Aortic aneurysms: A brief overview and dental implications
Received: 10-Oct-2018 Accepted Date: Nov 29, 2018; Published: 07-Dec-2018
Citation: Severs G, Day I, Joy A. Aortic aneurysms: A brief overview and dental implications. Int J Anat Var. Dec 2018;11(4):136-138.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
An aortic aneurysm is a dilatation of a segment of the aorta. Although it was previously believed that aneurysms were a form of atherosclerosis, aortic aneurysmal disease is now recognized as a distinct degenerative process involving all layers of the vessel wall. During routine dissection of the abdominal region of a 73-year-old female donor in the Gross Anatomy laboratory, first year dental students encountered an abdominal aortic aneurysm. The pathology was dissected in detail and documented with photographs. A literature review was carried out to study the condition and understand the clinical implications, with special emphasis on the implications of management in a dental setting.
Keywords
Aortic aneurysm; Anatomy; Dental management
Introduction
An aortic aneurysm is a dilatation of a segment of the aorta. Although it was previously believed that aneurysms were a form of atherosclerosis, aortic aneurysmal disease is now recognized as a distinct degenerative process involving all layers of the vessel wall. The pathophysiology of aortic aneurysms is characterized by four events: infiltration of the vessel wall by lymphocytes and macrophages; destruction of elastin and collagen in the tunica media and adventitia by proteases; loss of smooth muscle cells resulting in thinning of the tunica media; and neovascularization. Depending on their location, aortic aneurysms are classified as: aortic root aneurysm/aneurysm of Sinus of Valsalva; thoracic aortic aneurysm (may be ascending, aortic arch, or descending aneurysms); or abdominal aortic aneurysm (AAA).
Case Report
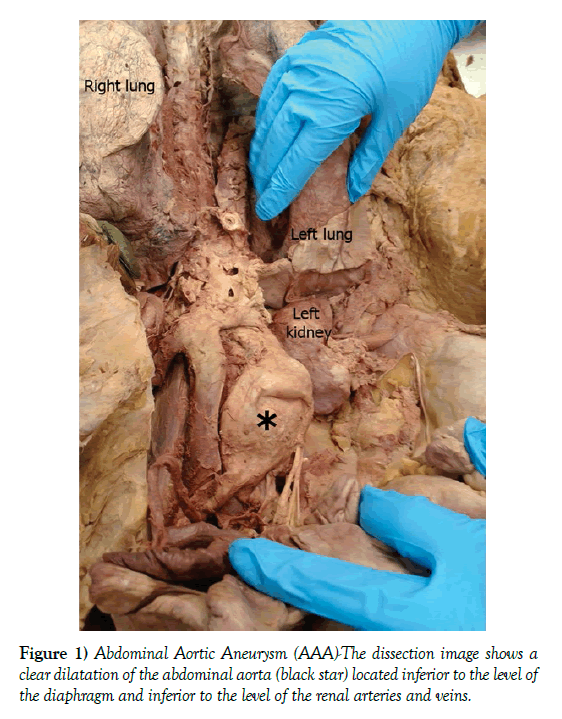
During routine dissection of the abdominal region of a 73-year-old female donor, the dissection team encountered an abdominal aortic aneurysm. The pathology was dissected in detail and documented with photographs. Measurements carried out indicated that the dilatation was approximately 11.43 cm wide and 26.8 cm long. The aneurysm was located inferior to the renal arteries and renal veins, and extended till about 4.5 cm above the bifurcation of the abdominal aorta into the right and left common iliac arteries. The branches of the inferior mesenteric artery could be seen extending inferiorly from the region of the dilatation (Figure 1). A literature review was carried out to study the condition and understand the clinical implications, with special emphasis on management of such patients in the dental setting.
Figure 1) Abdominal Aortic Aneurysm (AAA)-The dissection image shows a clear dilatation of the abdominal aorta (black star) located inferior to the level of the diaphragm and inferior to the level of the renal arteries and veins.
Discussion
The aorta, which originates in the left ventricle of the heart and travels inferiorly to eventually divide into the right and left common iliac arteries is one of the prominent arteries that can exhibit an aneurysm. Aortic aneurysms occur when there is a bulging of the aorta and is said to be present when the vessel measures greater than 3 cm [1]. In the current documented case, the dilatation observed was significantly larger than the minimum measurements that define an aortic aneurysm. Aortic aneurysms are slow-growing defects, typically developing over a number of years, and can remain unidentified due to the lack of symptoms associated with aneurysms. Aneurysms most often become symptomatic when they rupture, which leads to death in 90% of patients. Most intact aortic aneurysms do not produce symptoms, but as they enlarge, symptoms due to compression, such as abdominal and lumbar pain may develop. Compression of spinal nerve roots can also sometimes result in pain or paresthesia of the lower limbs [2-4].
Aortic aneurysms, whether abdominal or thoracic, generally occur due to a combination of weakening of the artery wall along with increased intravascular pressure. Abdominal aortic aneurysms (AAAs) are more common than thoracic aortic aneurysms (TAAs) because the abdominal aortic wall is thinner and less capable of resisting strain than the thoracic aortic wall. The two primary reasons for this are, the lower amount of elastin in the abdominal aorta than in the thoracic aorta, and the lack of the vasa vasorum in the abdominal aortic wall. Typically, most AAAs is true aneurysms that involve all three vessel wall layers (tunica intima, media, and adventitia). Multiple factors can increase the likelihood of developing an aortic aneurysm, including history of smoking, high blood pressure, atherosclerosis, and advancing age [1]. Abdominal aortic aneurysms (AAA) are more common after the age of 65 and are three to four times more prevalent in men than in women, most likely due to hormonal factors. Although AAAs are not nearly as prevalent in women as they are in men, women have four times the risk of rupture [3,4]. Behind smoking, genetic predisposition is the second most critical risk factor for aortic aneurysm development [1], with Caucasians being at higher risk for AAA formation [1]. Many different single nucleotide polymorphisms have also been correlated with a greater prevalence of AAA [1]. Certain genetic conditions have a much higher risk for thoracic aortic aneurysms (TAA) including Marfan syndrome, Loeys-Dietz syndrome, Ehlers-Danlos syndrome, and Turner syndrome [5]. Severe trauma and familial history have also been linked to higher incidence of aortic aneurysms.
Aneurysms can be discovered on abdominal examination; however, because of the retroperitoneal location of the aorta, palpation may not always be accurate. Ultrasonography is the primary method used for screening and is highly sensitive (95%) and specific (100%). The largest indicator for treatment and predictor of rupture is the size of the aneurysm [6-8]. The patient and/or physician may elect to only monitor the aneurysm if it is less than 5 cm in diameter [9-13]. Hypertension medications such as ACE inhibitors can be used to decrease the force placed on the vessel wall and reduce the risk of rupture in certain cases [14]. Open abdominal surgical intervention would consist of surgically opening up the patient’s chest or abdomen, depending on the location of the aneurysm, and replacing the part of the aorta containing the aneurysm with a synthetic graft to eliminate the weakened portion of the vessel [14]. Another surgical option is endovascular surgery. Endovascular surgery is less invasive than the open abdominal surgery, where the surgeons attach a graft to a catheter that is inserted into the femoral artery and maneuvered up the aorta until the aneurysm is found. Once the graft travels through the aorta to the aneurysm, the graft is then placed in the aneurysm to reinforce the weakened portion of the vessel to prevent further weakening or rupture [14].
After a patient is diagnosed with an aortic aneurysm it is recommended to avoid heavy lifting or any strenuous physical activity. Smoking cessation, elimination of stress, control of hypertension, and implementing a healthy diet have the potential to keep the aneurysm from further development [5,15-18].
Dental implications
A high prevalence of periodontal pathogens has been found in patients with abdominal aortic aneurysms and it is thought these bacteria could be involved with the formation and progression of aneurysms [19-23]. Many periodontal pathogens have been found in AAA dissections including Porphyromonas gingivalis, Aggregatibacter actinomycetemcomitans, Fusobacterium nucleatum, and Treponema denticola [19]. The current debate is whether these periodontal pathogens play a role in development of the aneurysm and weakening of the vessel, and/or if they are a secondary characteristic and colonize in the aneurysm after it has already developed. Newer studies have shown that repeated injections of P. gingivalis in rats have fostered aneurysm development, which was not found in rats injected with saline, showing that proper oral hygiene and routine dental care could reduce the risk of developing aortic aneurysms [20,24]. These aforementioned studies therefore suggest that it should be of high priority in the dental field to prevent and treat periodontal disease in high-risk AAA patients, especially white males with a smoking history. This is especially significant because of the association between periodontal pathogens and the risk of developing AAA in this subset of patients.
Clinical management in the dentist’s office
As a primary healthcare provider, dentists will encounter patients who have been diagnosed with AAAs. Decisions based on how to treat, when to treat, or if dental treatment can be provided are all complex and need to be addressed further based on size, symptoms, and progression of the disease. As a general rule, dental practitioners should approach these patients following the same guidelines as physicians and surgeons. A thorough medical history and physical examination should be performed, especially in those with a familial history of aortic aneurysms and dissection, due to the almost 20% increased incidence in these individuals. Patients with small to moderately sized aortic aneurysms (less than 4 cm in diameter) that is being monitored and which displays slow growth patterns pose only a small risk of rupture. The risk of rupture of an AAA is related to its diameter and shape – aneurysms larger than about 4 cm exhibit increased risk for rupture. With regard to shape, ‘saccular’ shaped aneurysms are at more risk for rupture than ‘fusiform’ aneurysms since the former result in excessive tension on the arterial wall as they are not dispersed along the length of the vessel. Patients who exceed the 4 cm size threshold therefore increase their risk of spontaneous rupture significantly, especially amongst smokers. Additionally, patients who have significant comorbidities like peripheral artery disease, rapid expansion of the aneurysm, and/or a coexistent aneurysm can all lead to a provider choosing to defer treatment until a physician or surgeon has been consulted and the aneurysm properly managed.
In patients with known AAAs, dental professionals should attempt to keep patient anxiety and stress at a minimum while continuously monitoring blood pressure. Nitrous oxide, supplemental oxygen, proper pain management, and local anesthesia can all aid in keeping AAA rupture at bay. Local anesthetic use is encouraged in AAA patients to prevent epinephrine spikes due to pain induction, but minimal vasoconstrictors are recommended to avoid increase in blood pressure [24]. In conclusion, patients with aortic aneurysms can be successfully treated in a dental setting with proper management and precautions while potentially reducing the progression of abdominal aortic aneurysms.
Conflict of Interest
The authors state that they have no conflicts of interest to declare.
REFERENCES
- Carino D, Sarac TP, Ziganshin BA, et al. Abdominal aortic aneurysm: Evolving controversies and uncertainties. Int J Angiol. 2018;27: 58-80.
- Assar AN, Zarins CK. Ruptured abdominal aortic aneurysm: a surgical emergency with many clinical presentations. Postgrad Med J. 2009; 85:268-73.
- Stather PW, Sidloff DA, Rhema IA, et al. A review of current reporting of abdominal aortic aneurysm mortality and prevalence in the literature. Eur J Vasc Endovasc Surg. 2014;47:240-2.
- Garcia SB. Abdominal aortic anuerysm. prevalence and associated risk factors in a population of patients hospitalized in Internal medicine. Revista clinica Espanola. 2018;30143-7.
- Bradley TJ, Alvarez NA, Horne SG. A practical guide to clinical management of thoracic aortic disease. Can J Cardiol. 2016;32:124-30.
- Chau KH, Elefteriades JA. Natural history of thoracic aortic aneurysms: Size matters, plus moving beyond size. Prog Cardiovasc Dis. 2013; 56:74-80.
- Laine MT, Laukontaus SJ, Kantonen I, et al. Population based study of ruptured abdominal aortic aneurysm. Br J Surg. 2016;103:1634-9.
- Laine MT, Vanttinen T, Kantonen I, et al. Rupture of abdominal aortic aneurysms in patients under screening age and elective repair threshold. Eur J Vasc Endovasc Surg. 2016;51:511-6.
- Geisbusch S, Griepp RB. Growth and rupture risk of small-to-moderate size ascending aortic aneurysms: A prospective study. J Thorac Cardiovasc Surg. 2016;151:278-9.
- Galland RB, Whiteley MS, Magee TR. The fate of patients undergoing surveillance of small abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 1998;16:104-9.
- Whiteley MS, Magee TR, Torrie EP, et al. Minimally invasive superficial femoral artery endarterectomy: Early experience with a modified technique. Eur J Vasc Endovasc Surg. 1998;16:254-8.
- Vardulaki KA, Prevost TC, Walker NM, et al. Growth rates and risk of rupture of abdominal aortic aneurysms. Br J Surg. 1998;85:1674-80.
- Wilmink AB, Quick CR. Epidemiology and potential for prevention of abdominal aortic aneurysm. Br J Surg. 1998;85:155-62.
- Chaikof EL, Dalman RL, Eskandari MK, et al. The society for vascular surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Surg. 2018;67:2-77.
- Peters AS, Hakimi M, Erhart P, et al. Current treatment strategies for ruptured abdominal aortic aneurysm. Langenbecks Arch Surg. 2016; 401:289-98.
- Schmitz Rixen T, Keese M, Hakimi M, et al. Ruptured abdominal aortic aneurysm-epidemiology, predisposing factors, and biology. Langenbecks Arch Surg. 2016; 401:275-88.
- Kokje VB, Hamming JF, Lindeman JH. Editor's choice-pharmaceutical management of small abdominal aortic aneurysms: A systematic review of the clinical evidence. Eur J Vasc Endovasc Surg. 2015;50:702-13.
- Sidloff D, Stather P, Dattani N, et al. Aneurysm global epidemiology study: public health measures can further reduce abdominal aortic aneurysm mortality. Circulation. 2014;129:747-53.
- Ding F, Lyu Y, Han X, et al. Detection of periodontal pathogens in the patients with aortic aneurysm. Chin Med J (Engl). 2014;127:4114-8.
- Delbosc S, Alsac JM, Journe C, et al. Porphyromonas gingivalis participates in pathogenesis of human abdominal aortic aneurysm by neutrophil activation-Proof of concept in rats. PLoS One. 2011;6:e18679.
- Kurihara N, Inoue Y, Iwai T, et al. Detection and localization of periodontopathic bacteria in abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2004;28:553-8.
- Paraskevas KI, Mikhailidis DP, Giannoukas AD. Periodontitis and abdominal aortic aneurysms: A random association or a pathogenetic link? Int Angiol. 2009;28:431-3.
- Pyysalo MJ, Pyysalo LM, Pessi T, et al. The connection between ruptured cerebral aneurysms and odontogenic bacteria. J Neurol Neurosurg Psychiatry. 2013;84:1214-8.
- Chaudhry S, Jaiswal R, Sachdeva S. Dental considerations in cardiovascular patients: A practical perspective. Indian Heart J. 2016;68:572-5.