Association of episodic psychotic behaviour with an arachnoid cyst of the brain “A rare case report”
Received: 06-Aug-2018 Accepted Date: Sep 27, 2018; Published: 03-Oct-2018
Citation: Guliani GS. Association of episodic psychotic behaviour with an arachnoid cyst of the brain “A rare case report”. J Child Adolesc Psych 2018;2(3):01-02.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Until recently, the coexistence of arachnoid cysts in the brain with psychiatric disturbances had not been closely covered in the literature. However, there are some references that focus on a possible link between arachnoid cysts and psychotic symptoms. The purpose of this case report is to suggest a relationship between such lesions and psychiatric illness. This is an effort to bring the possibility of association of arachnoid cyst in a patient presenting with psychotic signs and symptoms to a mental health physician.
Case presentation: Arachnoid cysts are considered a rare neurological tumor, few of which exhibit any symptomatology. This is a case report of a 23-year-old North Indian male with no previous psychiatric history that presented with abrupt onset of psychosis. The workup for medical etiology was within normal limits, but on a brain scan there was well defined arachnoid cyst in the occipital region. The patient best responded to the second generation antipsychotic risperidone.
Conclusion: Clinically the association of psychotic features with the rare structural lesion in the brain is significant because many psychiatric cases go misdiagnosed and untreated if there is a concealed neurological or organic cause. Such cases often go reported as treatment refractory because our eyes see what our mind thinks. It’s rare to find association of arachnoid cyst with the psychiatric condition but keeping this as a possibility in mind can be rewarding.
Keywords
Arachnoid cyst; Episodic psychosis; Olanzapine; Risperidone
Arachnoid cyst has been reported to occur nearly in 1.4% of the general population on brain MRI studies [1]. They can be located along the craniospinal axis with a predilection for the temporal fossa [2]. Aetiology of a psychotic disturbance can be due to a functional or organic condition. Arachnoid cysts are rare, benign space-occupying lesions formed by an arachnoid membrane containing cerebrospinal fluid (CSF). Intracranial arachnoid cysts are mostly congenital. In most cases, they are diagnosed accidentally. There is a sex dependency on some intracranial locations of arachnoid cysts, with temporal cysts occurring more frequently in men, and cerebellopontine cysts found more frequently in women [3]. Many articles have also reported patients with intracranial arachnoid cysts presenting with psychiatric illness as their main symptom. They usually arise in areas that are rich in arachnoid, and 50% are located in the sylvan fissure [4]. Arachnoid cyst seems to impair not only basic cognition but also executive functions. Most of this impairment can be surgically corrected if indicated [5]. The discovery of such an arachnoid cyst in a person with a psychotic disorder raises diagnostic and therapeutic issues that are extremely significant from a clinical point of view.
Case Presentation
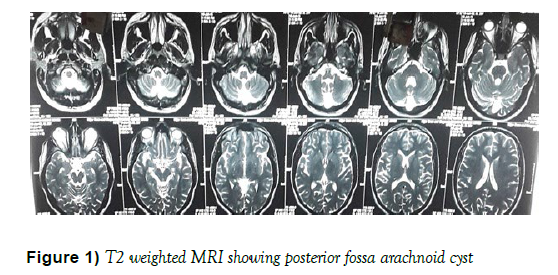
A 23-year-old male with no previous psychiatric history presented to the psychiatry OPD with the complaints of episodic heaviness in the head, loud involuntary laughter, flushing of face associated with a sudden change of laughter into a loud cry from the last 28 days. The episode lasted about 10-15 min. The episode was associated with loss of control over his body and actions without loss of consciousness. During the episode, the patient’s blood pressure was between 180-200 (systolic) by 100-120 (diastolic) mmHg. After the episode weaned off, his blood pressure came back to normal. During his first episode, the patient suddenly started laughing loudly and started banging his head against the wall. He was so aggressive that it took four people from his family to control him. After the episode weaned off the patient was relieved from the heaviness of head and felt asleep thereafter. On the interview, the patient was not able to clearly recollect the episode. However, he could only remember the heaviness of head with a feeling of a loss of control just before the episode. Slowly the episodes increased in frequency to four episodes per day over the following 4-5 days and there were similar signs and symptoms in all the episodes. During the episode, there were no tonic-clonic movements of any body part of the body, no fixed gaze, no nystagmus, no loss of consciousness, no frothing from the mouth and no incontinence of bladder or bowel. No hallucinations were reported by the patient during or after the episode or during his lifetime. There was no recent/past history of any trauma, mood disorder and no apparent stressor of any kind. No history of any substance abuse. No history of diabetes, hypertension, asthma, tuberculosis or any regular or long-term medication use. On Mental State examination, the patient was oriented to time, place and person. There was no change in psychomotor activity. There were no perceptional disturbances. Thoughtform, content, and stream were normal. The patient mood was euthymic. Patient MMSE was 29/30. On neurological examination, reflexes were normal with no neurological deficit. The patient was referred for MRI brain. The scan revealed retro-cerebellar arachnoid cyst measuring 3.9 x 2.3 x 1.8 cm in size with mild scalloping of overlying occipital bone was found (Figure 1).
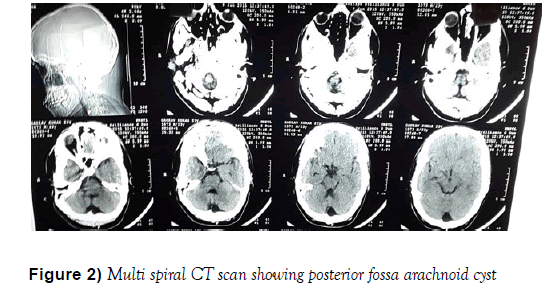
On ophthalmology examination, no papilledema was seen on fundoscopy and intraocular pressure was not raised. EEG did not reveal any abnormality in photic stimulation and sleep deprivation. Baseline investigations (including blood work, serum electrolytes, liver function test, renal function test, ECG, lipid profile, Hb1Ac, random blood glucose levels) were within normal range. The patient was consulted for neurosurgical opinion and was advised multi-spiral CT scan (Figure 2), but the neurosurgical department opted against surgical intervention at this stage.
The patient was started on tablet olanzapine 5 mg orally once daily but no response was seen after 7 days of drug initiation and henceforth the dose was increased up to 10 mg /day. Episodes still continued with the same frequency but aggression was decreased during the episodes. The patient has switched on risperidone 2 mg once daily and olanzapine was tapered slowly and then was completely stopped in next 5 days while risperidone was increased up to 4 mg per day. The patient tolerated risperidone well without any sign of extrapyramidal symptoms and also showed a significant improvement on risperidone. His duration of episodes was decreased to 1-2 episodes/ day in the following 2 weeks with less severity compared with the previous 4-5 episodes /day but without complete remission. Finally, the patient was discharged on risperidone 4 mg / daily with significant improvement in the quality of his life.
Conclusion
With the advent of neuroimaging, there has been an increased incidence of detection of incidental asymptomatic arachnoid cysts. Although these lesions are considered congenital, the exact aetiology is still not clear. The arachnoid cyst is a benign congenital collection of cerebrospinal fluid that accounts for about 1% of all space-occupying non-traumatic intracranial lesions [4]. The principal location is the temporal fossa. The clinical signs and symptoms of the cyst, if any (it is often an incidental finding), depending on the cyst’s location, size and on the patient’s age. This case report discusses the possibility of a causal relationship between the arachnoid cyst and the patient’s psychotic symptoms. It is possible that the patient’s cerebral lesion was superimposed upon an underlying psychiatric disorder, and that the brain lesion was an incidental finding without functional importance. Although limited by the absence of definite information about the development of the cystic lesion, we conclude that the patient’s abnormal behaviour was associated with an arachnoid cyst for the following reasons: (i) No past and familial psychiatric history and it was the first abrupt onset of episode; (ii) Psychotic symptoms accompanied with a severe headache (iii) No other clinically relevant findings were seen (iv) Cases presenting with schizophrenia-like psychosis associated with an arachnoid cyst [6], furthermore, recently Lanczik et al. reported a schizophrenia-like psychosis associated with an arachnoid cyst which mainly affected the left temporal lobe [7]. This might support our case report even though the evidence is inadequate as described above. Another interesting finding of the present case was the effectiveness and safety of low-dose risperidone treatment in the space-occupying lesion. This finding would support atypical antipsychotics like risperidone being used as alternative agents to typical antipsychotics for the treatment of psychosis related to organic aetiology. With the progression of modern imaging techniques; psychiatrists will discover an increasing number of structural brain abnormalities, which inevitably raises the question about the relationship of psychiatric disorders to the organic brain findings. In the future, more accurate diagnostic tools and techniques which integrate clinical manifestations and structural findings will increase the diagnostic reliability and validity. In the case described, the sudden onset of psychotic symptoms in a patient without personal or family antecedents of psychosis enables us to evaluate the possibility of a causal relationship between the arachnoid cyst discovered by brain imaging and the set of symptoms. Despite the rarity of arachnoid cysts, there are other case reports of patients with associated psychotic symptoms that could be explained by pressure generated by the cyst. Although the cyst seems to be congenital, it does not cause any symptoms earlier in life. According to current clinical practice, there are two aspects to the therapeutic approach of organic psychotic disorders: (i) Conservative i.e. controlling the symptoms, (ii) correcting the etiological situation. In this specific case of arachnoid cysts, the need for a surgical approach is neither clear nor uniform: Intracranial hypertension or progressive hydrocephaly is usually the situations where surgery is mandatory and stricter indications are there for the surgical approach in intracranial arachnoid cyst [8]. If neither of these indications is present and there are no focal neurological signs, given both the morbidity associated with surgery and the fact that this type of lesion can disappear spontaneously, the attitude is generally conservative. Although arachnoid cysts are symptomatic in a small number of patients, they are associated with a benign natural history for those presenting without symptoms [1]. However, an analysis of the literature shows that conservative management is the most frequently adopted option; there has been a case in which surgical intervention was specifically adopted as a therapeutic approach to the psychotic symptoms.
Declaration
Ethics approval and consent to participate: consent was taken from the patient in his own language and approval for the study was taken from the ethical committee of Government Medical College and Hospital Amritsar.
Competing Interest
The authors declare that they have no competing interests.
Author’s Contributions
GGS interviewed the patient, taken a detailed history, admitted patient under him and his team supervision, GR helped in drafting the manuscript and analyzing the data. GH helped in daily progression notes, taken care of interdepartmental consultations and performed literature searches along with helping in finalizing the manuscript. All authors read and approved the final manuscript
REFERENCES
- Al-Holou WN, Terman S, Kilburg C, et al. Prevalence and natural his-tory of arachnoid cysts in adults. J Neurosurg 2013;118(2):222-31.
- Wester K. Peculiarities of intracranial arachnoid cysts: location, sidedness, and sex distribution in 126 consecutive patients. Neurosurgery 1999;45(4):775-9.
- Helland CA, Lund-Johansen M, Wester K. Location, sidedness and sex distribution of intracranial arachnoid cyst in a population-based sample. J Neurosurg 2010;113(5):934-9.
- Gelabert-González M. Intracranial arachnoid cysts. Rev Neurol 2004;39(12):1161-6.
- Gjerde PB, Schmid M, Hammar A, et al. Intracranial arachnoid cysts: impairment of higher cognitive functions and postoperative improvement. J Neurodev disord 2013;5(1):21.
- Baquero GA, Molero P, Pla J, et al. A Schizophrenia-like psychotic disorder secondary to an arachnoid cyst remitted with neurosurgical treatment of the cyst. Open Neuroimaging J 2014;8:1-4.
- Lanczik M, Fritze J, Classen W, et al. Schizophrenia-like psychosis associated with an arachnoid cyst visualized by mapping of EEG and P300. Psychiatry Res 1989;29(3):421-3.
- Choi JW, Lee JY, Phi JH, et al. Stricter indications are recommended for fenestration surgery in intracranial arachnoid cysts of children. Childs Nerv Syst 2015;31(1):77-86.