Bilateral piercing of anterior scalene muscle by anterior branches of C5 & C6
Neslihan Cankara*, Gulnur Ozguner and Soner Albay
Suleyman Demirel University, Faculty of Medicine, Department of Anatomy, Isparta, Turkiye
- *Corresponding Author:
- Neslihan Cankara, MSc, PhD Candidate
Suleyman Demirel University, Faculty of Medicine, Department of Anatomy, 32260 Isparta, Turkiye
Tel: +90 246 2113305
E-mail: neslihancankara@yahoo.com
Date of Received: March 2nd, 2009
Date of Accepted: July 8th, 2009
Published Online: July 13th, 2009
© IJAV. 2009; 2: 73–74.
[ft_below_content] =>Keywords
brachial plexus, scalene muscles, C5-C6 spinal nerve roots, variation, thoracic outlet syndrome
Introduction
Anatomical variations of the brachial plexus have clinical importance for surgeons, radiologists and anesthetists, since it is a major nerve network supplying the upper limb, which begins in the neck and extends into the axilla [1].
The brachial plexus is formed by the union of the anterior rami of the last four cervical (C5-C8) and first thoracic (T1) nerves that constitute the roots of the brachial plexus. The roots usually pass through the gap between the anterior and the middle scalene muscles with the subclavian artery. In the inferior part of the neck, the roots of the brachial plexus unite to form three trunks [1]. The superior trunk is formed by the union of C5 and C6 roots, the middle trunk is the continuation of C7 root, and the inferior trunk is formed by the union of C8 and T1 roots [1].
Most of the variations in the formation of the brachial plexus have been previously described. Formation of the roots of brachial plexus, and also the relationship between these roots and scalene muscles were especially evaluated for thoracic outlet syndrome (TOS); because abnormalities in the above-mentioned structures may result in compression to the brachial plexus [2].
Case Report
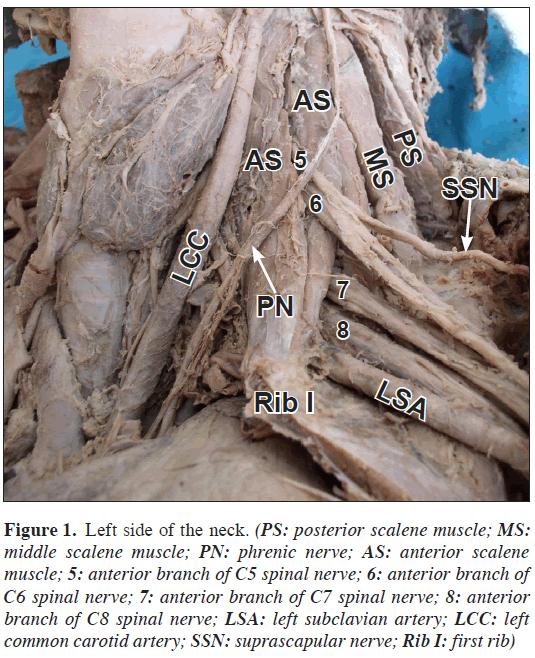
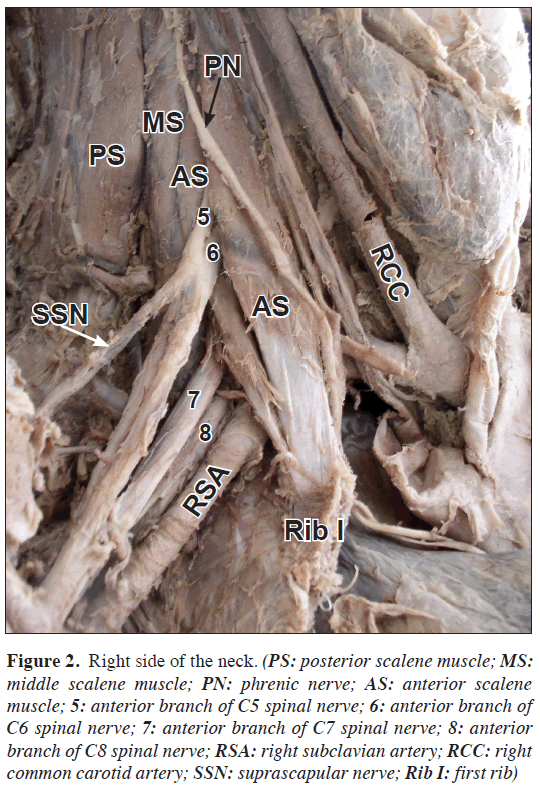
During routine dissections for educational purposes in our department, we encountered variations at the lateral side of the neck of a 25-year-old male cadaver, whose cause of death was traffic accident, without signs of trauma or surgical intervention on his neck. Brachial plexus, scalene muscles and subclavian artery and vein were exposed.
In our case, C5 and C6 nerve roots pierced anterior scalene muscle bilaterally, then formed the superior trunk of brachial plexus after merging on the anterolateral aspect of the muscle. Suprascapular nerve originated from the superior trunk bilaterally (Figures 1, 2).
Figure 1: Left side of the neck. (PS: posterior scalene muscle; MS: middle scalene muscle; PN: phrenic nerve; AS: anterior scalene muscle; 5: anterior branch of C5 spinal nerve; 6: anterior branch of C6 spinal nerve; 7: anterior branch of C7 spinal nerve; 8: anterior branch of C8 spinal nerve; LSA: left subclavian artery; LCC: left common carotid artery; SSN: suprascapular nerve; Rib I: first rib)
Figure 2: Right side of the neck. (PS: posterior scalene muscle; MS: middle scalene muscle; PN: phrenic nerve; AS: anterior scalene muscle; 5: anterior branch of C5 spinal nerve; 6: anterior branch of C6 spinal nerve; 7: anterior branch of C7 spinal nerve; 8: anterior branch of C8 spinal nerve; RSA: right subclavian artery; RCC: right common carotid artery; SSN: suprascapular nerve; Rib I: first rib)
Formations of medial and inferior trunks and all the cords were as usual. Terminal branches of the cords were observed as identified in classical textbooks. Neighborhoods of brachial plexus and subclavian artery, and also scalene muscles and subclavian artery, vein and phrenic nerve showed no variation.
Discussion
The knowledge of variations of brachial plexus is mostly important for anesthetic blocking and surgical interventions in this region.
Similar variations have been mentioned in previously published studies and case reports. Natsis et al. reported only one case of C6 nerve root piercing the root of anterior scalene muscle, among 93 cadavers in their study about variations of superior trunk [3]. Harry et al. reported the incidence of bilaterally pierced anterior scalene muscle by C5 and C6 nerve roots together, like in our case, as 8%. In the same study, C5 and C6 roots were bilaterally piercing the anterior scalene muscle separately in 2% of cases [4].
This variation of superior trunk that is related to scalene muscles may be considered as a predisposing factor for TOS. TOS is the common name of the syndromes characterized with neurogenic and/or vascular symptoms, which are resulted from compression of subclavian vessels and brachial plexus while passing through the cervico-axillary canal. Main findings of TOS are pain, muscular weakness and loose of sense in neck, shoulder, arm and hand [5]. TOS is seen approximately 8% in general population, and neurogenic involvement is present in 95% of the patients. In neurogenic involvement, the cause of the compression is mostly related to bony anomalies. However, in some cases while scalene muscles run to the first rib, brachial plexus may penetrate in the muscles, just like in our case [5].
In some cases of TOS, the differential diagnosis of all radiculopathies, which may compress to C5 and C6 spinal nerve roots as cervical disc hernias, is important. If paresthesia in the dermatome of C5 and C6 is more distinct in distal part of upper extremity, parethesia in thenar region and thumb may show similar symptoms with trap neuropathies. Neurological examination is of prime importance in such situations.
Acknowledgements
We would like to thank Mr. Kenan Halis Kizildag, MSc, for his excellent technical support.
References
- Moore KL, Dalley AF. Clinically Oriented Anatomy. 5th Ed., Philadelphia, Lippincott Williams and Wilkins. 2006; 773–775.
- Kocabiyik N, Yalcin B, Kilic C, Ozan H. Multiple anomalies of he brachial plexus: a case report. Neuroanatomy. 2007; 6: 21–23.
- Natsis K, Totlis T, Tsikaras P, Anastasopoulos N, Skandalakis P, Koebke J. Variations of the course of the upper trunk of the brachial plexus and their clinical significance for the thoracic outlet syndrome: a study on 93 cadavers. Am Surg. 2006; 72: 188–192.
- Harry WG, Bennett JD, Guha SC. Scalene muscles and the brachial plexus: anatomical variations and their clinical significance. Clin Anat. 1997; 10: 250–252.
- Kahraman C, Akçalı Y, Oğuzkaya F, Taşdemir K, Bilgin M, Şahin A. Torasik Outlet Kompresyon Sendromunda Cerrahi Tedavi. Türk Göğüs Kalp Damar Cerrahisi Dergisi. 1997; 5: 300–305. (Turkish)
Neslihan Cankara*, Gulnur Ozguner and Soner Albay
Suleyman Demirel University, Faculty of Medicine, Department of Anatomy, Isparta, Turkiye
- *Corresponding Author:
- Neslihan Cankara, MSc, PhD Candidate
Suleyman Demirel University, Faculty of Medicine, Department of Anatomy, 32260 Isparta, Turkiye
Tel: +90 246 2113305
E-mail: neslihancankara@yahoo.com
Date of Received: March 2nd, 2009
Date of Accepted: July 8th, 2009
Published Online: July 13th, 2009
© IJAV. 2009; 2: 73–74.
Abstract
During routine dissection of a 25-year-old male cadaver, we observed C5 and C6 nerve roots pierced anterior scalene muscle bilaterally and then formed the superior trunk of brachial plexus after merging on the anterolateral aspect of the muscle. Suprascapular nerve originated from the superior trunk bilaterally. Knowledge of such variations may be important in the diagnosis of upper limb paresthesias.
-Keywords
brachial plexus, scalene muscles, C5-C6 spinal nerve roots, variation, thoracic outlet syndrome
Introduction
Anatomical variations of the brachial plexus have clinical importance for surgeons, radiologists and anesthetists, since it is a major nerve network supplying the upper limb, which begins in the neck and extends into the axilla [1].
The brachial plexus is formed by the union of the anterior rami of the last four cervical (C5-C8) and first thoracic (T1) nerves that constitute the roots of the brachial plexus. The roots usually pass through the gap between the anterior and the middle scalene muscles with the subclavian artery. In the inferior part of the neck, the roots of the brachial plexus unite to form three trunks [1]. The superior trunk is formed by the union of C5 and C6 roots, the middle trunk is the continuation of C7 root, and the inferior trunk is formed by the union of C8 and T1 roots [1].
Most of the variations in the formation of the brachial plexus have been previously described. Formation of the roots of brachial plexus, and also the relationship between these roots and scalene muscles were especially evaluated for thoracic outlet syndrome (TOS); because abnormalities in the above-mentioned structures may result in compression to the brachial plexus [2].
Case Report
During routine dissections for educational purposes in our department, we encountered variations at the lateral side of the neck of a 25-year-old male cadaver, whose cause of death was traffic accident, without signs of trauma or surgical intervention on his neck. Brachial plexus, scalene muscles and subclavian artery and vein were exposed.
In our case, C5 and C6 nerve roots pierced anterior scalene muscle bilaterally, then formed the superior trunk of brachial plexus after merging on the anterolateral aspect of the muscle. Suprascapular nerve originated from the superior trunk bilaterally (Figures 1, 2).
Figure 1: Left side of the neck. (PS: posterior scalene muscle; MS: middle scalene muscle; PN: phrenic nerve; AS: anterior scalene muscle; 5: anterior branch of C5 spinal nerve; 6: anterior branch of C6 spinal nerve; 7: anterior branch of C7 spinal nerve; 8: anterior branch of C8 spinal nerve; LSA: left subclavian artery; LCC: left common carotid artery; SSN: suprascapular nerve; Rib I: first rib)
Figure 2: Right side of the neck. (PS: posterior scalene muscle; MS: middle scalene muscle; PN: phrenic nerve; AS: anterior scalene muscle; 5: anterior branch of C5 spinal nerve; 6: anterior branch of C6 spinal nerve; 7: anterior branch of C7 spinal nerve; 8: anterior branch of C8 spinal nerve; RSA: right subclavian artery; RCC: right common carotid artery; SSN: suprascapular nerve; Rib I: first rib)
Formations of medial and inferior trunks and all the cords were as usual. Terminal branches of the cords were observed as identified in classical textbooks. Neighborhoods of brachial plexus and subclavian artery, and also scalene muscles and subclavian artery, vein and phrenic nerve showed no variation.
Discussion
The knowledge of variations of brachial plexus is mostly important for anesthetic blocking and surgical interventions in this region.
Similar variations have been mentioned in previously published studies and case reports. Natsis et al. reported only one case of C6 nerve root piercing the root of anterior scalene muscle, among 93 cadavers in their study about variations of superior trunk [3]. Harry et al. reported the incidence of bilaterally pierced anterior scalene muscle by C5 and C6 nerve roots together, like in our case, as 8%. In the same study, C5 and C6 roots were bilaterally piercing the anterior scalene muscle separately in 2% of cases [4].
This variation of superior trunk that is related to scalene muscles may be considered as a predisposing factor for TOS. TOS is the common name of the syndromes characterized with neurogenic and/or vascular symptoms, which are resulted from compression of subclavian vessels and brachial plexus while passing through the cervico-axillary canal. Main findings of TOS are pain, muscular weakness and loose of sense in neck, shoulder, arm and hand [5]. TOS is seen approximately 8% in general population, and neurogenic involvement is present in 95% of the patients. In neurogenic involvement, the cause of the compression is mostly related to bony anomalies. However, in some cases while scalene muscles run to the first rib, brachial plexus may penetrate in the muscles, just like in our case [5].
In some cases of TOS, the differential diagnosis of all radiculopathies, which may compress to C5 and C6 spinal nerve roots as cervical disc hernias, is important. If paresthesia in the dermatome of C5 and C6 is more distinct in distal part of upper extremity, parethesia in thenar region and thumb may show similar symptoms with trap neuropathies. Neurological examination is of prime importance in such situations.
Acknowledgements
We would like to thank Mr. Kenan Halis Kizildag, MSc, for his excellent technical support.
References
- Moore KL, Dalley AF. Clinically Oriented Anatomy. 5th Ed., Philadelphia, Lippincott Williams and Wilkins. 2006; 773–775.
- Kocabiyik N, Yalcin B, Kilic C, Ozan H. Multiple anomalies of he brachial plexus: a case report. Neuroanatomy. 2007; 6: 21–23.
- Natsis K, Totlis T, Tsikaras P, Anastasopoulos N, Skandalakis P, Koebke J. Variations of the course of the upper trunk of the brachial plexus and their clinical significance for the thoracic outlet syndrome: a study on 93 cadavers. Am Surg. 2006; 72: 188–192.
- Harry WG, Bennett JD, Guha SC. Scalene muscles and the brachial plexus: anatomical variations and their clinical significance. Clin Anat. 1997; 10: 250–252.
- Kahraman C, Akçalı Y, Oğuzkaya F, Taşdemir K, Bilgin M, Şahin A. Torasik Outlet Kompresyon Sendromunda Cerrahi Tedavi. Türk Göğüs Kalp Damar Cerrahisi Dergisi. 1997; 5: 300–305. (Turkish)