supraclavicular phrenic nerve block it cannot be overlooked, and an extra care must be taken [13].
Conclusion
Likewise, the compression syndrome caused by the localization of the nerve in the venous fork is a possible cause of various neurological manifestations with primary unclear etiology. The finding demonstrates the need for a thorough knowledge of the anatomical variations of the phrenic nerve, which will enable safe and effective surgery using regional anesthesia and identify any complications in time.
The knowing the relation of the phrenic nerve and subclavian vein is very important for surgeons because nerve damage during venous cannulation could cause complications, such as diaphragmatic dysfunction, unilateral or bilateral diaphragmatic paralysis, manifested by decreased vital capacity, hypoxia, and rarely by shoulder pain.
REFERENCES
- Gray H, Standring S, Ellis H, et al. Head and neck. In: Gray H, eds. Gray's anatomy: the anatomical basis of clinical practice. 39th Ed., Edinburg, Elsevier/Churchill Livingstone. 2005;1627.
- Prates Júnior AG, Vasques LC, Bordoni LS. Anatomical variations of the phrenic nerve: an actualized review. J Morphol Sci. 2015;32:55-6.
- Drake LR. Head and neck. In: Drake LR, eds. Gray´s Anatomy for students. 3rd Ed., Philadelphia, Elsevier/Churchill Livingstone. 2015;1033-4.
- Kluchova D. Topographical anatomy of neck. In: Kluchová D, eds. Anatomy of head and neck. Kosice, Equilibria. 2018;134-5.
- Kugelmann D, Waschke J. Chest viscera. In: Waschke J, eds. Sobotta Anatomy Textbook. Munich, Elsevier. 2019;297-8.
- Standring S. Head and neck. In: Standring S, eds. Gray's anatomy: the anatomical basis of clinical practice. 40th Ed., Edinburgh, Elsevier/Churchill Livingstone. 2008;1551.
- Mráz P. Pitevne cvicenia. Martin, Osveta. 1995;199.
- Firment J, Studená A. Anesthesiology and Intensive Care. In: Firment J, eds. Anesthesiology and Intensive Care. Košice, UPJS. 2009;388.
- Prakash Prabhu LV, Madhyastha S, Singh G. A variation of the phrenic nerve: case report and review. Singap Med J. 2007;48:1156-7.
- Banneheka S. Morphological study of the ansa cervicalis and the phrenic nerve. Anat Sci Int. 2008;83:31-44.
- Paraskevas GK, Raikos A, Chouliaras K, et al. Variable anatomical relationship of phrenic nerve and subclavian vein: clinical implication for subclavian vein catheterization. Brit J Anaesth. 2011;106:348-51.
- Hollinshead WH. Anatomy for Surgeons. In: Hollinshead WH, eds. Anatomy for Surgeons. The Head and Neck, 3rd Ed., New York, Harper and Row. 1982:50.
- Rao TR, Kumar B, Shetty P, et al. Variation in the course of the left phrenic nerve: case report. Neuroanat. 2007;6:24-25.