Brachial plexus posterior cord variability: a case report and review
Edward O*, Arachchi A, Christopher B
University of Melbourne, Parkville VIC 3010, Australia.
- *Corresponding Author:
- Dr Edward O’Bryan
University of Melbourne, Parkville VIC 3010, Australia.
Tel: +61 431 532 539
E-mail: e.obryan@icloud.com
Citation: Edward O, Arachchi A, Christopher B. Brachial plexus posterior cord variability: a case report and review. Int J Anat Var. 2017;10(3):49-50.
Copyright: This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
[ft_below_content] =>Keywords
Brachial plexus; Posterior cord; Axillary nerve; Anatomical variation
Introduction
The brachial plexus is the neural network that supplies motor and sensory innervation to the upper limb. It is typically composed of anterior rami from C5 to T1 spinal segments, which subsequently unite to form superior, middle and inferior trunks. These trunks divide and reunite to form cords surrounding the axillary artery, which terminate in branches of the plexus.
The posterior cord is classically described as a union of the posterior divisions from the superior, middle and inferior trunks of the brachial plexus, with fibres from all five spinal segments. The upper subscapular, thoracodorsal and lower subscapular nerves propagate from the cord prior to the axillary and radial nerves forming terminal branches.
Variability in the brachial plexus is frequently reported in the literature. It is important for clinicians to be aware of possible variations when considering injuries or disease of the upper limb. In this study, a series of variations in the formation of the posterior cord and its branches is reported, with a discussion of the clinical implications.
Case Report
This study focuses on the dissected left brachial plexus of an embalmed 84 year-old Caucasian male, conducted at the University of Melbourne in Australia. An anterior approach to the neck, pectoral girdle, axilla, and upper limb was used to expose each of the components of the brachial plexus. The pectoralis muscles were reflected to allow greater exposure in the axilla. Several anatomical variations were discovered along the brachial plexus, with the scope of this report regarding those involving the formation and branches of the posterior cord.
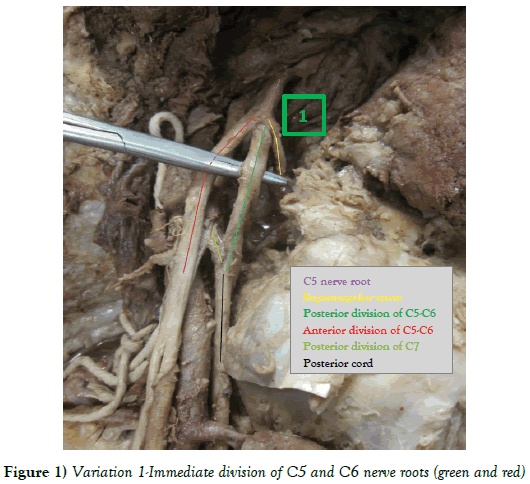
Our cadaveric specimen’s left brachial plexus was formed by the ventral rami of C5 to T1 nerve roots. The C5 and C6 nerve roots united and immediately divided into anterior and posterior divisions; rendering the superior trunk no more than a junctional point. The suprascapular nerve was found to branch from this junction. (Variation 1) (Figure 1).
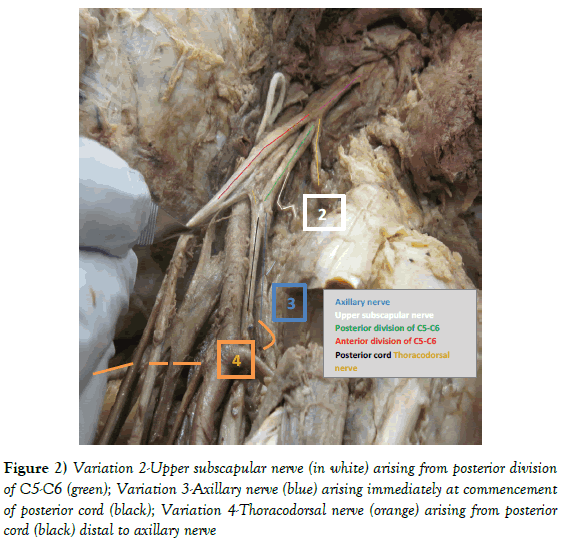
The upper subscapular nerve arose from the posterior division of the superior trunk, prior to the formation of the posterior cord (Variation 2).
A variant nerve, combining the lower subscapular and axillary nerves was the first branch from the posterior cord. It sent branches to innervate subscapularis and teres major prior to innervating teres minor and the deltoid muscle (Variation 3).
The posterior cord terminated with the thoracodorsal and radial nerves (Variation 4) (Figure 2).
Figure 2: Variation 2-Upper subscapular nerve (in white) arising from posterior division of C5-C6 (green); Variation 3-Axillary nerve (blue) arising immediately at commencement of posterior cord (black); Variation 4-Thoracodorsal nerve (orange) arising from posterior cord (black) distal to axillary nerve.
Discussion
We conducted a search using PubMed, Cochrane Library and Ovid Medline to assess for precedence in these variations individually, as a whole and of other posterior cord variations. The individual variations that were searched for include; the lack of a superior trunk, branches arising from posterior divisions, a high branching axillary nerve and an axillary nerve innervating other muscles. The search terms and results are outlined in Table 1.
| Database | Search Terms | Results |
|---|---|---|
| Cochrane Library | Brachial plexus variation | 12 studies matched |
| Ovid Medline | Posterior cord variation | 1088 studies matched |
| PubMed | Brachial plexus variation | 487 studies matched |
Table 1: Individually posterior cord variations different database.
Of the 1,587 matches, after accounting for duplicates and screening abstracts, fifteen full studies were accessed. Studies ranged from single case reports to larger observational studies.
Rastogi et al [1] conducted a cadaveric study of the bilateral upper limbs of 37 bodies in India and found many similar variations. They found that in 16.2% of cases, no superior trunk was formed, similar to that described in our case report. While they report that the upper and lower subscapular nerves were normal in all 74 limbs, 10.8% of cases had a high branching axillary nerve from the posterior division of the superior trunk. The axillary nerve carried the thoracodorsal nerve in 22.9% of cases. Fazan et al [2], Muthoka et al [3] also described the thoracodorsal nerve arising from the axillary nerve, with an incidence of 13% and 10.3% respectively.
Another Indian study by Chaudhary et al [4], studied the bilateral upper limbs of 30 bodies. While 86.67% of specimens exhibited the classically described plexus, 13.33% had very similar variations to those described above. The upper subscapular nerve, thoracodorsal nerve and axillary nerve were found to arise from the posterior division of the superior trunk in 8.33%, 3.33% and 1.66% specimens respectively. The lower subscapular nerve was found to arise from the axillary nerve in 3.33%, while no reports in the literature describe a lower subscapular nerve arising from the posterior division of the superior trunk itself.
Fazan et al [2], Kerr [5], found the upper subscapular nerve arose from the posterior division of the superior trunk in 25.4% and 59% of brachial plexus dissections respectively.
There is pattern to the variations exhibited by our own case report and those found in the literature. A number of muscles around the shoulder girdle are innervated by C5 and C6 ventral rami only; the deltoid, subscapularis and teres muscles. It appears to be common for these muscles to be innervated by nerves arising from the posterior division of the superior trunk as a result, or by a combination nerve (typically axillary) that gives branches to some or all of these muscles.
Descriptions in the literature of the thoracodorsal nerve arising from either the posterior division of the superior trunk, or the axillary nerve are not so easily explained. It does demonstrate that during injury to larger nerves such as the axillary, clinicians should not only examine the typical innervated musculature (i.e., deltoid), but all surrounding musculature, accounting for the possibility of variable innervation. This would be particularly important in traction injuries of the axillary nerve following glenohumeral dislocations considering possible subscapular nerve involvement, adding a muscular component (injury to subscapularis) to predisposing recurrent dislocations.
Unfortunately no study quantified the frequency of these abnormalities appearing in combination, as discovered in our case report. This is an important area for further research; as it would assist in understanding how these variations are formed and what variations should be expected in combination.
Conclusion
Given the high frequency of brachial plexus variability described in the literature, clinicians should not only be aware of possible variations, but also expect to encounter them. This case study and similar cases reported demonstrate some of the possible variations of the posterior cord and their frequency. These variations demonstrate the importance of examining all muscles following upper limb injuries, rather than only the muscles classically described to be innervated by any given terminal branch. An area for further research is the identification and quantification of variations appearing in combination.
References
- Rastogi R, Virendra B, Kshitij B. Posterior cord of brachial plexus and its branches: anatomical variations and clinical implication. ISRN Anat. 2013;3.
- Fazan VPS, Amadeu ADS, Caleffi AL, et al. Brachial plexus variations in its formation and main branches. Acta Cirurgica Brasileira. 2003;18:14-8.
- Muthoka JM, Sinkeet SR, Shahbal SH, et al. Variations in branching of the posterior cord of brachial plexus in a Kenyan population. Journal of Brachial Plexus and Peripheral Nerve Injury. 2011;6:1
- Chaudhary P, Singla R, Kalsey G, et al. Branching pattern of the posterior cord of brachial plexus: a cadaveric study. J Clin Diagnostic Res. 2011;5:787-90.
- Kerr AT. The brachial plexus of nerves in man, the variations in its formation and branches. Am J Anat. 1918;23:285-95.
Edward O*, Arachchi A, Christopher B
University of Melbourne, Parkville VIC 3010, Australia.
- *Corresponding Author:
- Dr Edward O’Bryan
University of Melbourne, Parkville VIC 3010, Australia.
Tel: +61 431 532 539
E-mail: e.obryan@icloud.com
Citation: Edward O, Arachchi A, Christopher B. Brachial plexus posterior cord variability: a case report and review. Int J Anat Var. 2017;10(3):49-50.
Copyright: This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The formation and distribution of the brachial plexus is a source of great anatomical variability. This case report details the anatomical variants discovered in the posterior cord of the brachial plexus in a routine cadaveric dissection at the University of Melbourne, Australia. Similar findings in the literature are reviewed and the clinical significance of these findings is discussed.
-Keywords
Brachial plexus; Posterior cord; Axillary nerve; Anatomical variation
Introduction
The brachial plexus is the neural network that supplies motor and sensory innervation to the upper limb. It is typically composed of anterior rami from C5 to T1 spinal segments, which subsequently unite to form superior, middle and inferior trunks. These trunks divide and reunite to form cords surrounding the axillary artery, which terminate in branches of the plexus.
The posterior cord is classically described as a union of the posterior divisions from the superior, middle and inferior trunks of the brachial plexus, with fibres from all five spinal segments. The upper subscapular, thoracodorsal and lower subscapular nerves propagate from the cord prior to the axillary and radial nerves forming terminal branches.
Variability in the brachial plexus is frequently reported in the literature. It is important for clinicians to be aware of possible variations when considering injuries or disease of the upper limb. In this study, a series of variations in the formation of the posterior cord and its branches is reported, with a discussion of the clinical implications.
Case Report
This study focuses on the dissected left brachial plexus of an embalmed 84 year-old Caucasian male, conducted at the University of Melbourne in Australia. An anterior approach to the neck, pectoral girdle, axilla, and upper limb was used to expose each of the components of the brachial plexus. The pectoralis muscles were reflected to allow greater exposure in the axilla. Several anatomical variations were discovered along the brachial plexus, with the scope of this report regarding those involving the formation and branches of the posterior cord.
Our cadaveric specimen’s left brachial plexus was formed by the ventral rami of C5 to T1 nerve roots. The C5 and C6 nerve roots united and immediately divided into anterior and posterior divisions; rendering the superior trunk no more than a junctional point. The suprascapular nerve was found to branch from this junction. (Variation 1) (Figure 1).
The upper subscapular nerve arose from the posterior division of the superior trunk, prior to the formation of the posterior cord (Variation 2).
A variant nerve, combining the lower subscapular and axillary nerves was the first branch from the posterior cord. It sent branches to innervate subscapularis and teres major prior to innervating teres minor and the deltoid muscle (Variation 3).
The posterior cord terminated with the thoracodorsal and radial nerves (Variation 4) (Figure 2).
Figure 2: Variation 2-Upper subscapular nerve (in white) arising from posterior division of C5-C6 (green); Variation 3-Axillary nerve (blue) arising immediately at commencement of posterior cord (black); Variation 4-Thoracodorsal nerve (orange) arising from posterior cord (black) distal to axillary nerve.
Discussion
We conducted a search using PubMed, Cochrane Library and Ovid Medline to assess for precedence in these variations individually, as a whole and of other posterior cord variations. The individual variations that were searched for include; the lack of a superior trunk, branches arising from posterior divisions, a high branching axillary nerve and an axillary nerve innervating other muscles. The search terms and results are outlined in Table 1.
| Database | Search Terms | Results |
|---|---|---|
| Cochrane Library | Brachial plexus variation | 12 studies matched |
| Ovid Medline | Posterior cord variation | 1088 studies matched |
| PubMed | Brachial plexus variation | 487 studies matched |
Table 1: Individually posterior cord variations different database.
Of the 1,587 matches, after accounting for duplicates and screening abstracts, fifteen full studies were accessed. Studies ranged from single case reports to larger observational studies.
Rastogi et al [1] conducted a cadaveric study of the bilateral upper limbs of 37 bodies in India and found many similar variations. They found that in 16.2% of cases, no superior trunk was formed, similar to that described in our case report. While they report that the upper and lower subscapular nerves were normal in all 74 limbs, 10.8% of cases had a high branching axillary nerve from the posterior division of the superior trunk. The axillary nerve carried the thoracodorsal nerve in 22.9% of cases. Fazan et al [2], Muthoka et al [3] also described the thoracodorsal nerve arising from the axillary nerve, with an incidence of 13% and 10.3% respectively.
Another Indian study by Chaudhary et al [4], studied the bilateral upper limbs of 30 bodies. While 86.67% of specimens exhibited the classically described plexus, 13.33% had very similar variations to those described above. The upper subscapular nerve, thoracodorsal nerve and axillary nerve were found to arise from the posterior division of the superior trunk in 8.33%, 3.33% and 1.66% specimens respectively. The lower subscapular nerve was found to arise from the axillary nerve in 3.33%, while no reports in the literature describe a lower subscapular nerve arising from the posterior division of the superior trunk itself.
Fazan et al [2], Kerr [5], found the upper subscapular nerve arose from the posterior division of the superior trunk in 25.4% and 59% of brachial plexus dissections respectively.
There is pattern to the variations exhibited by our own case report and those found in the literature. A number of muscles around the shoulder girdle are innervated by C5 and C6 ventral rami only; the deltoid, subscapularis and teres muscles. It appears to be common for these muscles to be innervated by nerves arising from the posterior division of the superior trunk as a result, or by a combination nerve (typically axillary) that gives branches to some or all of these muscles.
Descriptions in the literature of the thoracodorsal nerve arising from either the posterior division of the superior trunk, or the axillary nerve are not so easily explained. It does demonstrate that during injury to larger nerves such as the axillary, clinicians should not only examine the typical innervated musculature (i.e., deltoid), but all surrounding musculature, accounting for the possibility of variable innervation. This would be particularly important in traction injuries of the axillary nerve following glenohumeral dislocations considering possible subscapular nerve involvement, adding a muscular component (injury to subscapularis) to predisposing recurrent dislocations.
Unfortunately no study quantified the frequency of these abnormalities appearing in combination, as discovered in our case report. This is an important area for further research; as it would assist in understanding how these variations are formed and what variations should be expected in combination.
Conclusion
Given the high frequency of brachial plexus variability described in the literature, clinicians should not only be aware of possible variations, but also expect to encounter them. This case study and similar cases reported demonstrate some of the possible variations of the posterior cord and their frequency. These variations demonstrate the importance of examining all muscles following upper limb injuries, rather than only the muscles classically described to be innervated by any given terminal branch. An area for further research is the identification and quantification of variations appearing in combination.
References
- Rastogi R, Virendra B, Kshitij B. Posterior cord of brachial plexus and its branches: anatomical variations and clinical implication. ISRN Anat. 2013;3.
- Fazan VPS, Amadeu ADS, Caleffi AL, et al. Brachial plexus variations in its formation and main branches. Acta Cirurgica Brasileira. 2003;18:14-8.
- Muthoka JM, Sinkeet SR, Shahbal SH, et al. Variations in branching of the posterior cord of brachial plexus in a Kenyan population. Journal of Brachial Plexus and Peripheral Nerve Injury. 2011;6:1
- Chaudhary P, Singla R, Kalsey G, et al. Branching pattern of the posterior cord of brachial plexus: a cadaveric study. J Clin Diagnostic Res. 2011;5:787-90.
- Kerr AT. The brachial plexus of nerves in man, the variations in its formation and branches. Am J Anat. 1918;23:285-95.