Bilateral absence of musculocutaneous nerve with unusual communicating branch between radial and ulnar nerves
Busra Candan, Kenan Ozturk and Soner Albay*
Suleyman Demirel University, Faculty of Medicine Department of Anatomy, Isparta, Turkey
- *Corresponding Author:
- Soner Albay, MD
Assoc. Prof. Suleyman Demirel University, Faculty of Medicine, Department of Anatomy Isparta 32260, Turkey
Tel: +90 246 2113680
E-mail: soneralbay@yahoo.com
Date of Received: December 14th, 2014
Date of Accepted: December 24th, 2016
Published Online: January 1st, 2017
© Int J Anat Var (IJAV). 2016; 9: 39–42.
[ft_below_content] =>Keywords
median nerve, musculocutaneous nerve, brachial plexus, absence, variations
Introduction
Median nerve (MN) and musculocutaneous nerve (MCN) are both terminal branches of the brachial plexus. Median nerve is formed by the union of lateral and medial roots from lateral and medial cord of brachial plexus. It then courses downwards in front of the arm; crosses the brachial artery from lateral to the medial side and finally enters the forearm by crossing the elbow joint. Usually MN does not give muscular branches in the arm, except one of the forearm muscles, pronator teres whose nerve arises from the MN before the nerve crosses the elbow [1]. MCN is a mixed peripheral nerve arising from the lateral cord of the brachial plexus in the axilla [2]. The MCN usually supplies the coracobrachialis, biceps brachii, and the brachialis muscles in the anterior compartment of the upper arm and then continues as the lateral cutaneous nerve of the forearm (LCNF) [3].
MCN has frequent variations and they were discussed in detail even in very early articles. It may be doubled, unusually short, or even absent [4]. Variations of the MCN may occur in 6.25% of cases and its absence has been reported with a prevalence ranging from 1.7 to 15% [5]. According to Tountas and Bergman [6], the MCN arises from the lateral cord (90.5%), from the lateral and posterior cord (4%), from the MN (2%), as two separate bundles from the medial and lateral cords (1.4%), or from the posterior cords (1.4%) [6].
Variations of the brachial plexus have significant clinical and surgical importance [7]. The frequencies and classifications of brachial plexus variations have been reported by other authors. It should be noted that the brachial plexus is the most variable part of the peripheral nervous system. The prevalence of all variations of brachial plexus ranges from 12.8 up to 53% [5]. The aim of the present study is to report the bilateral absence of MCN and the variant innervation of the flexor muscles of arm and the skin of lateral side of forearm from MN.
Case Report
During the educational year 2012-2013, within routine educational dissection in the Department of Anatomy in Suleyman Demirel University we observed a variation of the brachial plexus characterized by the absence of MCN on both sides in a 65-year-old male cadaver. There were no trauma or surgical intervention to his upper extremities. Brachial plexus and its terminal branches, axillary and brachial branches were exposed. We first determined that the MCN did not emerge from the lateral cord. The lateral cord completely continued as lateral root of MN and then it was noticed the MCN was absent in fact. The MCN was absent so the MN took charge of the MCN by giving both muscular and sensory branches. The MN was formed by the fusion of the lateral root coming as a continuation of the lateral cord, and the medial root from the medial cord, anterior to the axillary artery. The coracobrachialis muscle was innervated by a branch of lateral cord bilaterally. From median nerve, two branches emerged: one to biceps brachii muscle and the other to brachialis muscle which continued as LCNF bilaterally.
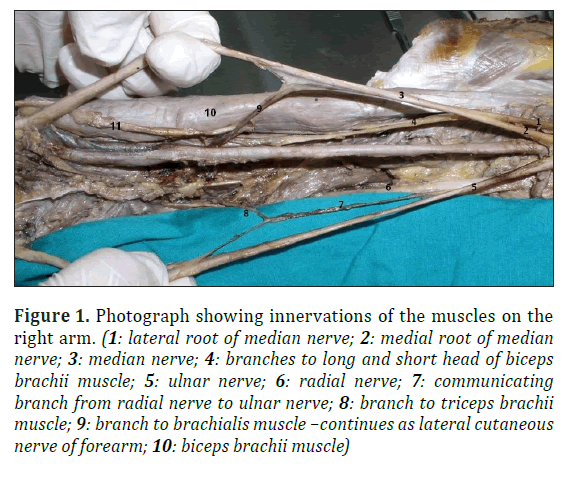
Right arm: Corocobrachialis muscle was innervated by a branch originated from the lateral cord just before formation of MN. MN innervated the biceps brachii muscle by a branch which further divided into two to supply long and short heads of the muscle individually (Figure 1). The latter branch of MN innervated the brachialis muscle in the middle part of the arm and then continued as LCNF. Medial cord divided to the medial root of MN and ulnar nerve. Posterior cord separated to radial nerve and axillary nerve. Additionally, a communicating branch was found from the radial nerve to the ulnar nerve in the arm. A branch emerging from this communicating branch innervated the triceps brachii muscle (Figure 1).
Figure 1: Photograph showing innervations of the muscles on the right arm. (1: lateral root of median nerve; 2: medial root of median nerve; 3: median nerve; 4: branches to long and short head of biceps brachii muscle; 5: ulnar nerve; 6: radial nerve; 7: communicating branch from radial nerve to ulnar nerve; 8: branch to triceps brachii muscle; 9: branch to brachialis muscle –continues as lateral cutaneous nerve of forearm; 10: biceps brachii muscle)
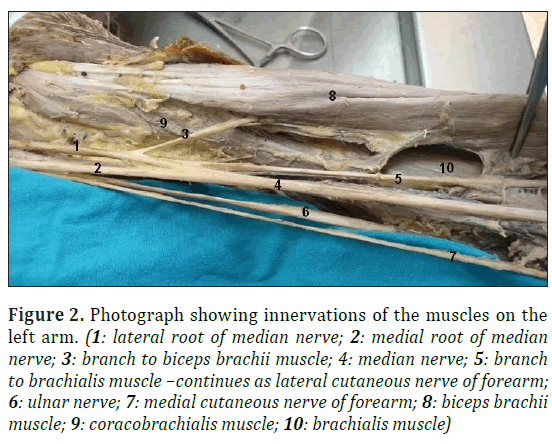
Left arm: Similar to right side, corocobrachialis muscle innervated by a branch from the lateral cord (which continued as lateral root of MN). MN innervated the biceps brachii muscle (Figure 2) by a branch which did not further divided to supply muscle heads individually, different from right side. Similar to right side, the other branch of MN innervated the brachialis muscle in the middle part of the arm and continued as LCNF. The medial cutaneous nerve of the forearm emerged from the medial cord. Medial cord divided to the medial root of MN and ulnar nerve. Posterior cord separated to radial and axillary nerves.
Figure 2: Photograph showing innervations of the muscles on the left arm. (1: lateral root of median nerve; 2: medial root of median nerve; 3: branch to biceps brachii muscle; 4: median nerve; 5: branch to brachialis muscle –continues as lateral cutaneous nerve of forearm; 6: ulnar nerve; 7: medial cutaneous nerve of forearm; 8: biceps brachii muscle; 9: coracobrachialis muscle; 10: brachialis muscle)
In conclusion, we observed that the MCN did not emerge from the lateral cord, actually it was absent on both sides. The MCN was absent so the MN took over the area of supply of the MCN by giving both the muscular and sensory branches. We cannot display all our observation as figures, because the materials used for student education and some structures were damaged.
Discussion
Variations in the branching pattern of brachial plexus may appear from unusual formation in the development of trunks, divisions and cords. Explanation of anatomical variations of brachial plexus relies on a proper understanding of its normal embryological development. Its development starts at 34th to 35th day of intrauterine life and definitive adult pattern is evident by 46th to 48th day of intrauterine life [7]. From the embryological studies done by Iwata (1960), the brachial plexus appears as a single radicular cone in the upper limb, which further divides into ventral and dorsal segments. The ventral segment gives roots to the median and the ulnar nerves. The MCN arises from the MN [3]. This study confirms the primitive embryological origin of the MCN from the MN.
The MCN innervates muscles of the anterior compartment of the arm and the lateral margin of the forearm. The MN does not have any muscular branches in the arm. If the MCN is absent, its fibers run in the MN and muscles of the anterior compartment of the arm are innervated by the MN [5]. Absence of the MCN does not lead to paralysis of the flexor musculature of the elbow or hypoesthesia of the lateral surface of the forearm, since the motor and sensory fibers arise from other nerves. The most common presentation is that its fibers originate from the MN or, less frequently, from the lateral root of the median nerve or from the lateral fasciculus of the brachial plexus [8].
According to Le Minor, the variations of the MCN and MN may be classified into five types [9]: Type I: There is no communication between the MCN and MN, fits to description in classic textbooks. The MCN pierces the coracobrachialis muscle and innervates the coracobrachialis, the biceps brachii and the brachialis muscles. Type II: Although some fibers of the medial root of the MN unite the lateral root of the MN and form the MN, other fibers run into the MCN and after some distance leaving it to join their proper trunk. Type III: The lateral root of the MN from the lateral cord runs into the MCN and after some distance leaving it to join their proper trunk. Type IV: The fibers of the MCN unite the lateral root of the MN; after some distance the MCN arise from the MN. Type V: The MCN is absent. The fibers supposed to form the MCN run into the MN along its course. The MCN does not pierce the coracobrachialis muscle in this type [9].
According to Le Minor, the variation of Type V was described by Broca in 1888 and its incidence ranged 0.3-2% [9]. Similar cases of absent MCN and unusual branches of the MN have been reported in literature [3,7]. Usually if the MCN is absent, the fibers of the MCN are enrouted through the lateral root of MN which takes the role of the MCN in supplying all the anterior arm muscles and lateral side of the skin of forearm [9]. In the present study, the MCN was absent bilaterally. Ihunwo et al. [10] also observed such a bilateral absence. Whereas Nakatani et al. [11] and Le Minor [9] observed its absence on the left side, and Prasada Rao and Chaudhary [3] observed it on the right side.
Ihunwo et al. reported a case of bilateral absence of the MCN from the lateral cord of the brachial plexus with four branches arising from the lateral side of the MN [10]. The first three were muscular branches to the coracobrachialis, biceps brachii, and brachialis muscles, and the last branch continued as the LCNF [10]. Our present case had complete absence of the MCN coinciding type V in Le Minor’s of classification [9]; the lateral cord completely continued as lateral root of MN. The MCN was absent. The coracobrachialis muscle was innervated by a branch of lateral cord bilaterally. From median nerve, two branches emerged: one to biceps brachii muscle and the other one to brachialis muscle which continued as LCNF bilaterally.
We also observed a rare communicating branch between ulnar and radial nerves at high humeral level. A branch originated from this communicating branch and innervated triceps brachii muscle. Ozguner et al. observed a unilateral connection between ulnar and radial nerves on the left arm of a 75-year-old male cadaver [12]. And also Arachchi et al. were demonstrated a communicating branch between ulnar and radial nerves on the right arm in a 85-year-old cadaver [13]. But these communicating branches did not innervated another muscle. Bergman et al. reported possible communication between radial and ulnar nerves in the arm [12]. However, prevalence for the communications between radial and ulnar nerves on the arm or forearm is missing in the literature. On the other hand, dorsal sensorial branch (60%) on the dorsal surface of the hand and radial nerve cutaneous innervations to the ulnar dorsum of the hand (16%) has been reported [12].
This is an anatomical variation that has clinical-surgical implications, considering that injury to the MN in this case might cause unexpected paralysis of the flexor musculature of the elbow and hypoesthesia of the lateral surface of the forearm. Variant nerve communications may cause ineffective nerve blocks and also sensory blockage of unexpected areas. During surgical procedure, such variations may lead to possible complications. Therefore, it is very important to know all variant communicating branches of brachial plexus for successful regional nerve blocks and operations. This case report is important to point out of possible anatomical variations during clinical practice.
Conclusion
Knowledge of anatomic variations of the MN and MCN is important in traumatology of the arm, as well as in plastic and reconstructive repair operations, and allows correct interpretation of clinical neurophysiology. Such cases may provide additional anatomical information to the clinicians for correct diagnosis of unusual clinical symptoms, and to surgeons to avoid damage to these nerves during surgical exploration of axilla and arm region.
Acknowledgments
All authors contributed equally to the paper.
References
- Bhanu PS, Sankar KD. Bilateral absence of musculocutaneous nerve with unusual branching pattern of lateral cord and median nerve of brachial plexus. Anat Cell Biol. 2012; 45(3): 207–210.
- Saeed M, Rufai AA. Median and musculocutaneous nerves: Variant formation and distribution. Clin Anat. 2003; 16(5): 453–457.
- Prasada Rao PV and Chaudhary SC. Absence of the musculocutaneous nerve. Two case reports. Clin Anat. 2001; 14(1): 31–35.
- Gumusburun E, Adiguzel E. A variation of the brachial plexus characterized by the absence of the musculocutaneus nerve: a case report. Surg Radiol Anat. 2000; 22(1): 63–65.
- Pacholczak R, Klimek-Piotrowska W, Walocha JA. Absence of the musculocutaneous nerve associated with a supernumerary head of biceps brachii: a case report. Surg Radiol Anat. 2011; 33(6): 551–554.
- Tountas C, Bergman R. Anatomic variations of the upper extremity. Churchill Livingstone, New York. 1993; 223–224.
- Chaware PN, Ughade JM, Pandit SV, Maske GL. Variant branches of brachial plexus - a case report. Int J Anat Var. 2012; 5: 5–7.
- Fregnani JH, Macea MI, Pereira CS, Barros MD, Macea JR. Absence of the musculocutaneous nerve: a rare anatomical variation with possible clinical-surgical implications. Sao Paulo Med J. 2008; 126(5): 288–290.
- Le Minor JM. A rare variant of the median and musculocutaneous nerves in Man. Arch Anat Histol Embryol. 1992; 73: 33–42.
- Ihunwo AO, Osinde SP, Mukhtar AU. Distribution of median nerve to muscles of the anterior compartment of the arm. Cent Afr J Med. 1997; 43(12): 359–360.
- Nakatani T, Tanaka S, Mizukami S. Absence of the musculocutaneous nerve with innervation of coracobrachialis, biceps brachii, brachialis and the lateral border of the forearm by branches from the lateral cord of the brachial plexus. J Anat. 1997; 191(3): 459–460.
- Oguner G, Desdicioglu K, Albay S. Connection between radial and ulnar nerves at high humeral level extremity. Int J Anat Var. 2010; 3: 49–50.
- Arachchi A, Loo ZY, Maung H, Vasudevan A. A rare anatomical variation between the radial and ulnar nerves in the arm. Int J Anat Var. 2013; 6: 131–132.
Busra Candan, Kenan Ozturk and Soner Albay*
Suleyman Demirel University, Faculty of Medicine Department of Anatomy, Isparta, Turkey
- *Corresponding Author:
- Soner Albay, MD
Assoc. Prof. Suleyman Demirel University, Faculty of Medicine, Department of Anatomy Isparta 32260, Turkey
Tel: +90 246 2113680
E-mail: soneralbay@yahoo.com
Date of Received: December 14th, 2014
Date of Accepted: December 24th, 2016
Published Online: January 1st, 2017
© Int J Anat Var (IJAV). 2016; 9: 39–42.
Abstract
Variations in the course and branches of the musculocutaneous nerve and the absence of the nerve have been reported in the literature. During the routine dissection of a 65-year-old male cadaver, we observed a variant brachial plexus characterized by the absence of the musculocutaneous nerve bilaterally. The median nerve took over the area of supply of the musculocutaneous nerve by giving both the muscular and sensory branches. The coracobrachialis muscle was innervated by a branch of lateral cord bilaterally. From median nerve, two branches emerged: one to biceps brachii muscle and the other one to brachialis muscle, which continued as lateral cutaneous nerve of forearm. We also observed a communicating branch between ulnar and radial nerves at high humeral level at right side. A branch emerged from this communicating branch and innervated triceps brachii muscle. These variations have clinical significance during surgical procedures in brachial plexus block, diagnostic clinical neurophysiology.
-Keywords
median nerve, musculocutaneous nerve, brachial plexus, absence, variations
Introduction
Median nerve (MN) and musculocutaneous nerve (MCN) are both terminal branches of the brachial plexus. Median nerve is formed by the union of lateral and medial roots from lateral and medial cord of brachial plexus. It then courses downwards in front of the arm; crosses the brachial artery from lateral to the medial side and finally enters the forearm by crossing the elbow joint. Usually MN does not give muscular branches in the arm, except one of the forearm muscles, pronator teres whose nerve arises from the MN before the nerve crosses the elbow [1]. MCN is a mixed peripheral nerve arising from the lateral cord of the brachial plexus in the axilla [2]. The MCN usually supplies the coracobrachialis, biceps brachii, and the brachialis muscles in the anterior compartment of the upper arm and then continues as the lateral cutaneous nerve of the forearm (LCNF) [3].
MCN has frequent variations and they were discussed in detail even in very early articles. It may be doubled, unusually short, or even absent [4]. Variations of the MCN may occur in 6.25% of cases and its absence has been reported with a prevalence ranging from 1.7 to 15% [5]. According to Tountas and Bergman [6], the MCN arises from the lateral cord (90.5%), from the lateral and posterior cord (4%), from the MN (2%), as two separate bundles from the medial and lateral cords (1.4%), or from the posterior cords (1.4%) [6].
Variations of the brachial plexus have significant clinical and surgical importance [7]. The frequencies and classifications of brachial plexus variations have been reported by other authors. It should be noted that the brachial plexus is the most variable part of the peripheral nervous system. The prevalence of all variations of brachial plexus ranges from 12.8 up to 53% [5]. The aim of the present study is to report the bilateral absence of MCN and the variant innervation of the flexor muscles of arm and the skin of lateral side of forearm from MN.
Case Report
During the educational year 2012-2013, within routine educational dissection in the Department of Anatomy in Suleyman Demirel University we observed a variation of the brachial plexus characterized by the absence of MCN on both sides in a 65-year-old male cadaver. There were no trauma or surgical intervention to his upper extremities. Brachial plexus and its terminal branches, axillary and brachial branches were exposed. We first determined that the MCN did not emerge from the lateral cord. The lateral cord completely continued as lateral root of MN and then it was noticed the MCN was absent in fact. The MCN was absent so the MN took charge of the MCN by giving both muscular and sensory branches. The MN was formed by the fusion of the lateral root coming as a continuation of the lateral cord, and the medial root from the medial cord, anterior to the axillary artery. The coracobrachialis muscle was innervated by a branch of lateral cord bilaterally. From median nerve, two branches emerged: one to biceps brachii muscle and the other to brachialis muscle which continued as LCNF bilaterally.
Right arm: Corocobrachialis muscle was innervated by a branch originated from the lateral cord just before formation of MN. MN innervated the biceps brachii muscle by a branch which further divided into two to supply long and short heads of the muscle individually (Figure 1). The latter branch of MN innervated the brachialis muscle in the middle part of the arm and then continued as LCNF. Medial cord divided to the medial root of MN and ulnar nerve. Posterior cord separated to radial nerve and axillary nerve. Additionally, a communicating branch was found from the radial nerve to the ulnar nerve in the arm. A branch emerging from this communicating branch innervated the triceps brachii muscle (Figure 1).
Figure 1: Photograph showing innervations of the muscles on the right arm. (1: lateral root of median nerve; 2: medial root of median nerve; 3: median nerve; 4: branches to long and short head of biceps brachii muscle; 5: ulnar nerve; 6: radial nerve; 7: communicating branch from radial nerve to ulnar nerve; 8: branch to triceps brachii muscle; 9: branch to brachialis muscle –continues as lateral cutaneous nerve of forearm; 10: biceps brachii muscle)
Left arm: Similar to right side, corocobrachialis muscle innervated by a branch from the lateral cord (which continued as lateral root of MN). MN innervated the biceps brachii muscle (Figure 2) by a branch which did not further divided to supply muscle heads individually, different from right side. Similar to right side, the other branch of MN innervated the brachialis muscle in the middle part of the arm and continued as LCNF. The medial cutaneous nerve of the forearm emerged from the medial cord. Medial cord divided to the medial root of MN and ulnar nerve. Posterior cord separated to radial and axillary nerves.
Figure 2: Photograph showing innervations of the muscles on the left arm. (1: lateral root of median nerve; 2: medial root of median nerve; 3: branch to biceps brachii muscle; 4: median nerve; 5: branch to brachialis muscle –continues as lateral cutaneous nerve of forearm; 6: ulnar nerve; 7: medial cutaneous nerve of forearm; 8: biceps brachii muscle; 9: coracobrachialis muscle; 10: brachialis muscle)
In conclusion, we observed that the MCN did not emerge from the lateral cord, actually it was absent on both sides. The MCN was absent so the MN took over the area of supply of the MCN by giving both the muscular and sensory branches. We cannot display all our observation as figures, because the materials used for student education and some structures were damaged.
Discussion
Variations in the branching pattern of brachial plexus may appear from unusual formation in the development of trunks, divisions and cords. Explanation of anatomical variations of brachial plexus relies on a proper understanding of its normal embryological development. Its development starts at 34th to 35th day of intrauterine life and definitive adult pattern is evident by 46th to 48th day of intrauterine life [7]. From the embryological studies done by Iwata (1960), the brachial plexus appears as a single radicular cone in the upper limb, which further divides into ventral and dorsal segments. The ventral segment gives roots to the median and the ulnar nerves. The MCN arises from the MN [3]. This study confirms the primitive embryological origin of the MCN from the MN.
The MCN innervates muscles of the anterior compartment of the arm and the lateral margin of the forearm. The MN does not have any muscular branches in the arm. If the MCN is absent, its fibers run in the MN and muscles of the anterior compartment of the arm are innervated by the MN [5]. Absence of the MCN does not lead to paralysis of the flexor musculature of the elbow or hypoesthesia of the lateral surface of the forearm, since the motor and sensory fibers arise from other nerves. The most common presentation is that its fibers originate from the MN or, less frequently, from the lateral root of the median nerve or from the lateral fasciculus of the brachial plexus [8].
According to Le Minor, the variations of the MCN and MN may be classified into five types [9]: Type I: There is no communication between the MCN and MN, fits to description in classic textbooks. The MCN pierces the coracobrachialis muscle and innervates the coracobrachialis, the biceps brachii and the brachialis muscles. Type II: Although some fibers of the medial root of the MN unite the lateral root of the MN and form the MN, other fibers run into the MCN and after some distance leaving it to join their proper trunk. Type III: The lateral root of the MN from the lateral cord runs into the MCN and after some distance leaving it to join their proper trunk. Type IV: The fibers of the MCN unite the lateral root of the MN; after some distance the MCN arise from the MN. Type V: The MCN is absent. The fibers supposed to form the MCN run into the MN along its course. The MCN does not pierce the coracobrachialis muscle in this type [9].
According to Le Minor, the variation of Type V was described by Broca in 1888 and its incidence ranged 0.3-2% [9]. Similar cases of absent MCN and unusual branches of the MN have been reported in literature [3,7]. Usually if the MCN is absent, the fibers of the MCN are enrouted through the lateral root of MN which takes the role of the MCN in supplying all the anterior arm muscles and lateral side of the skin of forearm [9]. In the present study, the MCN was absent bilaterally. Ihunwo et al. [10] also observed such a bilateral absence. Whereas Nakatani et al. [11] and Le Minor [9] observed its absence on the left side, and Prasada Rao and Chaudhary [3] observed it on the right side.
Ihunwo et al. reported a case of bilateral absence of the MCN from the lateral cord of the brachial plexus with four branches arising from the lateral side of the MN [10]. The first three were muscular branches to the coracobrachialis, biceps brachii, and brachialis muscles, and the last branch continued as the LCNF [10]. Our present case had complete absence of the MCN coinciding type V in Le Minor’s of classification [9]; the lateral cord completely continued as lateral root of MN. The MCN was absent. The coracobrachialis muscle was innervated by a branch of lateral cord bilaterally. From median nerve, two branches emerged: one to biceps brachii muscle and the other one to brachialis muscle which continued as LCNF bilaterally.
We also observed a rare communicating branch between ulnar and radial nerves at high humeral level. A branch originated from this communicating branch and innervated triceps brachii muscle. Ozguner et al. observed a unilateral connection between ulnar and radial nerves on the left arm of a 75-year-old male cadaver [12]. And also Arachchi et al. were demonstrated a communicating branch between ulnar and radial nerves on the right arm in a 85-year-old cadaver [13]. But these communicating branches did not innervated another muscle. Bergman et al. reported possible communication between radial and ulnar nerves in the arm [12]. However, prevalence for the communications between radial and ulnar nerves on the arm or forearm is missing in the literature. On the other hand, dorsal sensorial branch (60%) on the dorsal surface of the hand and radial nerve cutaneous innervations to the ulnar dorsum of the hand (16%) has been reported [12].
This is an anatomical variation that has clinical-surgical implications, considering that injury to the MN in this case might cause unexpected paralysis of the flexor musculature of the elbow and hypoesthesia of the lateral surface of the forearm. Variant nerve communications may cause ineffective nerve blocks and also sensory blockage of unexpected areas. During surgical procedure, such variations may lead to possible complications. Therefore, it is very important to know all variant communicating branches of brachial plexus for successful regional nerve blocks and operations. This case report is important to point out of possible anatomical variations during clinical practice.
Conclusion
Knowledge of anatomic variations of the MN and MCN is important in traumatology of the arm, as well as in plastic and reconstructive repair operations, and allows correct interpretation of clinical neurophysiology. Such cases may provide additional anatomical information to the clinicians for correct diagnosis of unusual clinical symptoms, and to surgeons to avoid damage to these nerves during surgical exploration of axilla and arm region.
Acknowledgments
All authors contributed equally to the paper.
References
- Bhanu PS, Sankar KD. Bilateral absence of musculocutaneous nerve with unusual branching pattern of lateral cord and median nerve of brachial plexus. Anat Cell Biol. 2012; 45(3): 207–210.
- Saeed M, Rufai AA. Median and musculocutaneous nerves: Variant formation and distribution. Clin Anat. 2003; 16(5): 453–457.
- Prasada Rao PV and Chaudhary SC. Absence of the musculocutaneous nerve. Two case reports. Clin Anat. 2001; 14(1): 31–35.
- Gumusburun E, Adiguzel E. A variation of the brachial plexus characterized by the absence of the musculocutaneus nerve: a case report. Surg Radiol Anat. 2000; 22(1): 63–65.
- Pacholczak R, Klimek-Piotrowska W, Walocha JA. Absence of the musculocutaneous nerve associated with a supernumerary head of biceps brachii: a case report. Surg Radiol Anat. 2011; 33(6): 551–554.
- Tountas C, Bergman R. Anatomic variations of the upper extremity. Churchill Livingstone, New York. 1993; 223–224.
- Chaware PN, Ughade JM, Pandit SV, Maske GL. Variant branches of brachial plexus - a case report. Int J Anat Var. 2012; 5: 5–7.
- Fregnani JH, Macea MI, Pereira CS, Barros MD, Macea JR. Absence of the musculocutaneous nerve: a rare anatomical variation with possible clinical-surgical implications. Sao Paulo Med J. 2008; 126(5): 288–290.
- Le Minor JM. A rare variant of the median and musculocutaneous nerves in Man. Arch Anat Histol Embryol. 1992; 73: 33–42.
- Ihunwo AO, Osinde SP, Mukhtar AU. Distribution of median nerve to muscles of the anterior compartment of the arm. Cent Afr J Med. 1997; 43(12): 359–360.
- Nakatani T, Tanaka S, Mizukami S. Absence of the musculocutaneous nerve with innervation of coracobrachialis, biceps brachii, brachialis and the lateral border of the forearm by branches from the lateral cord of the brachial plexus. J Anat. 1997; 191(3): 459–460.
- Oguner G, Desdicioglu K, Albay S. Connection between radial and ulnar nerves at high humeral level extremity. Int J Anat Var. 2010; 3: 49–50.
- Arachchi A, Loo ZY, Maung H, Vasudevan A. A rare anatomical variation between the radial and ulnar nerves in the arm. Int J Anat Var. 2013; 6: 131–132.