Brachial Artery: A Rare Case of Aneurysm and Successful Endovascular Repair
Received: 04-Jul-2023, Manuscript No. ijav-23-6607; Editor assigned: 05-Jul-2023, Pre QC No. ijav-23-6607 (PQ); Accepted Date: Jul 24, 2023; Reviewed: 19-Jul-2023 QC No. ijav-23-6607; Revised: 24-Jul-2023, Manuscript No. ijav-23-6607 (R); Published: 31-Jul-2023, DOI: 10.37532/1308-4038.16(7).287
Citation: Hvizdosova N. Brachial Artery: A Rare Case of Aneurysm and Successful Endovascular Repair. Int J Anat Var. 2023;16(7):349-350.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
with nonspecific symptoms; making early diagnosis challenging. This case report describes a 42-year-old male patient with a brachial artery aneurysm; which was initially misdiagnosed as a benign swelling. The patient’s history; clinical presentation; diagnostic workup; and successful endovascular repair are discussed in detail. This report aims to highlight the importance of considering vascular anomalies in patients presenting with unusual swellings in the upper limb and emphasizes the value of prompt and accurate diagnosis to prevent potential complications.
Keywords
Brachial artery; Aneurysm; Endovascular repair; Upper limb; Vascular anomaly
INTRODUCTION
The brachial artery is a vital conduit for blood flow in the upper limb. Brachial artery aneurysms are relatively rare, accounting for approximately 1% of all peripheral arterial aneurysms [1]. They are commonly asymptomatic and may remain undiagnosed until they lead to complications such as thrombosis, embolism, or rupture. Herein, we present a case of a brachial artery aneurysm in a 42-year-old male, initially misdiagnosed as a benign swelling, which was successfully managed using endovascular repair [2-4].
CASE REPORT
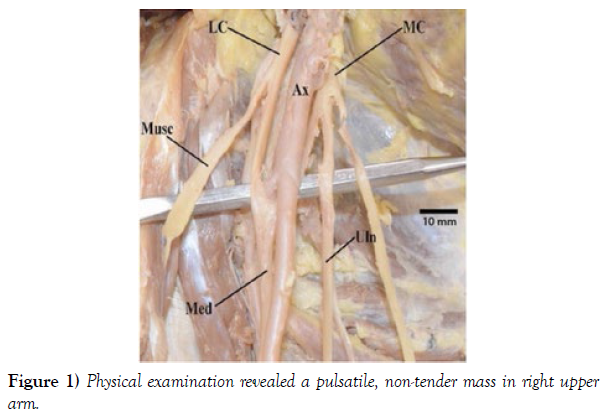
A 42-year-old male presented to our vascular surgery clinic with a progressively enlarging painless swelling in his right upper arm for the past six months. The patient reported no history of trauma or previous medical conditions. Physical examination revealed a pulsatile, non-tender mass approximately 5 cm in diameter, located along the course of the brachial artery in the mid-arm region. Peripheral pulses were intact distal to the swelling, with no signs of ischemia or neurological deficits. The rest of the physical examination was unremarkable.
Diagnostic Workup: Given the patient’s symptomatology and the physical examination findings, an ultrasound examination of the right upper limb was performed. The ultrasound revealed a fusiform aneurysm with a maximal diameter of 5.2 cm, involving the brachial artery. To further assess the extent and characteristics of the aneurysm, a computed tomography angiography (CTA) was performed.
The CTA confirmed the presence of a brachial artery aneurysm, measuring 5.5 cm in length and 5.2 cm in diameter. There were no signs of thrombosis, and the distal arterial segments appeared normal. The patient’s blood pressure and lipid profile were within normal limits, ruling out atherosclerosis as the underlying cause of the aneurysm.
Treatment Strategy: Considering the size of the aneurysm and the potential risk of thrombosis or rupture, a multidisciplinary team, including vascular surgeons, interventional radiologists, and anesthesiologists, discussed the case. The team decided to perform an endovascular repair to preserve the arterial flow and avoid the need for an open surgical procedure, which might lead to more significant morbidity.
Endovascular Repair: Under local anesthesia and fluoroscopic guidance, a small incision was made over the right brachial artery, and a sheath was inserted. A guidewire was advanced through the aneurysm, and a covered stent graft was introduced over the wire and positioned accurately within the aneurysm. The stent graft effectively excluded the aneurysm from the arterial circulation, promoting normal blood flow through the brachial artery.
Postoperative Course: The patient tolerated the endovascular repair well and was discharged the following day with antiplatelet medication to prevent stent thrombosis. Follow-up appointments were scheduled at regular intervals to monitor the stent graft’s function and assess for any signs of complications. Six months after the procedure, a follow-up CTA demonstrated the exclusion of the aneurysm without any evidence of endoleak or stent migration. The patient remained asymptomatic, and peripheral pulses were palpable and normal in the right upper limb (Figure 1).
DISCUSSION
Brachial artery aneurysms are infrequent vascular anomalies that can pose diagnostic challenges due to their nonspecific clinical presentation [5]. In this case, the patient’s history of a gradually enlarging pulsatile swelling in the upper arm, coupled with ultrasound and CTA findings, were instrumental in arriving at an accurate diagnosis. The management of brachial artery aneurysms depends on several factors, including the aneurysm’s size, location, and the presence of symptoms or complications [6-8].
CONCLUSION
This case highlights the significance of considering vascular anomalies, such as brachial artery aneurysms, in patients presenting with unusual swellings in the upper limb. Prompt and accurate diagnosis is crucial to prevent potential complications and guide appropriate treatment strategies [9-10]. Endovascular repair can be a safe and effective treatment option for brachial artery aneurysms, offering the advantage of minimizing morbidity compared to open surgical approaches. Long-term follow-up is essential to assess stent graft function and ensure patient outcomes remain favorable.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST
The author declares no conflicts of interest related to this case report.
REFERENCES
- Penprapa SK, Brianna KR. Duplication of the inferior vena cava: evidence of a novel type IV. Folia Med Cracov. 2020; 28; 60(2):5-13.
- Laurent de K, Stefano M. Variability of repairable bicuspid aortic valve phenotypes: towards an anatomical and repair-oriented classification. Eur J Cardiothorac Surg. 2019; 37(11):9-828.
- Jun S, Zhang-Y, Chuan C. Postoperative neovascularization, cerebral hemodynamics, and clinical prognosis between combined and indirect bypass revascularization procedures in hemorrhagic moyamoya disease. Clin Neurol Neurosurg. 2021; 208:106869.
- Qi L, Xiaojie T, Yafang D. Evaluation of Carotid Plaque Rupture and Neovascularization by Contrast-Enhanced Ultrasound Imaging: an Exploratory Study Based on Histopathology. Transl Stroke Res. 2021; 12(1):49-56.
- Kuo-Shyang J, Shu-Sheng L, Chiung-FC. The Role of Endoglin in Hepatocellular Carcinoma. Int J Mol Sci. 2021;22(6):3208.
- Anri S, Masayoshi O, Shigeru H. Glomerular Neovascularization in Nondiabetic Renal Allograft Is Associated with Calcineurin Inhibitor Toxicity. Nephron. 2020; 144 Suppl 1:37-42.
- Mamikonyan VR, Pivin EA, Krakhmaleva DA. Mechanisms of corneal neovascularization and modern options for its suppression. Vestn Oftalmo. 2016; 132(4):81-87.
- Brian M, Jared PB, Laura E. Thoracic surgery milestones 2.0: Rationale and revision. J Thorac Cardiovasc Surg. 2020 Nov; 160(5):1399-1404.
- Xin W, Bofu L. Aortic Dissection with Rare Anatomical Aortic Arch Variation Depicted by Computed Tomography Angiography. Heart Surg Forum. 2021; 24(2): E407-E408.
- Foivos I, Jonathon K, Daryll B. Aberrant right subclavian artery - a rare congenital anatomical variation causing dysphagia lusoria. Vasa. 2021; 504(5):394-397.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, , Google Scholar, , Crossref
Indexed at, , Google Scholar, Crossref
Indexed at, , Google Scholar, Crossref
Indexed at, , Google Scholar, , Crossref
Indexed at, Google Scholar, Crossref