Application Of Burow’s Wedge Advancement Flap For Reconstruction Of Facial Defects
Received: 12-Sep-2017 Accepted Date: Oct 04, 2017; Published: 06-Oct-2017
Citation: Dai HY, Wang YC, Lv C, et al. Application of Burow’s wedge advancement flap for reconstruction of facial defects. Surg Case Rep. 2017;1(1):5-7.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: To summarize our experience and principles of application of Burow’s wedge advancement skin flap (BWASF) in reconstruction of facial defects.
Methods: Defects in skin and tissue from a facial tumor and scar excision were repaired by BWASF. An aid incision was undertaken in concert with natural contour lines (nasolabial groove, sulcus alaris, maxillonasal suture, lid-margin, vermilion border, hairline) or skin wrinkles. The incision was concealed as much as possible.
Results: We reviewed 156 cases of use of BWASF (108 monolateral advancement flaps and 48 bilateral advancement flaps). Minimum and maximum areas of the facial defect (in cm) were 1.0 × 2.0 and 3.5 × 6.0, respectively. All flaps survived postoperatively without obvious complications. All patients underwent follow-up for 1–50 months, which showed that the flap matched well with the surrounding skin with regard to color, texture, and contour without tumor recurrence. The incision line was hidden and the scar became smooth and soft. All patients obtained satisfactory functional and esthetic results.
Conclusions: The BWASF requires fewer aid incisions and the flap transitioned naturally and smoothly with satisfactory appearance and cosmetic reconstruction effects in this series of facial defects.
Keywords
Face; Skin defect; Local flap; Burow’s wedge advancement; Skin flap
Often, after excision of tumors or scars on facial skin, defects of different sizes remain. Small defects can be sutured directly. However, often a free skin graft or skin-flap transplantation to cover the wound is required. The local flap has appropriate color and texture compared with the surrounding skin and does not cause secondary defects or deformity, so is given priority for reconstruction of facial defects.
Since August 2000, based on the principles of total excision of tumors and zonation repair on the face, we undertook 156 facial soft-tissue reconstructions applying Burow’s wedge advancement skin flap (BWASF) after excision of facial tumors and scars. We carried out this retrospective study to summarize our experience of applying BWASF in reconstruction of facial defects.
Material and Method
Clinical data
Between August 2000 and August 2012, 156 cases (72 male and 84 females; mean age, 48 (range, 12–85) years) were reviewed. Facial skin tumors comprised 43 basal cell carcinomas, 33 squamous cell carcinomas, 24 epidermal cysts, 38 pigmented naevae, and 18 scars (Table 1). We designed monolateral advancement flaps in 108 cases and bilateral advancement flaps in 48 cases. In 33 cases, the defect was in the preauricular region, on the lips in 37 cases, on the temple in 13 cases, on the lower eyelid in 17 cases, on the forehead in 35 cases, and on the nasal side in 21 cases (Table 2). Patients with malignant tumors were of clinical stage 0–I with a history ranging from 1 week to 1 month. The area of the defect (in cm) ranged from 1.0 × 2.0 to 3.5 × 6.0.
| Study population | Value |
|---|---|
| Total No. patients | 156 |
| No. female patients | 84 |
| No. male patients | 72 |
| Age (yrs) | |
| Average | 48 |
| Range | 12~85 |
| Tumor | |
| Basal cell carcinoma | 43 |
| Squamous cell carcinoma | 33 |
| Pigmented naevus | 38 |
| Epidermal cyst | 24 |
| Scar | 18 |
Table 1: Patient profiles, and the numbers of facial skin tumors.
| Type of flap | Number of cases (n=156) | |||||
|---|---|---|---|---|---|---|
| Lip (n=13) | Preauricular (n=33) | Temple (n=37) | Lower eyelid (n=17) | Forehead (n=35) | Nasal side (n=21) | |
| Monolateral advancement flaps | 7 | 28 | 24 | 12 | 23 | 15 |
| Bilateral advancement flaps | 6 | 5 | 13 | 5 | 12 | 6 |
Table 2: Types of local flaps used in all patients
Surgical methods
Under general anesthesia or local anesthesia, complete excision of the facial nevus, tumor, or scar was achieved. Pathology confirmed that there were no nevus cells or residual tumor cells left in the margin and base. According to the region of the defect and the elasticity of neighboring skin, we designed the position of the BWASF and the incision line along natural facial contour lines (nasolabial fold, nose trenches, nose and jaw joints, margin, vermilion border, hairline) or skin wrinkles. After the flap was advanced to cover the defect completely, the distal flap was sutured with the periosteum or fascia of the contralateral side. Then a skin wedge of the contralateral side of the pedicle flap was resected to eliminate the “dog ears” deformity. Skin and subcutaneous tissue were sutured separately (Table 3).
| Predetermined satisfaction grades | Satisfaction level (%) |
|---|---|
| “Very satisfied” (A) | 127 |
| “Satisfied” (B) | 29 |
| “Unsatisfied” (C) | 0 |
Table 3: Types of local flaps used in all patients
Complete healing was observed in patients with malignant tumors of clinical stage I. Patients showed a satisfactory face contour and visual effect during the follow-up period (1–50 months). The flap matched well with surrounding tissues about color, texture, and contour, and tumor recurrence was not observed. The incision line was hidden and the scar was smooth and soft. No secondary defects or deformity on the face was observed. All cases had a satisfactory face contour and esthetic results.
Typical case 1
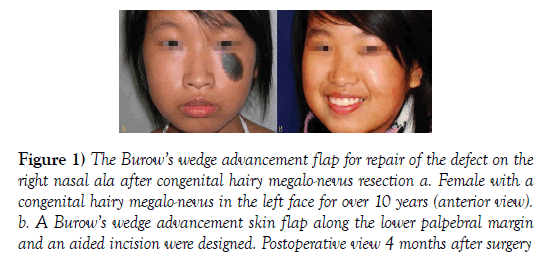
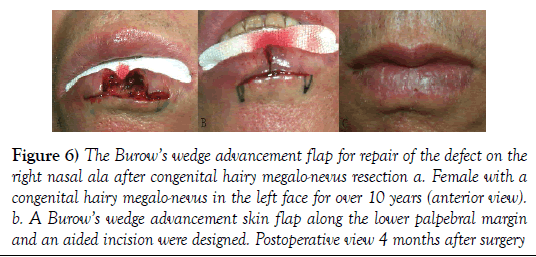
A 14-year-old female with a congenital hairy megalo-nevus on the left side of the face for >10 years was admitted to our hospital. Physical examination showed a black lesion measuring (in cm) 2.5 × 4.5 on the left zygomatica region with a clear border and upper margin near the lower palpebral margin. It had a flat, hairy surface without rupture. After conventional resection, a BWASF along the lower palpebral margin and an aided incision were designed. Then, the flap at the bottom of the incision was dissected and advanced to the wound. A wedge resection in the pedicle was created. After the edge was trimmed, the wound was sutured. On follow-up, satisfactory facial morphology and esthetic results were achieved (Figures 1a and 1b).
Figure 1: The Burow’s wedge advancement flap for repair of the defect on the right nasal ala after congenital hairy megalo-nevus resection a. Female with a congenital hairy megalo-nevus in the left face for over 10 years (anterior view). b. A Burow’s wedge advancement skin flap along the lower palpebral margin and an aided incision were designed. Postoperative view 4 months after surgery
Typical case 2
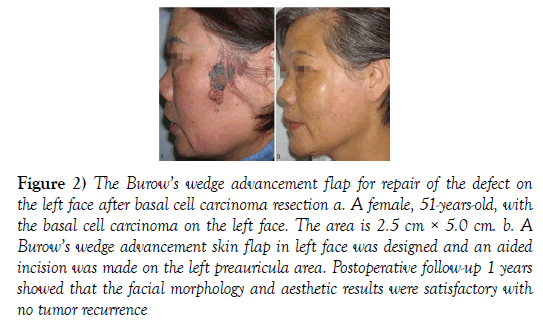
A 51-year-old female with a lump on the left facial area for >1 month was admitted to our hospital. Physical examination revealed a black lesion with pale-red areas, measuring (in cm) 2.5 × 5.0 on the left cheek. The border was unclear and the surface was rugged and partly ruptured. The lump was resected with a 1.0-cm margin and was diagnosed pathologically as basal cell carcinoma. No tumor cells in the margin or base were found. A BWASF on the left facial area was designed and an aiding incision made on the left preauricular area. The left facial skin was dissected and moved upwards to cover the wound. A wedge resection in the posterior auricular area was made to favor advancement of the flap. Postoperative follow-up showed that the facial morphology and esthetic results were satisfactory without tumor recurrence (Figures 2a and 2b).
Figure 2: The Burow’s wedge advancement flap for repair of the defect on the left face after basal cell carcinoma resection a. A female, 51-years-old, with the basal cell carcinoma on the left face. The area is 2.5 cm × 5.0 cm. b. A Burow’s wedge advancement skin flap in left face was designed and an aided incision was made on the left preauricula area. Postoperative follow-up 1 years showed that the facial morphology and aesthetic results were satisfactory with no tumor recurrence
Discussion
The face is an exposed, distinctive structure communicating with the outside world. Facial morphologic features have a direct impact on the visual impression and the patient’s state of mind. However, trauma, tumor excision, and scar removal often lead to facial soft-tissue defects that necessitate reconstruction by plastic surgeons (1). In general, the desired results of cosmetic reconstruction of facial skin defects should not change facial morphology or result in shifting or deformity of anatomic markers. Aiding incisions should be few and well concealed, flaps should match well with surrounding tissues with regards to color, texture, and contour, and there should be no secondary defects (2).
In achieving cosmetic results in reconstruction of soft-tissue defects, the tissues surrounding or adjacent to the defect should be the same or like the skin surrounding the wound in color, texture, and structural characteristics. The facial skin must be abundant in blood supply; the various regional flaps can be used to reconstruct moderate defects with no secondary deformity and a better face shape for functional and cosmetic results (3,4).
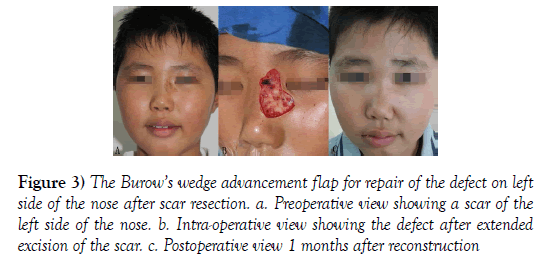
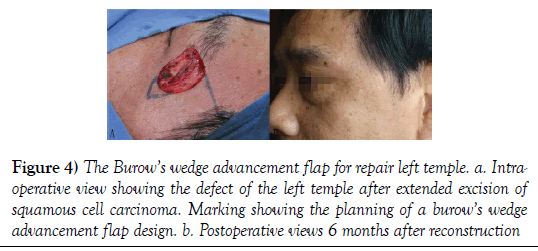
Various regional and adjacent flaps can be used to repair facial skin defects to achieve “ideal” effects, such as an “A-T” flap, modified rhomboid skin flap, “kite” flap, rotation flap, adjacent island flap and “V-Y” advancement flap, among others. It is imperative to reduce and hide the aiding incisions, guarantee sufficient blood supply, and ensure that the flap transitions naturally and smoothly. The BWASF can be employed for facial skin and soft-tissue defects, and can achieve a better cosmetic result for reconstruction (Figures 3–6).
Figure 3: The Burow’s wedge advancement flap for repair of the defect on left side of the nose after scar resection. a. Preoperative view showing a scar of the left side of the nose. b. Intra-operative view showing the defect after extended excision of the scar. c. Postoperative view 1 months after reconstruction
Figure 4: The Burow’s wedge advancement flap for repair left temple. a. Intraoperative view showing the defect of the left temple after extended excision of squamous cell carcinoma. Marking showing the planning of a burow’s wedge advancement flap design. b. Postoperative views 6 months after reconstruction
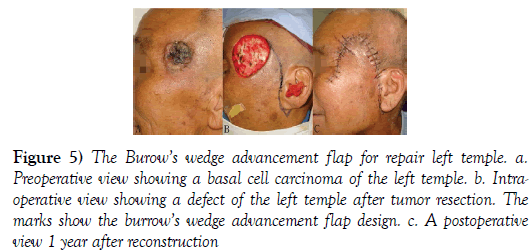
Figure 5: The Burow’s wedge advancement flap for repair left temple. a. Preoperative view showing a basal cell carcinoma of the left temple. b. Intraoperative view showing a defect of the left temple after tumor resection. The marks show the burrow’s wedge advancement flap design. c. A postoperative view 1 year after reconstruction
Figure 6: The Burow’s wedge advancement flap for repair of the defect on the right nasal ala after congenital hairy megalo-nevus resection a. Female with a congenital hairy megalo-nevus in the left face for over 10 years (anterior view). b. A Burow’s wedge advancement skin flap along the lower palpebral margin and an aided incision were designed. Postoperative view 4 months after surgery
The Burow’s wedge flap (5,6) is a modified advancement flap introduced first by Lisfranc in 1835 and von Burow in 1855. The flap makes full use of the ipsilateral skin of the defect and advances it to cover the wound without affecting the contralateral skin. The triangular skin and subcutaneous tissues in the pedicle should be resected to keep the skin flat. Major advantages are fewer and relatively concealed aiding incisions, wide base of the flat skin with sufficient blood supply, and ideal match between the flap and surrounding skin with no secondary deformity. It is suitable mainly for reconstruction of defects in temporal and paranasal regions, cheek, lower eyelid, forehead, and lips.
Conclusion
Based on evaluation of 156 patients, we came to six main conclusions. First, only one aided incision is needed in application of BWASF. Thus, it greatly reduces postoperative facial scars compared with methods used previously. The aided incision should be designed along the natural facial contour line (nasolabial fold, paranasal ala sulcus, maxillonasal suture, margines palpebrales, vermilion border, preauricular hair line) or skin wrinkles, which helps to hide the incision line as much as possible (7,8). Second, the flap is designed on the same side of the defect to ensure that tissues of the contralateral side avoid malposition or deformity. Especially for defects close to the palpebral margin, lip and nose, it is even better if the flap is designed away from anatomic markers with flabby skin. Due to an essentially horizontal advancement, there is no significant rotation or twisting of the flap. The skin transitions naturally and smoothly without pedicle distension or deformity (dog ears) (9). Third, it is not necessary to shape the wound into a triangle or circle if resecting facial scars or tumors. Instead, the incision should be designed along the border of the scar and tumor. In addition, the cutting edge should be designed in a “zig-zag” or curved manner to avoid straight incisions. Fourth, in general, the pedicle of the flap is broad with an abundant blood supply. Thus, the flap may be freed more widely to lessen the tension. Under certain circumstances, the distal flap can be sutured with the periosteum or fascia of the contralateral tissue, which may prevent or reduce tissue/organ malposition and deformity of the contralateral skin. Fifth, for defects in some regions such as the lips and frontal area, double Burow’s wedge advancement flaps can be designed to better reconstruct the defect and maintain the morphology and function of surrounding tissues (10). Finally, a wedge of skin of the contralateral side should be resected to eliminate the dog-ears deformity, which we carry out after the wound is covered to reduce the amount of resected skin.
Acknowledgement
None.
Conflict of Interest
None.
REFERENCES
- Nabili V, Knott PD. Advanced lip reconstruction: Functional and aesthetic considerations. Facial Plast Surg. 2008;24(1):92-104.
- Kaufman AJ. Bilateral vermilion rotation flap. Dermatol Surg. 2006 32(5):721-25.
- Demir Z, Yüce S, Karamürsel S, et al. Orbicularis oculi myocutaneous advancement flap for upper eyelid reconstruction. Plast Reconstr Surg. 2008;121(2):443-50.
- Iseli TA, Rosenthal EL. Reconstruction of periauricular and temporal bone defects. Facial Plast Surg Clin North Am. 2009;17(2):253-62.
- Yenidunya MO, Demirseren ME, Ceran C. Bilobed flap reconstruction in infraorbital skin defects. Plast Reconstr Surg. 2007;119(1):145-50.
- Xue CY, Li L, Guo LL, et al. Combined flaps for reconstructing wide-range facial defects. Aesth Plast Surg. 2011;35(1):13-18.
- Xue CY, Li L, Guo LL, et al. The axial frontonasal flap for reconstruction of large nasal-tip defects based on modified nasal subunits in East Asians. Clin Exp Dermatol. 2009;34(3):426-28.
- Birgfeld CB, Chang B. The periglabellar flap for closure of central forehead defects. Plast Reconstr Surg. 2007;120(1):130-33.
- Wang SQ, Goldberg LH. Burow's wedge advancement flap for lateral forehead defects. Dermatol Surg. 2006;32(12):1505-08.
- Sachithanandam K, Ilango N, Gupta AK. Effective use of Burow's triangle in a nasolabial flap– A technique. J Plast Reconstr Aesthet Surg. 2009;62(6): 853-54.