Attention deficit hyperactivity disorder in children and adolescents with co-morbid anxiety and depression
Citation: Shroff KP, Sanchez-Lacay JA. Attention deficit hyperactivity disorder in children and adolescents with co-morbid anxiety and depression. Clin Psychol Cog Sci. 2018;2(1):17-24.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: This paper reviews the prevalence and effects of anxiety and depression as comorbid conditions in children and adolescents having attention deficit hyperactivity disorder (ADHD) and to understand their implication on social, behavioral and emotional functioning of such children.
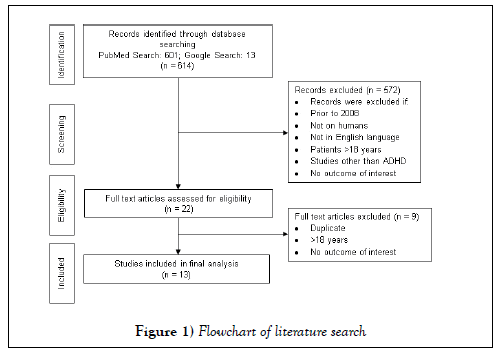
Methods: A detailed search of published literature in English language and studies on humans was performed using electronic databases such as MEDLINE (via PubMed) and Google, from 2008 to 2018 using relevant search terms. A total of 10 original studies and systematic review articles were retrieved for potential inclusion.
Results: Children and adolescents having ADHD reported relatively higher prevalence rates and severe symptoms of comorbid anxiety and depression compared to controls. Self-reporting of more severe ADHD symptoms was seen in parents of children having ADHD than parents of children not having ADHD. ADHD with comorbid anxiety or depression in children and adolescents is associated with significant impairments in health, sleeping patterns, social life and academic functioning. Poorer social functioning among young adolescents with ADHD is mainly caused due to depression.
Conclusion: Early diagnosis, long-term monitoring, and proper treatment may help in reducing social anxiety and functional impairment in children and adolescent with comorbid anxiety and depression. The primary care clinician should recognize ADHD as a chronic condition and consider children and adolescents having ADHD as children and youth with special health care needs. These inherent, biological, and social factors accountable for the complex correlations could be extricated with the help of longitudinal studies.
Keywords
Attention deficit hyperactivity disorder; Children; Adolescents; Anxiety; Depression
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is the most commonly diagnosed neurodevelopmental disorder in pediatric psychiatry and appears to be more challenging to diagnose and treat when there is comorbid anxiety and depressive disorder. ADHD is complicated by its heterogeneity, and evidence suggests high levels of comorbidity between ADHD and conduct disorder (30-50%), oppositional defiant disorder (40-50%), depression and anxiety disorders (15-75%) [1]. Both ADHD and depression/ anxiety are associated with significant impairments in health, social life and academic functioning [2,3].
ADHD is considered as an important public health issue as it not only impairs the performance of an individual but may affect both the family and social life [4]. Given the controversy of whether ADHD is over diagnosed or under diagnosed, a worldwide meta-analysis of 175 research studies on ADHD prevalence in children aged 18 and under was undertaken. Findings from that study reported an overall pooled estimate of 7.2% which exceeds the 5.3% estimate reported in previous studies [5]. According to the 2016 National Survey of Children’s Health, about 9.4% (6.1 million) children aged 2-17 years have been diagnosed with ADHD in United States [6]. In the UK, a survey of 10,438 children between the ages 5 and 15 years found that 3.62% of boys and 0.85% of girls had ADHD [7].
Comorbid anxiety and depression are also prevalent among the adolescents having ADHD. At least 60% of children having ADHD meet criteria for ≥ 1 comorbid disorder [8]. Atleast one anxiety disorder like social, separation or generalized anxiety is found in 25%-50% of children suffering from ADHD [9,10]. Further, individuals having comorbid ADHD and anxiety have worse working memory deficits, worse overall functioning, poorer psychosocial quality of life, and a lower response rate to stimulant treatment [11-14] than those with pure ADHD. Existing research has suggested that children with ADHD and anxiety are less impulsive [15,16] but these children have more attention and broader cognitive functioning difficulties [14,17] than those having ADHD alone.
The exacerbation of executive functioning issues along with avoidance and negative thought patterns impairs social behavior and relationship with family and friends causing anxiety [18]. It has been suggested that anxiety is caused by impairment in mesolimbic, mesocortical, and nigrostriatal cycles due to impairment in the physiology of nucleus accumbens in ADHD [19]. Epidemiological studies have reported ADHD to be significantly associated with somatic complains. Children often use somatic complaints as a way to verbalise or express distress [20] and children with emotional disorders such as depression and anxiety more frequently report somatic complaints [21].
In addition to anxiety, ADHD becomes more difficult to diagnose and treat in presence of a comorbid depressive disorder. Studies indicate prevalence rates of 9% to 38% for depressive disorders in children having ADHD [22-24]. In community samples, prevalence of depression among patients with ADHD was estimated to be 13% to 27%, while clinical samples reported prevalence as high as 60% [25-27]. Conversely, in children and adolescents with depression, prevalence rate of ADHD has been reported to be varying extensively from less than 5% to more than 50%. This is supported by a study which reports a 42% ADHD rate in very young children [28,29]. It has been suggested that depression in ADHD is linked to ADHDassociated demoralization i.e., low self-esteem associated to academic and social performance [30]. Further, the relationship between depression and ADHD may vary as a function of moderating variables (sex, age, comorbid oppositional deficient disorder), ADHD subtype, and data source (doctor, child, parent and teacher). Evidence suggests that depression scores are significantly correlated (p<0.001) with ADHD-Inattentive (ADHD-I) subtype than with ADHD-Hyperactive (ADHD-H) subtype. However, when these correlations within different age groups like younger than 10 years, 10 to 14 years, and older than 14 years were considered, it was observed that distinctly widespread differences in correlation between depression and ADHD subtypes stayed only for the youngest group (p<0.0001).
This highlights the significance of considering behaviors which can be normed by age [31]. This paper reviews the prevalence and effects of anxiety and depression as comorbid conditions in children and adolescents with ADHD and to understand their implication on social, behavioral and emotional functioning of such children.
Methodolgy
In order to identify and retrieve potentially relevant published literature, an electronic search of the literature was conducted from 2008 to 2018 on MEDLINE (via PubMed) and Google search database, using the search terms such as: “Attention-Deficit Hyperactivity Disorder or attention deficit disorder with hyperactivity or attention deficit disorders or ADHD, child, children or adolescents, or prevalence or comorbidity or multimorbidity, anxiety or anxiety disorder, depression or depressive disorder”. Publications in English language and studies performed on humans were retained for further evaluation. The search yielded [22] original studies and systematic review articles which were screened using the following inclusion and exclusion criteria, and as detailed in the Figure 1.
Inclusion criteria for the study
• Studies that included ADHD children and adolescents as patients.
• Studies that evaluated the prevalence of comorbid anxiety or depression in ADHD.
• Studies that evaluated the effects of comorbid anxiety or depression in ADHD in terms of behavior, functioning and social-skills.
• Studies on humans, in English language and published between 2008- 2018.
Exclusion criteria for the study
• Studies that included young or adult ADHD patients.
• Studies that included comorbid psychological disorders other than anxiety and depression such as bipolar disorder, obsessive compulsive disorder.
• Studies not on human subjects.
• Study types to be excluded: Editorials, letters, addresses, bibliographies, biographies, comments, dictionaries, directories, interviews, legal cases, legislation, news, patient education materials, periodical indices, case series and case reports.
• No outcomes of interest (e.g., pharmacokinetic studies).
Results
The final detailed examination of our study included 13 independent studies as described in (Table 1).
| Sr. No. | Author | Study type | Study population | Age | Prevalence |
|---|---|---|---|---|---|
| 1 | Gumus et al. [39] | Cohort study | 170 children and adolescents | Age range: 6-12 years Mean age: (Mean ± SD): 9.0 ± 2.3 | Overall ADHD with Anxiety: 27.6% |
| Girls with ADHD and Anxiety: 39.4% | |||||
| Boys with ADHD and Anxiety: 24.8% | |||||
| 2 | Tung et al. [40] | Meta-analysis | 1997 girls | Mean age range: 8.5-13.5 years | Girls with ADHD and Anxiety: 37.7% |
| Girls with ADHD and Depression: 10.3% | |||||
| 3 | Selinus et al. [33] | Longitudinal cohort study | 4635 twins | Age range: 9-12 years | Girls with ADHD and Internalizing problems: 44.3% |
| Boys with ADHD and internalizing problems: 14.8% | |||||
| 4 | Xia et al. [32] | Case control study | 200 children | Age range: 7-10 years | ADHD and Anxiety: 27.4% |
| ADHD and Depression: 17.8% | |||||
| Comorbid Anxiety and Depression: 14.8% | |||||
| 5 | Hu et al. [35] | Cross-sectional analysis | 287 adolescents | Age range: 11-18 years Mean age: (Mean ± SD): 13.1 ± 2.0 | ADHD and Anxiety: 10.5% |
| ADHD and Depression: 6.3% | |||||
| 6 | Leirbakk et al. [21] | Cross-sectional health survey | 12900 children | Age range: 8-13 years | Comorbid Anxiety and Depression: 29.6% |
| 7 | Larson et al. [41] | Cross-sectional analysis | 61779 children | Age range: 6-17 years | ADHD and Anxiety: 18% |
| ADHD and Depression: 14% | |||||
| 8 | Anastopoulos et al. [38] | Cohort study | 358 children | Mean age: 8.7 years | ADHD and Separation Anxiety: 11.4% |
| ADHD and Generalized Anxiety: 6.1% | |||||
| ADHD and major depression/dysthymic disorder: 3.8% | |||||
| 9 | Mikami et al. [62] | Cohort study | 62 children | Mean age: 8.26 ± 1.21 years | ADHD and comorbid anxiety/depression: 17.7% |
| 10 | Mikami et al. [63] | Randomized clinical trial | 24 children | Mean age: 8.15 ± 0.79 years | Comorbid depressive and/or anxiety: 16.7% |
| 11 | Bussing et al. [42] | Cohort study | 94 adolescents | Age range: 5-11 years | Comorbid Anxiety and Depression: 13% |
| 12 | Becker et al. [34] | Cohort study | 215 children | Mean age: 8.30 ± 1.31 years | ADHD and Anxiety: 17% |
| ADHD and Depression: 4% | |||||
| Comorbid Anxiety or depression: 18% |
Table 1: Patient characteristics of the included studies
Although the initial search included studies published since 1989, all of the final 13 studies included were in or after 2008. Studies which included any ADHD subtype in the ADHD group, and diagnoses were typically based on a diagnostic interview using validated instruments or an interview along with rating scale as described in Table 2.
| Sr. No. | Author | Study type | Instruments used | Findings | Conclusion | ||
|---|---|---|---|---|---|---|---|
| Parameter | Statistic | p value | |||||
| 1 | Hu et al. [35] | Cross-sectional analysis | MASC-T, CES-D, SNAP-IV, C-SBEQ, BIS, BAS | Correlates of anxiety and BIS score | β=0.495, t=9.406 | p<0.001 | Behavioral temperamental traits as examined on the BIS, comorbid ASD, and bullying involvement are significantly associated with anxiety and depression in adolescents with ADHD. |
| Correlates of severity of anxiety and bullying involvement: | |||||||
| – Bullying victim | β=0.202, t=4.050 | p<0.001 | |||||
| – Bullying perpetrator | β=0.068, t=1.407 | p=0.161 | |||||
| Correlates of depression and BIS score | β=0.313, t=5.204 | p<0.001 | Clinicians, educational professionals, and parents should monitor the symptoms of anxiety and depression in adolescents with ADHD who exhibit the correlates of anxiety and depression identified in this study so that appropriate action may be taken. | ||||
| Correlates of severity of depression and bullying involvement: | |||||||
| – Bullying victim | β=0.190, t=3.454 | p=0.001 | |||||
| Bullying perpetrator | β=0.228, t=4.308 | p<0.001 | |||||
| 2 | Selinus et al. [33] | Longitudinal cohort study | A-TAC, SDQ, Olweus Bully Victim Questionnaire, Self-Reported Delinquency scale, Substance abuse self-reported alcohol and drug use measure | Psychosocial outcomes | Values are adjusted odds ratios reported as OR (95%CI). | The study necessitates the need to consider gender-specific risks for negative development during adolescence among children with ADHD symptoms. | |
| Girls: | |||||||
| – Internalizing problems | 1.39 (1.10-1.77) | ||||||
| –Peer problems | 1.47 (1.13-1.92) | ||||||
| –School problems | 1.90 (1.38-2.63) | ||||||
| –Drug misuse | 1.52 (1.14-2.03) | ||||||
| –Alcohol misuse | 1.14 (0.90-1.44) | ||||||
| –Antisocial behaviour | 1.86 (1.45-2.39) | ||||||
| Boys: | The study necessitates the need to consider gender-specific risks for negative development during adolescence among children with ADHD symptoms. | ||||||
| Internalizing problems | |||||||
| –Peer problems | 1.19 (0.91-1.56) | ||||||
| –School problems | 1.07 (0.86-1.33) | ||||||
| –Drug misuse | 1.68 (1.28-2.21) | ||||||
| –Alcohol misuse | 0.89 (0.66-1.20) | ||||||
| –Antisocial behaviour | 1.41 (1.16-1.71) | ||||||
| Increasing levels of ADHD symptom in childhood associated with higher proportions of adolescents who displayed negative psychosocial outcomes | 1.40 (1.16-1.68) | ||||||
| 3 | Larson et al. [41] | Cross-sectional analysis | The Aggravation in Parenting Scale | Odds of functioning: | Values are reported as OR (95%CI) | Clinical management of ADHD must address multiple comorbid conditions and a range of adverse functional outcomes. | |
| Activity restriction | 4.14 (3.34-5.15) | ||||||
| School problems | 5.18 (4.47-6.01) | ||||||
| Grade repetition | 3.71 (3.02-4.55) | ||||||
| Poor parent-child communication | 2.55 (1.84-3.52) | Therapeutic approaches should be responsive to each child’s neurodevelopmental profile, personalized to their unique social and family circumstances, and integrated with educational, mental health and social support services. | |||||
| Low social competence scores | 2.86 (2.46-3.31) | ||||||
| High parent aggravation | 4.30 (3.72-4.98) | ||||||
| Children with ADHD had higher odds of functioning compared to children without ADHD. | |||||||
| 4 | Becker et al. [34] | Cross-sectional analysis | RADS-2, MASC, BDI-II, SSIS, SPPC | Parent-reported scale scores for social functioning in young adolescents having ADHD with comorbid anxiety vs. those with ADHD without comorbid anxiety: | Relation between internalizing symptoms and social functioning among young adolescents with ADHD is nuanced | ||
| –Social skills | t=2.71 | p=0.007 | |||||
| –Social acceptance | t=2.52 | p=0.01 | |||||
| Parent-reported scale for young adolescents having ADHD with comorbid depression vs. those with ADHD without comorbid depression: | In terms of comorbid diagnoses, depression is more clearly related than anxiety to poorer social functioning among young adolescents with ADHD. These results point to the importance of attending to specific facets of anxiety and depression in clinical care and future research. | ||||||
| –Social skills | t=5.41 | p<0.001 | |||||
| –Social competence | t=3.49 | p<0.001 | |||||
| 5 | Anastopoulos et al. [38] | C-DISC-IV, CRS-R, BASC-2, Services Use in Children and Adolescents–Parent Interview | Odds of functional impairment indices: | Values are reported as OR (95%CI) | Deficits in the self-regulation of emotion are evident in a substantial number of children with AD/HD and that these deficits play an important role in determining functional impairment and comorbidity outcomes. | ||
| Social skills | 3.009 (1.584-5.716) | ||||||
| Daily living | 19.818 (7.243-54.223) | ||||||
| Adaptive skills composite | 6.336 (2.979-13.470) | ||||||
| Internalizing comorbidities | 5.716 (2.372-13.774) | ||||||
| Conduct problems | 4.753 (1.785-12.660) | ||||||
| Children with ADHD displayed significantly higher odds of functional impairment indices. | |||||||
| 6 | BussiNg et al. [42] | K-SADS-PL, VADPRS, BASC SRP, CIS, YQOL questionnaire, Pride Questionnaire for Parents, CASA | Functional and psychosocial indices | Values are reported as OR (95%CI) | Childhood ADHD heralds persistence of ADHD and comorbid symptoms into adolescence, as well as significant risks for functional impairment and juvenile justice involvement | ||
| Anxiety/Depression | 10.3 (2.7-39.3) | ||||||
| Clinical Maladjustment | p<0.0001 | ||||||
| School Maladjustment | p=0.0012 | Subthreshold ADHD symptoms typically do not qualify affected students for special educational interventions yet increase the risk for adverse educational outcomes. | |||||
| Grade retention | p<0.0001 | ||||||
| Alcohol abuse | p=0.1125 | ||||||
| Psychosocial Summary | p<0.0001 | Findings stress the importance of early ADHD recognition, especially its comorbid presentation with ODD, for prevention and intervention strategies. | |||||
| Overall functional impairment | 3.4 (1.7-6.9) | ||||||
| Functional and psychosocial indices were higher in children with childhood ADHD compared to the non-ADHD children. | |||||||
| 7 | Gumus et al. [39] | Cohort study | KSADS-PL, T-DSM-IV-S, WICS-R | WISC-R score for ADHD patients with AD vs. those without AD comorbidity | Z=1.68 | p=0.09 | Patients with ADHD had higher comorbidity rate of AD than general populaÂÂtion and clinical sample without ADHD. |
| T-DSM-IV-S score for | |||||||
| -Mothers of children with ADHD and AD comorbidity vs. those without AD | Z=0.573 | p=0.567 | The possibility of comorbidity of AD in patients with ADHD should be considered because higher rates of AD are observed in ADHD and comorbidities of AD. | ||||
| -Fathers of children with ADHD and AD comorbidity vs. those without AD | Z=0.469 | p=0.63 | |||||
| Teachers of children with ADHD and AD comorbidity vs. those without AD | T=2.19 | p=0.69 | |||||
| 8 | Leirbakk et al. [21] | Cross-sectional health survey | SDQ | Somatic complaints’ comparison between different groups: | Values are reported as OR (95%CI) | Prevalence of ADHD, depression/anxiety and comorbidity in children are generally consistent with those provided in previous research. | |
| Headache: | |||||||
| -Only ADHD group | 1.219 (0.426-3.493) | p<0.001 | |||||
| -ADHD with depression/anxiety group | 3.335 (2.039-5.455) | p<0.001 | |||||
| Abdominal pain | However, there is a need for understanding the development of psychopathology in children, in order to provide the best treatment. | ||||||
| -Only ADHD group | 1.641 (0.576-4.675) | p<0.001 | |||||
| -ADHD with depression/anxiety group | 4.919 (3.041-7.957) | p<0.001 | |||||
| Neck pain: | |||||||
| -Only ADHD group | 0.626 (0.085-4.625) | p<0.001 | |||||
| ADHD with depression/anxiety group | 4.867 (2.791-8.489) | p<0.001 | |||||
| 9 | Xia et al. [32] | Case control study | SACRED, DSRSC, ASRS, STAI, BDI, STAI-AD-SAI, STAI-AD-TAI | Mean total score on self-report anxiety in children with ADHD vs. without ADHD | 18.3 vs. 8.1 | p<0.001 | School-aged children with ADHD commonly suffer from comorbid anxiety and depressive disorders, and the severity of these symptoms parallels the level of anxiety and depressive symptoms in their parents. |
| Mean total score on self-report depression in children with ADHD vs. without ADHD | 10.8 vs. 3.1 | p<0.001 | |||||
| STAI-AD-TAI scores for mothers of children with ADHD vs. mothers of children without ADHD | t=3.20 | p<0.001 | |||||
| Correlation of anxiety symptoms of children with that of parents | r=0.58 | p<0.001 | |||||
| Correlation of depressive symptoms of children with that of parents | r=0.59 | p=0.030 | |||||
| Comparing fathers and mothers in ADHD group: | Self-reported symptoms of ADHD are significantly more common in parents of children with ADHD than in parents of children without ADHD. | ||||||
| - ASRS score | t=1.97 | p=0.050 | |||||
| -STAI-AD-SAI | t=1.97 | p<0.001 | |||||
| -STAI-AD-TAI | t=2.37 | p=0.020 | |||||
| -BDI | t=1.855 | p=0.068 | |||||
| Comparing fathers and mothers in control group: | Longitudinal studies are needed to disentangle the genetic, biological, and social factors responsible for these complex inter-relationships. | ||||||
| -ASRS score | t=0.38 | p=0.701 | |||||
| -STAI-AD-SAI | t=2.11 | p=0.039 | |||||
| -STAI-AD-TAI | t=0.66 | p=0.511 | |||||
| -BDI | t=0.91 | p=0.366 | |||||
| Severity of parent’s anxiety symptoms | β=1.071, t=8.43 | p<0.001 | |||||
| Severity of parent’s depressive symptoms | β=1.361, t=3.35 | p<0.001 | |||||
ADHD: Attention Deficit Hyperactivity Disorder; ADMASC: Multidimensional Anxiety Scale for Children; MASC-T: Taiwanese version of the Multidimensional Anxiety Scale for Children; CES-D: Center for Epidemiological Studies Depression Scale; SNAP-IV: Swanson, Nolan, and Pelham Version IV Scale; C-SBEQ: School Bullying Experience Questionnaire; BIS: Behavior Inhibition System; BAS: Behavior Approach System; A-TAC: Autism-Tics, ADHD, and other Comorbidities Inventory; SDQ: Strengths and Difficulties Questionnaire; RADS-2: Reynolds Adolescent Depression Scale, Second Edition; BDI-II: The Beck Depression Inventory-II; SSIS: Social Skills Improvement System; SPPC: Self-Perception Profile for Children; C-DISC-IV: Computerized Diagnostic Interview Schedule for Children, Fourth Edition; CRS-R: Conners’ Rating Scales; BASC-2: The Behavior Assessment System for Children-Second Edition; K-SADS-PL: Kiddie Schedule for Affective Disorder and Schizophrenia -Present and Lifetime Version; VADPRS: Vanderbilt ADHD Diagnostic Parent Rating Scale; BASC SRP: Self-Report of Personality of the Behavior Assessment System for Children; CIS: Columbia Impairment Scale; YQOL: Youth Quality of Life; CASA: Child and Adolescent Services Assessment; T-DSM-IV-S: Total DSM-IV-based Child and Adolescent Behavioral Dis¬orders Screening and Rating Scale; WICS-R: Wechsler Intelligence Scale for Children-Revised; AD: Anxiety disorder; SDQ: Strengths and Difficulties Questionnaire; ASRS: ADHD Adult Self Report Scale; STAI: State-Trait Anxiety Inventory; STAI-AD-SAI: State-Trait Anxiety Inventory for Adult–State-Anxiety scale; STAI-AD-TAI: State-Trait Anxiety Inventory for Adult–Trait-Anxiety scale.
Studies included parents, teachers and children as informants to establish diagnostic status.
Prevalence of comorbid anxiety and depression in ADHD
ADHD children and adolescents with age ranging from 6 to 18 years usually suffer from comorbid anxiety and/or depressive disorders. Anxiety in children with ADHD ranges from 10.5% to 27.6% while depression ranges from 3.8% to 17.8%. Comorbid anxiety and depression range from 14.8% to 29.6%. The prevalence of anxiety is higher in girls compared to boys (39.4% vs. 24.8%) [32-40]. Further, generalized anxiety disorder (GAD) prevalence was found to be statistically significantly higher in girls compared to boys with ADHD (12.1% in girls vs. 1.5% in boys, p=0.01).39 Results report that girls with ADHD were 3.66 times more likely to meet criteria for anxiety disorder than girls without ADHD. Moreover, girls reported higher prevalence of comorbid anxiety and depression than boys (44.3% vs. 14.8%) [33]. This indicates that the girls with ADHD have substantially higher risk of developing comorbid anxiety or depression. In addition to this the lower mean age of parents of the children with comorbid anxiety has also been found to be statistically significant compared to that of parents of children without anxiety [39] (Table 1) enlists prevalence of comorbid anxiety and depression in studies included.
Effect of comorbid anxiety and depression in behaviour, functioning and social-skills
Behavioral temperamental traits such as sensitive towards punishment assessed using behavioral inhibition system (BIS) and sensitive to rewards assessed using behavioral approach system (BAS) represent negative and positive emotions, which may be associated with anxiety and depression comorbidities in children having ADHD. It has been observed that adolescents who reported higher BIS scores reported severe anxiety and depression than those with lower BIS scores (p<0.001). However, significant association was not found between BAS and anxiety and depression. Further, more severe anxiety and depressive symptoms were reported by adolescents having ADHD and who were bullying victims (p<0.001). These in turn may impair an adolescent’s social skills and self-esteem, and increase the risk of being victimized by peers. On the other hand, more severe depressive symptoms were reported by adolescents who were bullying perpetrators than those who did not bully others (p<0.001). This suggests that the risk of depression requires close monitoring not only in adolescent bullying victims with ADHD but also in perpetrators with ADHD [35]. Studies have suggested that increasing levels of ADHD symptoms in childhood were associated with higher proportions of adolescents who displayed negative psychosocial outcomes like internalizing problems, poor peer relations and school problems, which in turn led to a risky drug and alcohol use and antisocial behavior [33] Such emotional and behavioral troubles in children and adolescents with ADHD accompanied by anxiety and depression comorbidities put a substantial burden on their social and family relationships and their overall functioning [34,38,41,42]. Results of few studies have reported that children with ADHD compared to those without ADHD had higher odds of activity restriction [OR(95%CI): 4.14 (3.34-5.15)], school problems [OR(95%CI): 5.18 (4.47- 6.01)], grade repetition [41,42] [OR(95%CI): 3.71 (3.02-4.55)] [41], poor parent-child communication [OR (95%CI): 2.55 (1.84-3.52)] [41] daily living [OR(95%CI): 19.818 (7.243-54.223)] and adaptive skills [OR(95%CI): 6.336 (2.979-13.470)] (38). Also, different comorbid emotional and behavioral indices, particularly depression and aggression were linked to greater levels of emotional lability (p<0.001) (38). Moreover, results suggests that total scores of Wechsler Intelligence Scale for Children-Revised (WISC-R) are lesser in children with anxiety disorder (AD) comorbidity versus those without AD. Also, total scores of DSM-IV-based Child and Adolescent Behavioral Disorders Screening and Rating Scale (T-DSM-IV-S) were found to be greater, though not statistically significant, in parents and teachers of cases with ADHD and AD comorbidity than those without AD comorbidity (39). This result shows that AD may have been developed in cases with severe symptoms of ADHD due to more difficulties faced in the social and academic life or the presence of AD as a comorbidity has worsened the ADHD condition [43,44]. Findings have also suggested that somatic complaints like headache, abdominal pain and neck pain are not more common among children having ADHD alone, but rather associated with those having both ADHD and depression/anxiety. Results report that such children were strongly associated with all somatic complaints but more specifically complained about neck and abdominal pain [21].
From a study accessing self-evaluation of comorbid conditions in school-aged children with and without ADHD, it was observed that children with ADHD self-reported significantly higher anxiety and depression symptoms than children without ADHD (p<0.001). Similarly, mothers of children having ADHD had a significantly higher State-Trait Anxiety Inventory for Adult– Trait-Anxiety scale (STAI-AD-TAI) score compared to mothers of children without ADHD (p<0.001). When the fathers and mothers in ADHD group were compared to the control group, it was found that mothers reported more severe anxiety and depressive symptoms than fathers. This indicates that there is significant correlation between depressive and anxiety symptoms of children with ADHD and corresponding symptoms in their parents [depressive symptoms (r:0.59, p=0.030); anxiety symptoms (r:0.59, p<0.001). Multivariate regression analysis using self-reported severity of anxiety and depressive symptoms in children with ADHD and their parents’ self-reported severity of these comorbidities have shown strong correlation (r>0.50) [32]. Further, it has been shown that youth with comorbid anxiety or depression disorders have poorer parent-reported social skills and lower social acceptance than youth without comorbid anxiety or depression. On the other hand, according to youth-reported scales, the youth with or without an anxiety or depressive disorder diagnosis did not differ on social skills (p=0.11) and social acceptance (p=0.58). After controlling for independent variables, the path analysis showed that having an anxiety disorder was not associated with any of the social functioning variables; but having depression was significantly associated with poorer parent - reported social skills (p=0.004) and social acceptance (p=0.02). All these results suggest that the connection between internalizing symptoms and social functioning in young adolescents with ADHD has a subtle distinction and it depends on the facets of anxiety and depression, as well as the domains of social adjustment which may be taken into consideration [34] (Table 2) enlists behavioral, functional and social skills’ findings from the studies included in this review.
Discussion
ADHD is one of the most frequently diagnosed disorders in children and adolescents and its correct diagnosis in the presence of comorbid conditions is often challenging. Anxiety which has the characteristics of fear and unrest causing substantial distress and loss of function is more prevalent in untreated ADHD children than control. Impaired information process in ADHD impairs adaptation to academic norms and thus causes anxiety [39] Depressed children often show more irritability and inattention than sadness, which may lead to a misdiagnosis of ADHD. Conditions, such as thyroid disease, drug abuse, sleep disorders, learning disabilities, bipolar disorder, or attachment disorders may easily be misdiagnosed as ADHD if not screened appropriately. In clinical practice, other than moderating factors such as age and gender, additional comorbid conditions add complexity to diagnosis, treatment and outcome of comorbid ADHD and depression [31]. Gender specific analysis reveals higher prevalence of comorbid anxiety and depression in girls than boys which may be due to the perception that girls with ADHD exhibit fewer behavior problems than boys. The pathways of risk for developing anxiety and/or depression among girls with ADHD may be due to individual and environmental factors that are independent of their ADHD, such as cognitive factors (e.g. perceived control), temperament (e.g. inhibition), and unique family factors (e.g., parental over protectiveness) [45-47].
Implications of comorbid anxiety and depression in ADHD
Comorbid anxiety and/or depression in children and adolescents with ADHD may lead to difficulty in regulating emotions-displaying higher rates of negative effect, greater emotional reactivity, and lower levels of empathy relative to normal controls [48-55]. This may be attributed to higher BIS scores which hinders the motivational aspect and leads to negative emotions. Nearly six fold increased risk for displaying significantly elevated levels of emotional lability, is observed. Further, children with depressive symptoms reported poorer self-reported social skills and youth-/parent-reported social acceptance. Children with ADHD and comorbid depression depicted lower scores on a latent construct measure of social competence (including parentreported social skills, self-reported popularity, and teacher-reported peer functioning) than non-depressed children with ADHD [34]. Further, effects of comorbidities on sleep with ADHD have found that GAD and SAD are associated with sleep-related involuntary movements reporting higher overall sleep disturbance scores than ADHD children without psychiatric comorbidities. Depressed children with ADHD report higher sleep onset latency as well as sleep duration, insomnia, hypersomnia, and fatigue leading to poor sleep quality [36]. In addition, parents who screened positive for ADHD reported relatively high rates of clinically significant anxiety or depressive symptoms which may be attributed to the age of the parents wherein young parents with inadequate life experience exhibited worried or an overprotective attitude due to their anxiety. Their feeling of desperation in turn facilitates development of anxiety in children with ADHD. Similarly, greater depressive symptoms have also been observed in mothers of children who had ADHD, indicating that current, environment-related state anxiety would also be higher [32].
Moreover, it has been observed that quality of life (QoL) is impaired in children and adolescents having ADHD. Individuals with comorbid ADHD and anxiety have worse working memory deficits (11) worse overall functioning [12] poorer psychosocial quality of life [13] and a lower response rate to stimulant treatment [14] than those with only ADHD. Further it has been observed that comorbid ADHD and depression results in greater levels of psychosocial impairment than those with only ADHD. Multiple anxiety comorbidities have been observed to be associated with poorer QoL, daily functioning as well as problematic behavior for children with ADHD. Poorer functioning in children with both ADHD-I and ADHDCombined (ADHD-C) was attributed to two or more anxiety comorbidities. Systematically assessing and treating anxiety in children with ADHD has the potential to improve functioning for these children [37].
Another implication of ADHD and comorbid disorders is health services utilization and treatment use. Findings suggest that the increase in number of comorbidities in children with ADHD causes a decline in functioning which results in increase in the use of health care services, educational services [41] and treatment services [38,41,42]. Children with ADHD have reported higher mental health service utilization use [41,42] (p<0.05) than children with any other mental health or neurodevelopmental disorder (41) or the unaffected children, [42] which results in a higher use of educational services in children with ADHD than those without ADHD (p<0.05). Lastly there was a significant association between socio-economic status of the parents of children with ADHD, comorbid anxiety/depression and low parental socio economic position with comorbid group being more strongly related (p<0.001) compared to the ADHD only group or depression/anxiety only group [21]. Since, children from low-income families typically have less access to health services, functioning declined more in children with lower income families than in children with affluent family background.
Limitation
Limitation of the present review is that only internalizing disorders such as anxiety and depression are considered for evaluation leaving externalizing disorders (oppositional defiant disorder and conduct disorder) as externalizing disorders are more disruptive in nature and clearly visible compared to internalizing disorder which in lieu of externalizing disorder goes unnoticed. Another limitation is that studies prior to 2008 are excluded keeping 10 years time-frame for reviewing. Further, adult ADHD is excluded from this analysis as the objective of the present review is to focus ADHD in children and adolescents and reviewing adult ADHD would go beyond the scope of present review. Lastly our findings are derived from cross-sectional studies, precluding casual inferences.
Conclusion
From the above findings it is clear that both genetic and social factors influence the occurrence, duration, and severity of anxiety and depressive symptoms in children and adolescents with ADHD. A critical feedback from parents about a child’s ADHD behaviors [56-63] poor adaptive skills and cognitive biases of parents learnt by children,58 disruptive behaviours, substance use and poor coping skills,59-61 strains family relationships, thereby increasing the risk of anxiety and depression and worsens ADHD symptoms. Considering that ADHD is a lifetime neurodevelopmental disorder and causes susceptibility to numerous mental disorders, early diagnosis, long-term monitoring, and proper treatment may help in reducing social anxiety and functional impairment in children and adolescent with comorbid anxiety and depression.
Key Messages
• Children having ADHD showed comparatively higher rates of comorbid anxiety and depressive disorders compared to control group [32].
• Girls with ADHD depicted higher internalizing problems compared to boys (44.3% vs. 14.8%) [33].
• Mothers of children who had ADHD self-reported significantly more severe trait anxiety symptoms and significantly more severe depressive symptoms than mothers of children without ADHD indicating the genetic correlation of ADHD [32].
• Depression is more evidently linked to poorer social functioning than anxiety among young adolescents with ADHD [34].
• Adolescents having ADHD reporting higher BIS score reported sever anxiety and depressive symptoms [35].
• ADHD children with anxiety showed higher overall sleep disturbance and children with depression showed higher sleep onset latency and sleep duration [36].
• With the increasing number of comorbidities (≥ 2), social and academic functioning decline in a step-wise fashion in children with ADHD leading to poorer QoL [37].
• Children with ADHD displayed high levels of emotional lability and functional impairment when present with comorbid depression and aggression [38].
Acknowledgements
The authors would like to acknowledge pharm EDGE for providing writing and editorial support while developing the manuscript.
Conflict of Interest
The authors do not have any conflict of interest to declare.
Source of Funding
Authors have not taken any financial support for this research and development of this manuscript.
Disclosure
The authors have nothing to disclose.
REFERENCES
- Costello EJ, Mustillo S, Erkanli A, et al. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837-44.
- Beidel DC, Turner SM, Morris TL. Psychopathology of childhood social phobia. J Am Acad Child Adolesc Psychiatry. 1999;38:643-50.
- Honjo S, Sasaki Y, Kaneko H, et al. School refusal and depression with school in attendance in children and adolescents: Comparative assessment between the children’s depression inventory and somatic complaints. Psychiatry Clin Neurosci. 2001;55:629-34.
- Uneri OS, Vatandas N, Atay G. Characteristics of ADHD first diagnosed during adolescence and compare the data with patients’ diagnosed at six-ten years of age. Anadolu Psikiyatri Derg. 2009;10:48-54.
- Thomas R, Sanders S, Doust J, et al. Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics. 2015;135:e994-1001.
- Danielson ML, Bitsko RH, Ghandour RM, et al. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents. J Clin Child Adolesc Psychol. 2018;47:199-212.
- Ford T, Goodman R, Meltzer H. The British child and adolescent mental health survey 1999: The prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry. 2003;42:1203-11.
- Gillberg C, Gillberg IC, Rasmussen P, et al. Co-existing disorders in ADHD-implications for diagnosis and intervention. Eur Child Adolesc Psychiatry. 2004;13:I80-92.
- Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: Implications for research, practice, and DSM-V. J Am Acad Child Adolesc Psychiatry. 1997;36:1065-79.
- Jarrett MA, Ollendick TH. A conceptual review of the comorbidity of attention-deficit/hyperactivity disorder and anxiety: Implications for future research and practice. Clin Psychol Rev. 2008;28:1266-80.
- Schatz DB, Rostain AL. ADHD with comorbid anxiety: A review of the current literature. J Atten Disord. 2006;10:141-49.
- March JS, Swanson JM, Arnold LE, et al. Anxiety as a predictor and outcome variable in the multimodal treatment study of children with ADHD (MTA). J Abnorm Child Psychol. 2000;28:527-41.
- Klassen AF, Miller A, Fine S. Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics. 2004;114:e541-47.
- Tannock R, Ickowicz A, Schachar R. Differential effects of methylphenidate on working memory in ADHD children with and without comorbid anxiety. J Am Acad Child Adolesc Psychiatry. 1995;34:886-96.
- Newcorn JH, Halperin JM, Jensen PS, et al. Symptom profiles in children with ADHD: effects of comorbidity and gender. J Am Acad Child Adolesc Psychiatry. 2001;40:137-46.
- Pliszka SR. Comorbidity of attention-deficit hyperactivity disorder and overanxious disorder. J Am Acad Child Adolesc Psychiatry. 1992;31:197-203.
- Bowen R, Chavira DA, Bailey K, et al. Nature of anxiety comorbid with attention deficit hyperactivity disorder in children from a pediatric primary care setting. Psychiatry Res. 2008;157:201-9.
- Barkley R. Behavioral inhibition, sustained attention, and executive func¬tion: constructing a unified theory of ADHD. Psychol Bull. 1997;121:65-94.
- Levy F. Synaptic gating and ADHD: A biological theory of comorbidity of ADHD and anxiety. Neurospychopharmacology. 2004;29:1589-96.
- Garralda ME. Somatisation in children. J Child Psychol Psychiatry. 1996;37:13-33.
- Leirbakk MJ, Clench-Aas J, Raanaas RK. ADHD with co-occurring depression/anxiety in children: The relationship with somatic complaints and parental socio-economic position. J Psychol Abnorm. Child 2015;4:137.
- Bird HR, Canino G, Rubio-Stipec M, et al. Estimates of prevalence of psychiatric maladjustment in a community survey in Puerto Rico. Arch Gen Psychiatry. 1988;45:1120-26.
- Anderson JC, Williams S, McGee R, et al. DSM-III disorders in preadolescent children: Prevalence in a large community sample. Arch Gen Psychiatry. 1998;44:69-76.
- Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry. 1991;148:564-77.
- Kessler RC, Adler LA, Barkley R, et al. Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: Results from the national comorbidity survey replication. Biol Psychiatry. 2005;57:1442-51.
- Med Scape. Depression and ADHD: What you need to know. 2018;2:1.
- Furman L. What is attention-deficit hyperactivity disorder (ADHD)?. J Child Neurol. 2005;20:994-1002.
- Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40:57-87.
- Luby JL, Heffelfinger AK, Mrakotsky C, et al. The clinical picture of depression in preschool children. J Am Acad Child Adolesc Psychiatry. 2003;42:340-48.
- Med Scape. ADHD in children with comorbid conditions: Diagnosis, misdiagnosis, and keeping tabs on both. 2018.
- Psychiatric Times. Comorbid depression and ADHD in children and adolescents. 2017.
- Xia W, Shen L, Zhang J, et al. Comorbid anxiety and depression in school-aged children with attention deficit hyperactivity disorder (ADHD) and self-reported symptoms of ADHD, anxiety, and depression among parents of school-aged children with and without ADHD. Shanghai Arch Psychiatry. 2015;27:356-67.
- Selinus EN, Molero Y, Lichtenstein P, et al. Subthreshold and threshold attention deficit hyperactivity disorder symptoms in childhood: Psychosocial outcomes in adolescence in boys and girls. Acta Psychiatr Scand. 2016;134:533-45.
- Becker SP, Langberg JM, Evans SW, et al. Differentiating anxiety and depression in relation to the social functioning of young adolescents with ADHD. J Clin Child Adolesc Psychol. 2015;44:1015-29.
- Hu HF, Chou WJ, Yen CF. Anxiety and depression among adolescents with attention-deficit/hyperactivity disorder: The roles of behavioral temperamental traits, comorbid autism spectrum disorder, and bullying involvement. Kaohsiung J Med Sci. 2016;32:103-9.
- Accardo JA, Marcus CL, Leonard MB, et al. Associations between psychiatric comorbidities and sleep disturbances in children with attention-deficit/hyperactivity disorder. J Dev Behav Pediatr. 2012;33:97-105.
- Sciberras E, Lycett K, Efron D, et al. Anxiety in children with attention-deficit/hyperactivity disorder. Pediatrics. 2014;133:801-8.
- Anastopoulos AD, Smith TF, Garrett ME, et al. Self-regulation of emotion, functional impairment, and comorbidity among children with AD/HD. J Atten Disord. 2011;15:583-92.
- Gumus YY, Cakin Memik N, Agaoglu B. Anxiety disorders comorbidity in children and adolescents with attention deficit hyperactivity disorder. Noro Psikiyatr Ars. 2015;52:185-93.
- Tung I, Li JJ, Meza JI, et al. Patterns of comorbidity among girls with ADHD: A meta-analysis. Pediatrics. 2016;138:e20160430.
- Larson K, Russ SA, Kahn RS, et al. Patterns of comorbidity, functioning, and service use for US children with ADHD, 2007. Pediatrics. 2011;127:462-70.
- Bussing R, Mason DM, Bell L, et al. Adolescent outcomes of childhood attention-deficit/hyperactivity disorder in a diverse community sample. J Am Acad Child Adolesc Psychiatry. 2010;49:595-605.
- Weiss M, Weiss G. Attention deficit hyperactivity disorder. In: Lewis M, (ed.) Child and adolescent psychiatry. A comprehensive textbook. (3rd ed.). Bal¬timore: LWW Books. 2002;pp:645-78.
- Waslick B, Greenhill L. Attention deficit hyperactivity disorder. In: Wiener J, Dulcan M (ed.) Text book of child and adolescent psychiatry. Washington DC: APA Books. 2004;pp:485-509.
- Chorpita BF, Brown TA, Barlow DH. Perceived control as a mediator of family environment in etiological models of childhood anxiety. Behav Ther. 1998;29:457-76.
- Degnan KA, Almas AN, Fox NA. Temperament and the environment in the etiology of childhood anxiety. J Child Psychol Psychiatry. 2010;51:497-517.
- Rapee RM, Schniering CA, Hudson JL. Anxiety disorders during childhood and adolescence: origins and treatment. Annu Rev Clin Psychol. 2009;5:311-41.
- Braaten EB, Rosén LA. Self-regulation of affect in attention deficit-hyperactivity disorder AD/HD and non-AD/HD boys: Differences in empathic responding. J Consult Clin Psychol. 2000;68:313-21.
- Cole PM, Zahn-Waxler C, Smith KD. Expressive control during a disappointment: Variations related to preschoolers’ behavior problems. Dev Psychol. 1994;30:835-46.
- Hinshaw SP, Melnick SM. Peer relationships in boys with attention-deficit hyperactivity disorder with and without comorbid aggression. Development and Psychopathology. 1995;7:627-47.
- Jensen SA, Rosén LA. Emotional reactivity in children with attention-deficit/hyperactivity disorder. J Atten Disord. 2004;8:53-61.
- Maedgen JW, Carlson CL. Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. J Clin Child Psychol. 2000;29:30-42.
- Martel MM. Research review: A new perspective on attention-deficit hyperactivity disorder: Emotion dysregulation and trait models. J Child Psychol Psychiatry. 2009;50:1042-51.
- Melnick SM, Hinshaw SP. Emotion regulation and parenting in AD/HD and comparison boys: linkages with social behaviors and peer preference. J Abnorm Child Psychol. 2000;28:73-86.
- Walcott CM, Landau S. The relation between disinhibition and emotion regulation in boys with attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol. 2004;33:772-82.
- Low SB, Stocker C. Family functioning and children’s adjustment: Associations among parent’s depressed mood, marital hostility, parent-child hostility and children’s adjustment. J Fam Psychol. 2005;19:394-403.
- Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90:12-17.
- Field AP. The behavioral inhibition system and the verbal information pathway to children’s fears. J Abnorm Psychol. 2006;115:742-52.
- Jerrell JM, McIntyre RS, Park YM. Risk factors for incident major depressive disorder in children and adolescents with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry. 2015;24:65-73.
- Meinzer MC, Lewinsohn PM, Pettit JW, et al. Attention deficit-hyperactivity disorder in adolescence predicts onset of major depressive disorder through early adulthood. Depress Anxiety. 2013;30:546-53.
- Mrug S, Molina BSG, Hoza B, et al. Peer rejection and friendships in children with attention-deficit/hyperactivity disorder: contributions to long-term outcomes. J Abnorm Child Psychol. 2012;40:1013-26.
- Mikami AY, Jack A, Eeh CC, et al. Parental influence on children with attention-deficit/hyperactivity disorder: I. relationships between parent behaviors and child peer status. J Abnorm Child Psychol. 2010;38:721-36.
- Mikami AY, Griggs MS, Lerner MD, et al. A randomized trial of a classroom intervention to increase peers' social inclusion of children with attention-deficit/hyperactivity disorder. J Consult Clin Psychol. 2013;81:100-112.