Bilateral ovarian artery absence in a 95-year-old primiparous British cadaver
Rose Lewis, Natasha Russell, Henry Bergman and Deborah merrick*
School of Life Sciences, University of Nottingham, Queen’s Medical Centre, Nottingham, NG7 2UH, UK.
- *Corresponding Author:
- Deborah Merrick
School of Life Sciences U niversity of Nottingham Queen’s Medical Centre Nottingham NG7 2UH, UK
Tel: +44 115 82 30117
E-mail: deborah.merrick@nottingham.ac.uk
Date of Received: April 8th, 2015
Date of Accepted: August 16th, 2015
Published Online: May 19th, 2016
© Int J Anat Var (IJAV). 2016; 9: 8–9.
[ft_below_content] =>Keywords
anatomical variation, ovary, ovarian artery, uterine artery, bilateral absence
Introduction
The right and left ovarian arteries typically originate from the anterior aspect of the abdominal aorta at approximately the level of L2. They descend inferiorly from their origin, crossing the pelvic inlet within the suspensory ligament of the ovary to supply blood to the ovaries. Branches may also pass through the mesometrium division of the broad ligament to anastomose with the uterine artery, a branch of the internal iliac artery. Multiple variations in the course of the ovarian arteries have previously been described in the literature. For example, the right ovarian artery has been observed to course posterior to the inferior vena cava [1,2] and the left to course between the renal artery and vein before turning inferiorly close to the medial border of the kidney [3]. Only one report of bilateral absence of the ovarian artery has previously been described in a 38-year-old Tanzanian cadaver (parity status not reported), suggesting this is a rare occurrence [4]. Ovarian veins originate from a plexus in the broad ligament where they drain the corresponding ovary and are in communication with the uterine plexus. The ovarian veins ascend superiorly, anterior to the psoas major muscle and ureter. The right and left ovarian veins drain into the inferior vena cava and left renal vein, respectively.
Case Report
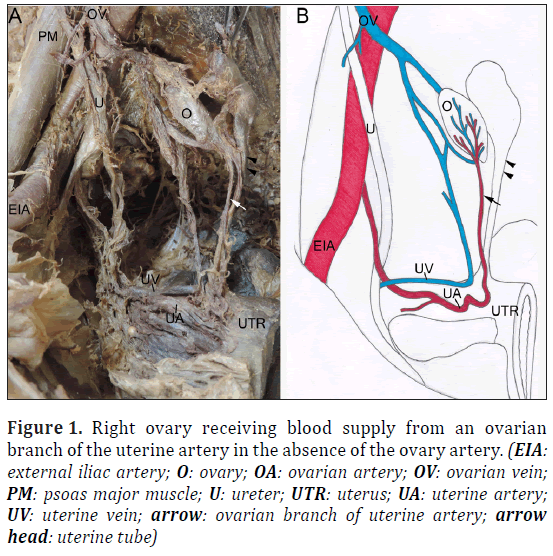
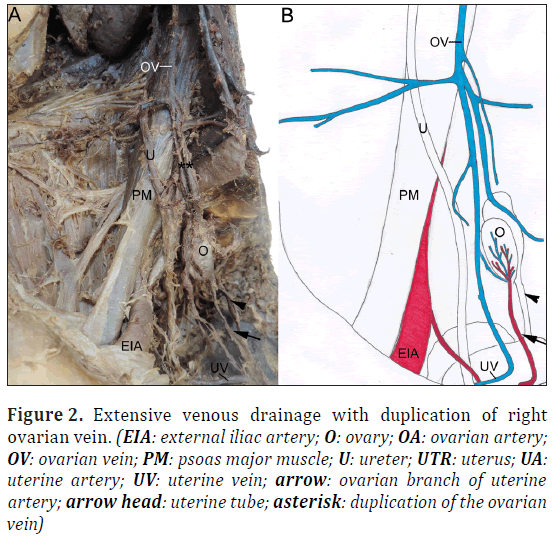
During a routine dissection of a 95-year-old primiparous female cadaver bilateral ovarian artery absence was observed. Associated vasculature including the abdominal aorta and ovarian veins were identified alongside their accompanying branches and tributaries. It was found that both ovaries received their blood supply from a single branch of the uterine artery (Figure 1). Both ovarian veins formed an extensive and complex network of vessels with tributaries from multiple veins, including veins that drained the uterus, ureter, lateral walls of the pelvis and bladder (Figure 2). Duplicated segments of the ovarian veins were also visualized (Figure 2).
Figure 1: Right ovary receiving blood supply from an ovarian branch of the uterine artery in the absence of the ovary artery. (EIA: external iliac artery; O: ovary; OA: ovarian artery; OV: ovarian vein; PM: psoas major muscle; U: ureter; UTR: uterus; UA: uterine artery; UV: uterine vein; arrow: ovarian branch of uterine artery; arrow head: uterine tube)
Figure 2: Extensive venous drainage with duplication of right ovarian vein. (EIA: external iliac artery; O: ovary; OA: ovarian artery; OV: ovarian vein; PM: psoas major muscle; U: ureter; UTR: uterus; UA: uterine artery; UV: uterine vein; arrow: ovarian branch of uterine artery; arrow head: uterine tube; asterisk: duplication of the ovarian vein)
Discussion
A small proportion of people (8.8%) may have gonadal vessel variations that could be explained due to different embryological origins of the vessels [5]. The embryo has nine lateral mesonephric arteries divided into cranial, intermediate and caudal groups [6]. Normally, the gonadal arteries originate from the caudal arteries, however they all have the capability of developing into the ovarian arteries which may account for some variations observed [6]. Gonadal artery variation could also be due to abnormal development of the networks of veins that form the inferior vena cava, inducing the ovarian artery to course posteriorly. An alternative cause may be due to the unusual descent of the ovaries around the kidneys as a consequence of abnormal gubernaculum development. The ovarian vessels follow the course of the ovaries and therefore may end up supplying alternative structures such as the suprarenal glands and diaphragm whilst the ovaries receive their blood supply from an alternative source.
An appreciation of variations that may present in the ovarian vessels is clinically very important. Prior to this case report, bilateral absence of the ovarian artery had only been reported once in the literature [4]. This case study further highlights the importance of the uterine artery during surgical procedures, as it may be the only blood supply to the ovary. Uterine artery occlusion and uterine artery embolization are minimally invasive interventions used to treat uterine fibroids in women who wish to preserve fertility [7]. Surgeons should be aware that vascular occlusion of the uterine artery could lead to ischemia of the ovaries in some rare cases. It is noteworthy that this case study of bilateral ovarian artery absence was from a primiparous female, illustrating for the first time that the anatomical variation has no effect on fertility. The ovarian veins in this cadaver had developed into a major venous drainage source of the pelvis. This is an interesting observation when comparing that to the failed development of the ovarian arteries. One could postulate that the ovarian veins may have developed at the expense of the ovarian arteries.
In conclusion, absence of the ovarian arteries can occur bilaterally and has no influence on the development or functioning of the ovary if there is a blood supply from a branch of the uterine artery. The ovarian veins can develop into prominent venous drainage vessels of the pelvis, with many branches and tributaries.
Acknowledgments
We would like to express our sincere thanks to all staff of the Anatomy Suite at the University of Nottingham (UK) for their technical support and assistance during the dissection.
References
- Sulak O, Albay S, Tagil SM, Malas MA. Ovarian arteries with bilateral unusual courses. Saudi Med J. 2005; 26: 1456–1458.
- Terayama H, Yi SQ, Naito M, Qu N, Hirai S, Kitaoka M, Iimura A, Moriyama H, Steinke H,Itoh M. Right gonadal arteries passing dorsally to the inferior vena cava: embryological hypotheses. Surg Radiol Anat. 2008; 30: 657–661.
- Nayak S. Abnormal course of left ovarian artery. Int J Anat Var (IJAV). 2008; 1: 4–5.
- Kasindye GU, Mwasunga AS, Fabian FM. Bilateral absence of ovarian artery in a Tanzanian female cadaver: a rare variation. Int J Anat Var (IJAV). 2012; 5: 73–75.
- Cicekcibasi AE, Salbacak A, Seker M, Ziylan T, Buyukmumcu M, Uysal II. The origin of gonadal arteries in human fetuses: anatomical variations. Ann Anat. 2002; 184: 275–279.
- Nayak SR1, J JP, D’Costa S, Prabhu LV, Krishnamurthy A, Pai MM, Prakash. Multiple anomalies involving testicular and suprarenal arteries: embryological basis and clinical significance. Rom J Morphol Embryol. 2007; 48: 155–159.
- Brölmann H, Huirne J. Current Treatment Options and Emerging Strategies for Fibroid Management. The Internet Journal of Gynecology and Obstetrics. Volume 10, Number 1.(http://ispub.com/IJGO/10/1/6739).
Rose Lewis, Natasha Russell, Henry Bergman and Deborah merrick*
School of Life Sciences, University of Nottingham, Queen’s Medical Centre, Nottingham, NG7 2UH, UK.
- *Corresponding Author:
- Deborah Merrick
School of Life Sciences U niversity of Nottingham Queen’s Medical Centre Nottingham NG7 2UH, UK
Tel: +44 115 82 30117
E-mail: deborah.merrick@nottingham.ac.uk
Date of Received: April 8th, 2015
Date of Accepted: August 16th, 2015
Published Online: May 19th, 2016
© Int J Anat Var (IJAV). 2016; 9: 8–9.
Abstract
Bilateral ovarian artery absence was identified during a routine dissection of a 95-year-old British female cadaver at the University of Nottingham, UK. This is only the second reported case of bilateral ovarian artery absence in the literature. Although it appears to be a rare anatomical variation, it remains clinically important for those involved in operative, diagnostic and endovascular procedures to be vigilante of such occurrences. In this individual case, the ovaries were supplied solely by an ovarian branch of the uterine artery. Interestingly, this bilateral variation was observed in a primiparous female cadaver, showing that this anatomical variation had no impact on fertility. Both ovarian veins formed an extensive and complex network of pelvic vessels with the presence of duplicated segments.
-Keywords
anatomical variation, ovary, ovarian artery, uterine artery, bilateral absence
Introduction
The right and left ovarian arteries typically originate from the anterior aspect of the abdominal aorta at approximately the level of L2. They descend inferiorly from their origin, crossing the pelvic inlet within the suspensory ligament of the ovary to supply blood to the ovaries. Branches may also pass through the mesometrium division of the broad ligament to anastomose with the uterine artery, a branch of the internal iliac artery. Multiple variations in the course of the ovarian arteries have previously been described in the literature. For example, the right ovarian artery has been observed to course posterior to the inferior vena cava [1,2] and the left to course between the renal artery and vein before turning inferiorly close to the medial border of the kidney [3]. Only one report of bilateral absence of the ovarian artery has previously been described in a 38-year-old Tanzanian cadaver (parity status not reported), suggesting this is a rare occurrence [4]. Ovarian veins originate from a plexus in the broad ligament where they drain the corresponding ovary and are in communication with the uterine plexus. The ovarian veins ascend superiorly, anterior to the psoas major muscle and ureter. The right and left ovarian veins drain into the inferior vena cava and left renal vein, respectively.
Case Report
During a routine dissection of a 95-year-old primiparous female cadaver bilateral ovarian artery absence was observed. Associated vasculature including the abdominal aorta and ovarian veins were identified alongside their accompanying branches and tributaries. It was found that both ovaries received their blood supply from a single branch of the uterine artery (Figure 1). Both ovarian veins formed an extensive and complex network of vessels with tributaries from multiple veins, including veins that drained the uterus, ureter, lateral walls of the pelvis and bladder (Figure 2). Duplicated segments of the ovarian veins were also visualized (Figure 2).
Figure 1: Right ovary receiving blood supply from an ovarian branch of the uterine artery in the absence of the ovary artery. (EIA: external iliac artery; O: ovary; OA: ovarian artery; OV: ovarian vein; PM: psoas major muscle; U: ureter; UTR: uterus; UA: uterine artery; UV: uterine vein; arrow: ovarian branch of uterine artery; arrow head: uterine tube)
Figure 2: Extensive venous drainage with duplication of right ovarian vein. (EIA: external iliac artery; O: ovary; OA: ovarian artery; OV: ovarian vein; PM: psoas major muscle; U: ureter; UTR: uterus; UA: uterine artery; UV: uterine vein; arrow: ovarian branch of uterine artery; arrow head: uterine tube; asterisk: duplication of the ovarian vein)
Discussion
A small proportion of people (8.8%) may have gonadal vessel variations that could be explained due to different embryological origins of the vessels [5]. The embryo has nine lateral mesonephric arteries divided into cranial, intermediate and caudal groups [6]. Normally, the gonadal arteries originate from the caudal arteries, however they all have the capability of developing into the ovarian arteries which may account for some variations observed [6]. Gonadal artery variation could also be due to abnormal development of the networks of veins that form the inferior vena cava, inducing the ovarian artery to course posteriorly. An alternative cause may be due to the unusual descent of the ovaries around the kidneys as a consequence of abnormal gubernaculum development. The ovarian vessels follow the course of the ovaries and therefore may end up supplying alternative structures such as the suprarenal glands and diaphragm whilst the ovaries receive their blood supply from an alternative source.
An appreciation of variations that may present in the ovarian vessels is clinically very important. Prior to this case report, bilateral absence of the ovarian artery had only been reported once in the literature [4]. This case study further highlights the importance of the uterine artery during surgical procedures, as it may be the only blood supply to the ovary. Uterine artery occlusion and uterine artery embolization are minimally invasive interventions used to treat uterine fibroids in women who wish to preserve fertility [7]. Surgeons should be aware that vascular occlusion of the uterine artery could lead to ischemia of the ovaries in some rare cases. It is noteworthy that this case study of bilateral ovarian artery absence was from a primiparous female, illustrating for the first time that the anatomical variation has no effect on fertility. The ovarian veins in this cadaver had developed into a major venous drainage source of the pelvis. This is an interesting observation when comparing that to the failed development of the ovarian arteries. One could postulate that the ovarian veins may have developed at the expense of the ovarian arteries.
In conclusion, absence of the ovarian arteries can occur bilaterally and has no influence on the development or functioning of the ovary if there is a blood supply from a branch of the uterine artery. The ovarian veins can develop into prominent venous drainage vessels of the pelvis, with many branches and tributaries.
Acknowledgments
We would like to express our sincere thanks to all staff of the Anatomy Suite at the University of Nottingham (UK) for their technical support and assistance during the dissection.
References
- Sulak O, Albay S, Tagil SM, Malas MA. Ovarian arteries with bilateral unusual courses. Saudi Med J. 2005; 26: 1456–1458.
- Terayama H, Yi SQ, Naito M, Qu N, Hirai S, Kitaoka M, Iimura A, Moriyama H, Steinke H,Itoh M. Right gonadal arteries passing dorsally to the inferior vena cava: embryological hypotheses. Surg Radiol Anat. 2008; 30: 657–661.
- Nayak S. Abnormal course of left ovarian artery. Int J Anat Var (IJAV). 2008; 1: 4–5.
- Kasindye GU, Mwasunga AS, Fabian FM. Bilateral absence of ovarian artery in a Tanzanian female cadaver: a rare variation. Int J Anat Var (IJAV). 2012; 5: 73–75.
- Cicekcibasi AE, Salbacak A, Seker M, Ziylan T, Buyukmumcu M, Uysal II. The origin of gonadal arteries in human fetuses: anatomical variations. Ann Anat. 2002; 184: 275–279.
- Nayak SR1, J JP, D’Costa S, Prabhu LV, Krishnamurthy A, Pai MM, Prakash. Multiple anomalies involving testicular and suprarenal arteries: embryological basis and clinical significance. Rom J Morphol Embryol. 2007; 48: 155–159.
- Brölmann H, Huirne J. Current Treatment Options and Emerging Strategies for Fibroid Management. The Internet Journal of Gynecology and Obstetrics. Volume 10, Number 1.(http://ispub.com/IJGO/10/1/6739).