Bilateral bitruncular venous malformation of the thigh: Case report
2 Department of Anatomy, School of Medicine, Mersin University, Mersin, Turkey, Email: turann_koc@yahoo.com
Received: 26-Feb-2018 Accepted Date: Mar 19, 2018; Published: 03-Apr-2018, DOI: 10.37532/1308-4038.18.11.37
Citation: Fahrioglu SL, Koç T, Kurtoglu Z, et al. Bilateral bitruncular venous malformation of the thigh: Case report. Int J Anat Var. 2018;11(2):37-39.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Summary
We present a case with bitruncular venous malformations of popliteal and femoral veins, bilaterally and we observed more than one connection which were described as femoral and popliteal connections in the gluteal region and lower extremity dissection of the formalin-fixed, 64-year-old male cadaver. On both sides, the small saphenous vein, anterior tibial, lateral genicular and one of the posterior tibial (PTV) veins drained into the lateral root of the popliteal vein. However, the other PTV and medial genicular vein drained into the medial root of the popliteal vein. In the left anterior thigh region, we observed three femoral connections between the lateral and medial roots of the femoral vein while two connections were observed among them on the right side. Additionally, we encountered unusual connections which were described ‘Z’ & ‘M’ shaped between perforant branches of the deep femoral vein and inferior gluteal vein. Having knowledge about the deep vein variations in the lower limb will guide the radiological, surgical and clinical evaluation of the patients with deep vein thrombosis.
Keywords
Popliteal vein; Femoral vein; Sciatic nerve; Vascular malformation; Deep vein thrombosis
Introduction
Primitive vascular channels are formed during the third week of the intrauterine period. According to Uhl et al. [1] three developmental stages of vascular formation are classified as undifferentiated (the first stage), retiform (the second stage), and maturation (the third stage) stages. During the first two stages, capillary networks and large plexiform structures are formed. At the last stage, larger channels are formed and maturations of the arteries, veins and lymphatics are shaped into their final forms [1,2] by biochemical factors (vascular endothelial growth factor & epinephrine family) [3-5].
The venous development of the lower limb in the embryonic period is determined by the femoral nerve (FN), greater sciatic nerve (SN) and small sciatic nerve (SSN) which are called the angioguiding nerves. The axial venous plexus is formed by the axial nerve or greater sciatic nerve, preaxial venous plexus is formed by the preaxial or femoral nerve and post-axial venous plexus formed by the SSN or sural nerve. The femoral vein (FV) and the great saphenous vein (GSV) are derived from preaxial venous plexus while the small saphenous vein (SSV) is developed from postaxial venous plexus [1]. The main venous drainage system of the lower limb takes its final shape as a result of the venous channels that disappeared and their anastomoses. The venous anatomy is not as stable as the anatomy of the arteries and especially the venous anatomy of the lower limbs shows highly variative formation [1,6,7]. It has been described in the literature that the number of femoral trunks and various anatomic variations in their venous diameter at the thigh level may have clinical importance in case of a disease such as deep vein thrombosis (DVT) [8-11].
In this report, morphometrical features of a case with duplicated femoral and popliteal veins were used to evaluate their impact on developmental and clinical aspects.
Case Report
The present case, displaying bilaterally duplicated femoral and popliteal veins, accompanied with high division of SN and connection between inferior gluteal vein (IGV) and 2nd perforant branch of the deep femoral vein (DFV) was encountered during a routine gluteal region and lower extremity dissection (10% formalin-fixed, 64-year-old male cadaver) in the Human Anatomy Department at the Near East University.
In the popliteal fossa, we encountered bitruncular venous malformations of popliteal and femoral veins (as lateral and medial roots), bilaterally. We observed more than one connection which were described as femoral (FC) and popliteal (PC) connections.
The evaluation of the popliteal venous networks/connections on both sides
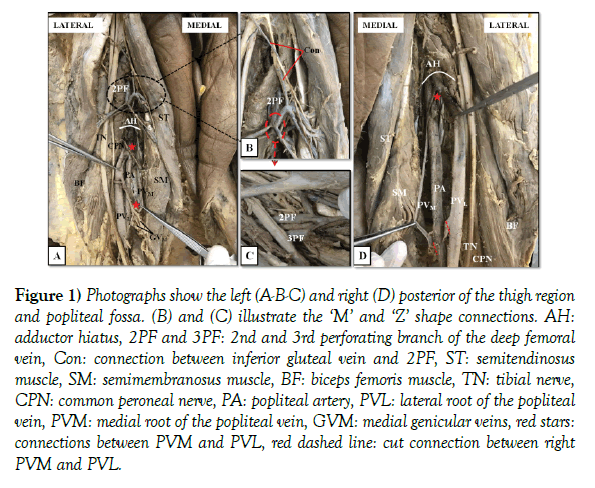
On both sides, small saphenous vein (SSV), anterior tibial (ATV), lateral genicular (GVL) and one of the posterior tibial veins (PTV) drained into the lateral root of the popliteal vein (PVL). However, the other PTV and medial genicular vein (GVM) drained into the PVM (Figure 1). The PVL (9 mm in diameter) was ascending anterolateral to the popliteal artery (PA) while PVM (4 mm in diameter) was posteromedial to the PA, bilaterally (Figure 1). On the both sides, we encountered two connections between PVL and PVM before they reached the adductor hiatus (AH). These two connections were crossed the PA anteriorly. On the left side, these connection lengths were 14 mm and 36 mm while they were 24 mm and 36 mm on the right side.
Figure 1) Photographs show the left (A-B-C) and right (D) posterior of the thigh region and popliteal fossa. (B) and (C) illustrate the ‘M’ and ‘Z’ shape connections. AH: adductor hiatus, 2PF and 3PF: 2nd and 3rd perforating branch of the deep femoral vein, Con: connection between inferior gluteal vein and 2PF, ST: semitendinosus muscle, SM: semimembranosus muscle, BF: biceps femoris muscle, TN: tibial nerve, CPN: common peroneal nerve, PA: popliteal artery, PVL: lateral root of the popliteal vein, PVM: medial root of the popliteal vein, GVM: medial genicular veins, red stars: connections between PVM and PVL, red dashed line: cut connection between right PVM and PVL.
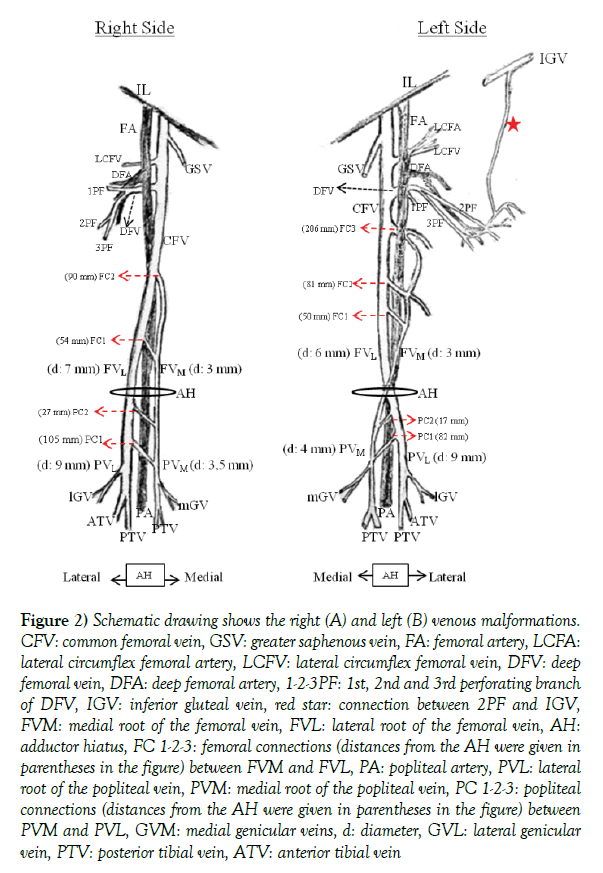
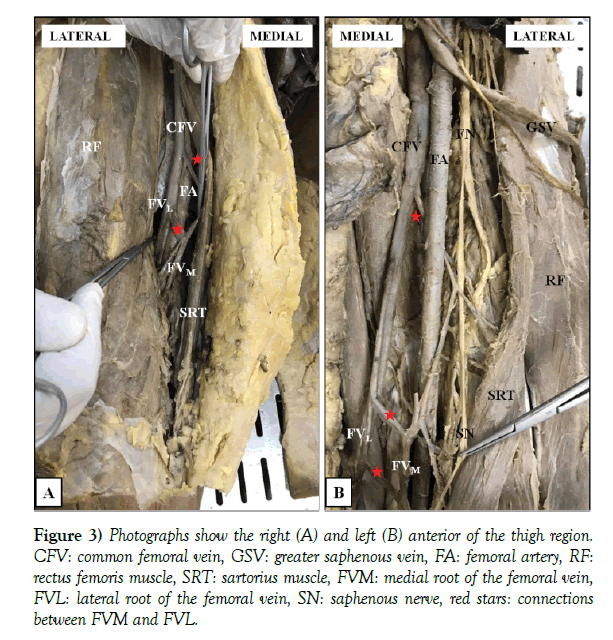
In addition, these two roots passed through the adductor hiatus (AH) and continued as lateral root of the femoral (FVL) and medial root of the femoral vein (FVM) on both sides (Figures 2 and 3).
Figure 2) Schematic drawing shows the right (A) and left (B) venous malformations. CFV: common femoral vein, GSV: greater saphenous vein, FA: femoral artery, LCFA: lateral circumflex femoral artery, LCFV: lateral circumflex femoral vein, DFV: deep femoral vein, DFA: deep femoral artery, 1-2-3PF: 1st, 2nd and 3rd perforating branch of DFV, IGV: inferior gluteal vein, red star: connection between 2PF and IGV, FVM: medial root of the femoral vein, FVL: lateral root of the femoral vein, AH: adductor hiatus, FC 1-2-3: femoral connections (distances from the AH were given in parentheses in the figure) between FVM and FVL, PA: popliteal artery, PVL: lateral root of the popliteal vein, PVM: medial root of the popliteal vein, PC 1-2-3: popliteal connections (distances from the AH were given in parentheses in the figure) between PVM and PVL, GVM: medial genicular veins, d: diameter, GVL: lateral genicular vein, PTV: posterior tibial vein, ATV: anterior tibial vein
Figure 3) Photographs show the right (A) and left (B) anterior of the thigh region. CFV: common femoral vein, GSV: greater saphenous vein, FA: femoral artery, RF: rectus femoris muscle, SRT: sartorius muscle, FVM: medial root of the femoral vein, FVL: lateral root of the femoral vein, SN: saphenous nerve, red stars: connections between FVM and FVL.
The evaluation of the femoral venous networks/connections on both sides:
In the left anterior thigh region, we observed three femoral connections between the FVL and the FVM while two connections were observed on the right side (Figures 2 and 3). On the right side, the FVM (3 mm in diameter) and connections coursed anterior to FA. The last connections point the FVM drained into FVL (7 mm in diameter) and it continued as common femoral vein (CFV). However, on the left anterior thigh region, the FVM (3 mm in diameter) and connections coursed anterior to the PA and FVM drained into the FVL (6 mm in diameter) posterior to FA (Figures 2 and 3). Additionally, medial femoral circumflex vein (MCV) and greater saphenous vein (GSV), deep femoral vein (DFV) also drained into CFV (48 mm, 62 mm and 78 mm above the formation point of CFV, respectively).
‘’M’’ and ‘’Z’’ shapes venous networks on the left posterior thigh region
During the posterior dissection of the left thigh region, the perforating branches of the DFV were observed to be closer to the surface than normal and very close to tibial and common peroneal nerves. We encountered connections between 2nd (2PF) and 3th PF (3PF) and IGV and 2nd PF of DFV. Before the perforation of the adductor muscle fibers, the diameters of the 2PF and 3PF were measured as 3.5 mm and 4.8 mm, respectively. A connection was detected between 2PF and 3PF and appeared like the letter “Z” (Figures 1 and 2). At this point, 2PF appeared like the letter “M”. A branch (diameter 2 mm) separated from the IGV suspends the “M” shape of the 2PF (Figures 1 and 2A, 2B). On the left side, the sciatic nerve (SN) had a high division and divided into its terminal branches (TB) in the pelvic region, however, on the right side, TB were separated in the gluteal region. There was no connection between the VGI and DFV on the right side.
Discussion
The main cause of venous variation in the lower limbs is congenital venous malformations occurring during the late developmental stage of the embryo, which is the most important period for venous malformations [1,6,7].
Various venous malformations of the femoral vein can be observed from agenesis to multiplication. Uhl et al. [1] reported that 88% of the femoral veins had modal anatomy while 12% of them had truncular malformation. In addition, these malformations were divided in two main classes as unitruncular or bitruncular types (mainly based on the number of channels that carry the blood from distal to the proximal). These two configurations have various formations [1,6,7,12]. The present case both PV and FV had two separated roots which are called medial and lateral roots of the regarding veins. Therefore, the present case was in concordance with the sub-group of bitruncular configuration (bifidity of femoral vein) [1]. Koç et al. [6] described the draination patterns of the SSV, PTV, ATV, GVM and GVL in the presence of the persistent sciatic vein (PSV) case; SSV, PTV and one of ATV drained into the PSV while the other ATV and all genicular veins drained into the popliteal vein on the both sides. We observed that the presence of the PVL and PVM, the drainage patterns of the SSV, PTV, ATV, GVM and GVL were difference from the regular anatomy.
The prevalence of anatomical variations in the veins of the lower limb was assessed with venographic studies by Gordon et al. [10] as 25%, by Quinlan et al. [11] as 32%, and by Screaton et al. [13] as 46%. Agenesis was observed at 0.3% in the Parks et al. (14) study. Multiple FV was reported as 6%-38% and the variations that presented as duplicated femoral veins was 12% to 46% in the literature including venographic ultrasonographic and cadaveric studies [1,14].
Lower extremity DVT is a disease that can sometimes be seen in healthy individuals with patients in the postoperative period [15]. Maki et al. [15] reported that 77.7% of thrombi of the lower limb was observed either the CFV or PV or both of them while 22.3% of thrombi was observed in superficial FV. According to the results of another study, 99% of patients had widespread femoral venous or popliteal venous acute deep venous thrombosis, only 1% had superficial femoral vascular acute DVT [16]. DVT is also a systemic side effect of sclerotherapy, also known as a safe method for the treatment of superficial venous insufficiency. If any of these patients have an unknown variation of the femoral and popliteal vein, there could be an increased risk for DVT. Additionally, the risk of DVT, which develops as a complication of sclerotherapy, may change in cases with variations in the FV and PV. In the literature, there is not enough information about drainage patterns of the SSV on duplicated PV cases. Therefore, in patients who go through sclerotherapy, the question of whether more or less complications may arise in the presence of duplicated PV and FV should be investigated.
It has been reported that variations of the lower limb veins are particularly important for DVT, as the risk of thrombus formation in one channel of different diameter and duplicated variant veins is more than the risk of thrombus formation in normal anatomic vessels [9]. It may be explained by decreasing flow velocity because of duplicated and different in diameter veins [9]. The M and Z shaped vein formations and femoral/popliteal connections in our case should be considered as variant structures that can influence flow velocity.
In the light of the findings, duplicated popliteal and femoral veins and connections between duplicated veins itself should be considered in the interpretation of radiological images and assessment of sclerotherapy complications for deep vein thrombosis, and sciatic nerve blockage applications.
REFERENCES
- Uhl JF, Gillot C, Chahim M. Anatomical variations of the femoral vein. J Vasc Surg. 2010;52:714-9.
- Belov S. Anatomopathological classification of congenital vascular defects. Semin Vasc Surg. 1993;6:219-24.
- le Noble F, Moyon D, Pardanaud L, et al. Flow regulates arterial-venous differentiation in the chick embryo yolk sac. Development. 2004;131:361-75.
- Mukouyama YS, Shin D, Britsch S, et al. Sensory nerves determine the pattern of arterial differentiation and blood vessel branching in the skin. Cell. 2002; 109:693-705.
- Wang HU, Chen ZF, Anderson DJ. Molecular distinction and angiogenic interaction between embryonic arteries and veins revealed by ephrin-B2 and its receptor Eph-B4. Cell. 1998;93:741-53.
- Koç T, Gilan IY, Kulekçi GD, et al. Bilateral persistent sciatic vein: report of a case with developmental, histological and clinical aspects. Surg Radiol Anat. 2014; 36:189-94.
- Cherry KJ, Gloviczki P, Stanson AW. Persistent sciatic vein: diagnosis and treatment of a rare condition. J Vasc Surg. 1996;23:490-7.
- Cockett FB. Abnormalities of the deep veins of the leg. Postgrad Med J. 1954;30:512-22.
- Dona E, Fletcher JP, Hughes TM, et al. Duplicated popliteal and superficial femoral veins: incidence and potential significance. Aust N Z J Surg. 2000;70:438-40.
- Gordon AC, Wright I, Pugh ND. Duplication of the superficial femoral vein: recognition with duplex ultrasonography. Clin Radiol. 1996;51:622-4.
- Quinlan DJ, Alikhan R, Gishen P, et al. Variations in lower limb venous anatomy: implications for US diagnosis of deep vein thrombosis. Radiology. 2003;228:443-8.
- Natsis K, Totlis T, Paraskevas G, et al. Axial transformation of the profunda femoris vein: formation, relations and course in a cadaveric specimen. Folia Morphol. 2008;67:304-6.
- Screaton NJ, Gillard JH, Berman LH, et al. Duplicated superficial femoral veins: a source of error in the sonographic investigation of deep vein thrombosis. Radiology. 1998;206:397-401.
- Park EA, Chung JW, Lee W, et al. Three-dimensional evaluation of the anatomic variations of the femoral vein and popliteal vein in relation to the accompanying artery by using CT venography. Korean J Radiol. 2011;12:327-40.
- Maki DD, Kumar N, Nguyen B, et al. Distribution of thrombi in acute lower extremity deep venous thrombosis implications for sonography and CT and MR venography. AJR Am J Roentgenol. 2000;175:1299-301.
- Pezzulo JA, Perkins AB, Cronan JJ. Symptomatic deep vein thrombosis: diagnosis with limited compression ultrasound. Radiol. 1996;198:67-70.