Caring for caregivers: impact of covid-19 on the mental health of health care workers
2 Resident Physician, Brooklyn, New York, USA
3 Maimonides Medical Center, Brooklyn, USA
4 University of California, Berkeley, California, United States
5 Department of Neurosurgery, University of Michigan, Medical Center Drive, 3552 Taubman Center, Ann Arbor, USA
6 Psychiatrist in Brooklyn, New York, USA
Received: 27-Mar-2023, Manuscript No. puljcpn-23-6272; Editor assigned: 29-Mar-2023, Pre QC No. puljcpn-23-6272 (PQ); Accepted Date: Mar 31, 2023; Reviewed: 30-Mar-2023 QC No. puljcpn-23-6272 (Q); Revised: 31-Mar-2023, Manuscript No. puljcpn-23-6272 (R); Published: 27-Apr-2023, DOI: 10.37532/puljcpn.2023.6(2).1-8
Citation: Bodic M, Hayes S, Su Z, et al. Caring for caregivers: impact of covid19 on the mental health of health care workers. J Clin Psychiatry Neurosci. 2023; 6(2):1-8.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Health Care Workers (HCWs) are facing unprecedented levels of COVID-19-related psychological stress. Death by suicide has been reported in frontline providers taking care of COVID-19 patients in NYC. This study looks at the impact of COVID-19 on HCWs based on levels of exposure to patient, as well as clinical and non-clinical work.
Objective: Measure the impact COVID-19 on the psychological wellbeing of HCWs.
Methods: IRB-approved, cross-sectional study was conducted via selfadministered Qualtrics survey including demographic data, validated scales for depression (PHQ-9), anxiety (GAD-7), and Post-Traumatic Stress (PC-PTSD-5). HCWs’ own suggestions were also collected.
Results: Among 1109 respondents (17% response rate, 45% clinical and 55% non-clinical), 53% had worked directly with COVID patients. 57.6% screened positive for anxiety, 63.4% for depression and 28.5% for PTSD. Scores were significantly higher in direct contact HCWs (p<0.007). 41% felt the need for Mental Health (MH) support. Perceived need for MH was the biggest predictor in screening positive for anxiety (P<0.0001), depression, and PTSD. Suggestions included more access to MH resources, PPE, time off and managerial support.
Conclusion: HCWs experienced significant psychological distress. Our study adds solid data that HCWs need additional MH support.
Key Words
Depression, Anxiety, PTSD
Introduction
Health Care Worker (HCW) Mental Health (MH) has been a growing and difficult discussion as this population is constantly in emotionally charged environments with excessive workloads, where reaching out for aid may be stigmatized [1-4]. That said, the benefits of investing in this important subject are crucial to countering the risks, which include overall poorer quality of care due to medical errors, increased patient falls, increased infections, and low patient satisfaction scores. In March 2020 WHO declared novel coronavirus SARS-CoV-2(COVID-19) a global pandemic. As of January 2022, it has infected over 328 million people worldwide with 5.5 million confirmed deaths, putting HCWs under unprecedented demand and stressors on top on pre-existing baseline psychiatric pathology [5, 6]. Given there has been MH decline in HCWs during other pandemics, it was expected that the COVID-19 pandemic would have similar effects on HCWs. The increased prevalence of mental health symptoms in HCWs associated with this pandemic have been reported in many countries, with meta-analyses of COVID-19’s impact on the HCW’s MH showing significantly high prevalence of anxiety, depression and PTSD symptoms [7-12].
Additionally, frontline HCWs were reported to have higher scores than non-front line workers [13]. One study done in New York City based hospitals regarding HCWs MH measured high positive screens for acute distress, anxiety and depression while other studies showed high distress in multiple areas of life as well as explored various methods to help with resilience and support within the hospitals. The hospital of focus in this study is Maimonides Medical Center (MMC), where more than half of the population within the hospital’s area of service is within the 2018 near poverty range, with a good number in the poverty range [14-17]. Higher levels of poverty such as these were noted to have higher numbers of cases, increased hospitalizations and deaths during the direct contact wave [18]. Due to the high risk population along with knowledge regarding the effects of pandemics on HCW’s MH, this study sought to assess levels of depression, anxiety, PTSD symptoms, substance use and overall well-being of the staffs at this time while determining what interventions or support could be put into play for the expected return of COVID-19 to help maintain HCWs’ wellbeing.
Study objectives
In this study we aim to measure the impact of COVID-19 has had on the psychological wellbeing of HCWs at Maimonides Medical Center. We will measure psychological distress including depression, anxiety and PTSD symptoms among HCWs who were involved in the treatment and management of COVID patients including physicians, nurses, technician, clerical staffs, maintenance staffs, and administrators. We will also compare the degree and severity of symptomatology between clinical staff and non-clinical staff based on levels of exposure. From this data we will try to identify several factors that may have contributed to the distress experienced by HCWs. We hope to use these results to generate important evidence on the development of clinical and policy strategies to support HCWs during such high stress public health crises by disseminating this data to the responsible authorities for us to be better informed about what services and supports are needed. Furthermore, we expect this survey would better prepare us in addressing the psychological needs of HCW in future public health crises.
HYPOTHESIS
HCW would experience new onset psychological distress including depression, anxiety and PSTD symptoms. Levels of psychological distress will be directly proportional to the degree of exposure to high stress environments and events.
Method
Study Design
Design
This is an IRN approved cross sectional study evaluating symptoms of depression, anxiety, PTSD by surveying HCWs using validated scales: PHQ-9 (Patient Health Questionnaire-9), GAD-7 General Anxiety Disorder-7 (GAD-7), (PC-PTSD-5) Primary Care PTSD Screen for DSM-5, respectively.
Data Collection Procedures
A self-administered survey including the above questionnaires (see attached) will be created using the Qualtrics survey platform. The Qualtrics survey link will be emailed to Maimonides HCWs’ work email and also distributed on paper via on-site posts (breakrooms for nurses and physicians) which can be dropped into a locked box located on premise. Weekly reminders will be sent during the study period. The study team will collect the dropped off paper surveys from the locked box every week. Electronically completed survey data will be automatically captured by the Qualtrics platform and accessed by the study team. Surveys will be anonymous and self-administered. The Qualtrics software will not collect data on the IP address of the computer or any other identifying info.
Statistical Analysis
All survey questions were summarized with frequency and percentage and compared across groups with a chi-square test, or fisher exact test where necessary. Univariable logistic regression models were fit for all predictors modeling mental health outcomes (moderate to severe depression, moderate to severe depression, and PTSD). Variables significant in the univariable models at p < 0.05 were then included in a multivariable model for each outcome.
All analyses were conducted using SPSS, version 27.
Results
Demographics
A total of 1109 HCWs completed the surveys during the 60-day period allotted. The response rate was 17% of the entire healthcare work-force at the institution. The numbers of female participants (73.6%) were significantly higher than those who reported as male or other gender. Respondents represented a wide range of health care workers in the facility with both clinical staff (63%) and non-clinical staff (37.0%), including administrators (N=159), Clerical staff (N=128), registered nurses (N=182). Among all the respondents, 53.0% worked on a Covid-19 unit and had direct contact with Covid19 patients during the pandemic (direct contact-line HCWs). 25% of the respondents reported to be deployed to a Covid-19 unit from other specialties. The respondent demographics comparing clinical vs non-clinical and direct contact vs indirect contact HCWs are given in Table 1.
TABLE 1 Demographics of Health Care Workers
| Characteristic | Clinical | Non-Clinical | p-value | Direct contact | Indirect contact | p-value |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||
| Age | ||||||
| 18-29 | 84 (13.7%) | 37 (10.4%) | <0.0001 | 72 (14%) | 49 (10.7%) | <0.0001 |
| 30-39 | 180 (29.5%) | 56 (15.8%) | 156 (30.3%) | 84 (18.4%) | ||
| 40-49 | 115 (18.8%) | 79 (22.3%) | 106 (20.6%) | 87 (19.1%) | ||
| 50-59 | 153 (25%) | 97 (27.3%) | 117 (22.7%) | 134 (29.4%) | ||
| 60-69 | 70 (11.5%) | 73 (20.6%) | 56 (22.7%) | 89 (29.4%) | ||
| 70 and above | 9 (1.5%) | 13 (3.7%) | 8 (1.6%) | 13 (2.9%) | ||
| Gender | ||||||
| Female | 467 (76.9%) | 244 (68.2%) |
0.006 |
376 (73.6%) | 341 (74.5%) |
0.216 |
| Male | 137 (22.6%) | 113 (31.6%) | 131 (25.6%) | 117 (25.5%) | ||
| Other | 3 (0.5%) | 1 (0.3%) | 4 (0.8%) | 0 (0%) | ||
| Race | ||||||
| African American | 82 (13.3%) | 51 (14.3%) | <0.0001 | 69 (13.3%) | 62 (13.5%) | <0.0001 |
| Asian | 119 (19.3%) | 31 (8.7%) | 101 (19.5%) | 49 (10.7%) | ||
| Caucasian | 277 (45%) | 207 (58%) | 232 (44.7%) | 256 (55.9%) | ||
| Hispanic | 58 (9.4%) | 31 (8.7%) | 43 (8.3%) | 48 (10.5%) | ||
| Other | 79 (12.8%) | 37 (10.4%) | 74 (14.3%) | 43 (9.4%) | ||
| Marital Status | ||||||
| Divorced/Separated | 45 (7.3%) | 48 (13.4%) |
0.024 |
44 (8.5%) | 48 (10.5%) |
0.465 |
| Married | 334 (54.4%) | 188 (52.5%) | 278 (53.6%) | 248 (54.1%) | ||
| Single | 208 (33.9%) | 103 (28.8%) | 174 (33.5%) | 140 (30.6%) | ||
| Widowed | 17 (2.8%) | 11 (3.1%) | 16 (3.1%) | 11 (2.4%) | ||
| Other | 10 (1.6%) | 8 (2.2%) | 7 (1.3%) | 11 (2.4%) | ||
| Role | ||||||
| Administrator | 35 (5.7%) | 124 (34.9%) | <0.0001 | 32 (6.2%) | 129 (28.3%) | <0.0001 |
| Allied HC professional | 84 (13.7%) | 12 (3.4%) | 60 (11.5%) | 36 (7.9%) | ||
| Attending physician | 95 (15.4%) | 2 (0.6%) | 70 (13.5%) | 28 (6.1%) | ||
| Clerical staff | 42 (6.8%) | 86 (24.2%) | 34 (6.5%) | 94 (20.6%) | ||
| Maintenance staff | 1 (0.2%) | 8 (2.3%) | 4 (0.8%) | 5 (1.1%) | ||
| Registered nurse | 168 (27.3%) | 14 (3.9%) | 155 (29.8%) | 28 (6.1%) | ||
| Resident physician | 57 (9.3%) | 2 (0.6%) | 54 (10.4%) | 5 (1.1%) | ||
| Technician | 40 (6.5%) | 20 (5.6%) | 41 (7.9%) | 21 (4.6%) | ||
| Other | 93 (15.1%) | 87 (24.5%) | 70 (13.5%) | 110 (24.1%) |
COVID-19 status and related issues
Significant differences were noted in self-reported Covid-19 status and related issues among the survey respondents. Perception of having Covid-19 (presence of symptoms attributed to Covid such as, fever, cough, sore throat, loss of taste or smell, joint pain, shortness of breath) was significantly high in direct contact-line HCWs as compared to that in indirect contact-line HCWs. While a third of the direct contact-line HCWs reported to have experienced Covid-19 related symptoms, only 20.0% of the indirect contact-line responded as having had them. (P <0.0001). It is noteworthy that although much lower numbers had tested positive for Covid-19, the group differences remained significant between direct contact and indirect contact-line HCWs (14.7% vs 9.9%; P=0.03). The same was reflected in terms of positivity for Covid-19 antibodies as well. However, when group comparisons were made between clinical and non-clinical HCWs, no such differences in positivity for the virus or antibodies were observed except that significantly more clinical HCWs reported having symptoms attributed to Covid-19 than non-clinical workers (P<0.0001).
While majority of the respondents rated access to PPE, one of the main issues during the pandemic, as equaled or exceeded expectations, as much as 41% HCWs reported that it did not meet their expectations. (Table 2).
TABLE 2 COVID-19 Status and Related Healthcare Worker Data
| Clinical | Non-Clinical | p-value | Direct contact | Indirect contact | p-value | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||
| Clinical | 435 (84.5%) | 178 (39.6%) | <0.0001 | |||
| Redeployed | 179 (29.4%) | 57 (16.2%) | <0.0001 | 192 (37.6%) | 44 (9.7%) | <0.0001 |
| Worked on COVID-19 unit | 435 (71%) | 80 (22.7%) | <0.0001 | |||
| Cared for COVID-19+ patients | 374 (61%) | 16 (4.5%) | <0.0001 | 369 (71.2%) | 24 (5.3%) | <0.0001 |
| Hours with COVID 19+ patients: | ||||||
| 0-10 hours | 217 (42.5%) | 137 (82.5%) | <0.0001 | 179 (37.4%) | 178 (89.4%) | <0.0001 |
| 11-20 hours | 50 (9.8%) | 7 (4.2%) | 53 (11.1%) | 3 (1.5%) | ||
| 21-30 hours | 42 (8.2%) | 4 (2.4%) | 41 (8.6%) | 4 (2%) | ||
| 31-40 hours | 136 (26.7%) | 11 (6.6%) | 137 (28.6%) | 12 (6%) | ||
| >40 hours | 65 (12.7%) | 7 (4.2%) | 69 (14.4%) | 2 (1%) | ||
| Your perceived health condition: | ||||||
| Extremely bad | 4 (0.7%) | 1 (0.3%) | 0.183 | 2 (0.4%) | 3 (0.7%) | 0.528 |
| Somewhat bad | 37 (6.2%) | 21 (6.1%) | 28 (5.6%) | 31 (7%) | ||
| Neither good nor bad | 77 (13%) | 62 (18.1%) | 69 (13.8%) | 72 (16.3%) | ||
| Somewhat good | 307 (51.8%) | 155 (45.2%) | 256 (51.3%) | 206 (46.5%) | ||
| Extremely good | 168 (28.3%) | 104 (30.3%) | 144 (28.9%) | 131 (29.6%) | ||
| Access to PPE: | ||||||
| Far exceeded expectations | 25 (4.1%) | 20 (6.2%) | <0.0001 | 61 (4.8%) | 53 (4.3%) | 0.002 |
| Exceeded expectations | 61 (10%) | 51 (15.8%) | 61 (11.7%) | 53 (12.6%) | ||
| Equaled expectations | 240 (39.3%) | 156 (48.3%) | 195 (37.5%) | 204 (48.7%) | ||
| Short of expectations | 213 (34.9%) | 63 (19.5%) | 180 (34.6%) | 99 (23.6%) | ||
| Far short of expectations | 71 (11.6%) | 33 (10.2%) | 59 (11.3%) | 45 (10.7%) | ||
| Perceived having COVID symptoms | 188 (31.5%) | 66 (19.2%) | <0.0001 | 167 (33.3%) | 89 (20%) | <0.0001 |
| Tested COVID positive | 76 (13.7%) | 33 (10.2%) | 0.136 | 69 (14.7%) | 41 (9.9%) | 0.031 |
| COVID antibody positive | 128 (22.7%) | 62 (19.3%) | 0.244 | 116 (24.2%) | 75 (18.2%) | 0.031 |
Impact of Covid-19 on Mental Health
The data reveal that the pandemic had significant impact on the mental health of HCWs, especially the frontline workers (Table 3). Overall, 21.2% of respondents reported to have experienced an increase in smoking, drinking alcohol or other behaviors that could interfere with work or personal relationships during the pandemics. Of note is that, at least 21 individuals reported having had suicidal ideations at some point during the peak of the pandemic.
TABLE 3 Impact of COVID-19 on HCW Mental Health
| Clinical | Non-Clinical | p-value | Direct contact | Indirect contact | p-value | |
|---|---|---|---|---|---|---|
| Increased smoking, substance abuse/drinking alcohol | ||||||
| Definitely not | 339 (57.1%) | 198 (58.2%) | 0.73 | 274 (54.5%) | 263 (60.3%) | 0.213 |
| Probably not | 125 (21%) | 75 (22.1%) | 111 (22.1%) | 90 (20.6%) | ||
| Probably yes | 91 (15.3%) | 43 (12.6%) | 77 (15.3%) | 59 (13.5%) | ||
| Definitely yes | 39 (6.6%) | 24 (7.1%) | 41 (8.2%) | 24 (5.5%) | ||
| PHQ9 score / Depression category | ||||||
| 0-4, No Depression | 60 (10.7%) | 38 (11.7%) | 0.084 | 146 (30.5%) | 179 (43.4%) | 0.001 |
| 5-9, Mild Depression | 189 (33.8%) | 135 (41.5%) | 182 (38%) | 139 (33.7%) | ||
| 10-14, Moderate Depression | 216 (38.6%) | 104 (32%) | 88 (18.4%) | 57 (13.8%) | ||
| 15-27, Moderate-Severe Depression | 95 (17%) | 48 (14.8%) | 63 (13.2%) | 37 (9%) | ||
| GAD7 score / Anxiety category | ||||||
| 0-4, No Anxiety | 207 (37.7%) | 160 (50%) | 0.002 | 169 (36.2%) | 200 (49%) | 0.002 |
| 5-9, Mild Anxiety | 200 (36.4%) | 80 (25%) | 162 (34.7%) | 117 (28.7%) | ||
| 10-14, Moderate Anxiety | 77 (14%) | 40 (12.5%) | 71 (15.2%) | 48 (11.8%) | ||
| 15-21, Severe Anxiety | 65 (11.8%) | 40 (12.5%) | 65 (13.9%) | 43 (10.5%) | ||
| PC-PTSD-5 Screening | ||||||
| <3, Less likely PTSD | 382(71.0%) | 230(72.6%) | 0.704 | 307(66.9%) | 307(76.6%). | 0.007 |
| >=3, Possible PTSD | 156 (25.2%) | 87 (24.3%) | 152 (29.1%) | 94 (20.5%) | ||
Anxiety
About a quarter of the responding HCWs (25.9%) reported a GAD-7 score of 10 or greater and 57.6% reported a GAD>5. This is much higher than the 5.7% prevalence of anxiety in the US adult. Higher number of direct contact workers belonged to the categories of moderate to severe anxiety than indirect contact HCWs (based on GAD-7 Scores, P=0.002).
Depression
Among all those participants who responded, 27.5% reported a PHQ-9 score≥10, indicating a high likelihood of MDD, this is much higher than the prevalence of 7.8% in the general adult population [19]. As well, 63.4% of respondents had a PHQ9≥5 and 11.2% were greater than 15. A significantly high number of direct contact HCWs fell into the categories of both moderate and severe depression, as compared to that of indirect contact HCWs. (P=0.001). However, the comparison between clinical and non-clinical workers did not indicate a significant difference in PHQ-9 scores.
PTSD
Many of the participants (28.5%) reported more than 3 symptoms in the PC-PTSD-5 screening, indicating they are much more likely to meet criteria for PTSD, requiring attention in the future. The direct contact HCWs were also found to have significantly higher number of individuals in the categories of possible PTSD (p=0.007). However, there were no significant differences between clinical and non-clinical workers for positive PTSD screening.
Suicidal Ideation
Mental Health Needs and Access to Care
A total of 410, or 43% of the study respondents reported that they felt the need of some level of mental health support during the pandemic. Of these, the number of direct contact-line HCWs were significantly higher than indirect contact-line workers for mental health support (N=263, 52.4% versus N=144, 32.7%, P<0.0001). Clinical staff also reported significantly higher needs for mental health support than non-clinical HCWs (N=288, 48.6% versus N=155, 33.5%, P<0.0001).
Although, 72.0% (N=425) of the respondents said they were aware that there was a free Employee Mental Health Clinic available through the Department of Psychiatry, it was reportedly used by no more than 25% of all HCWs, demonstrating a gap between being aware of the resource and actually seeking mental health support. There were no significant differences across the various groups in either the awareness or utilization of the mental health support resource available.
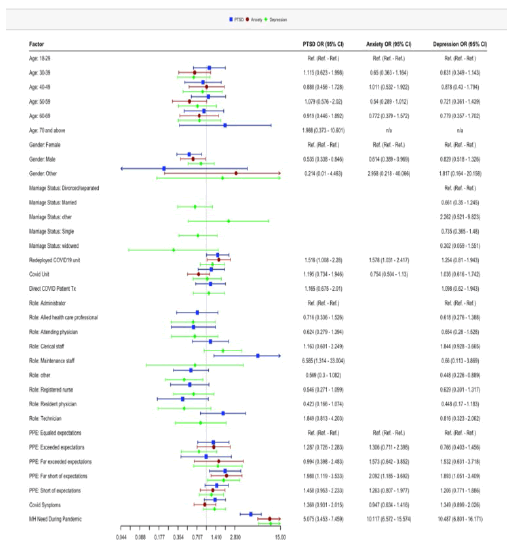
Risk / Predictive Factors of Negative Mental Health Outcomes
Mental Health Care Need: The perceived need for mental health care was the biggest predictor of screening positive for anxiety–12 times more (OR, 12.36; 95% CI, 8.39-18.22; P<0.0001), depression – 10 times more (OR, 10.03; 95% CI, 7.01-14.34; P<0.0001) and possible PTSD – 6 times more (OR, 6.17; 95% CI, 4.43-8.57; P<0.0001), in HCWs in this cohort. Multivariable logistic regression analysis showed that even controlling for other confounding risk factors, the likelihood for these negative mental health outcomes decreased only incrementally.
Redeployment: Being redeployed to a Covid unit increased the odds for anxiety, even after adjusting for other risks. OR, 1.58; 95% CI, 1.03-2.42; P = .04. Redeployment to a Covid unit also increased the odds for depression by 1.5 times (OR, 1.51; 95% CI, 1.08-2.10; P=0.02), however on controlling for other risk factors it did not remain significant. Redeployed HCWs also screened positive for possibly suffering from PTSD (OR, 1.74; 95% CI, 1.24 -2.43; P=0.001) which remained increased even after adjusting for other factors.
PPE: Thoughts of PPE shortage was a predictive factor for screening positive for anxiety, depression and likely PTSD. Perception of PPE availability being far short of expectations, doubled the odds for anxiety (OR, 2.09; 95% CI, 1.19–3.69; P = .01) and PTSD (OR, 1.99; 1.12-3.53; P =.02), and increased the likelihood of screening positive for depression (OR 1.89; 95% CI, 1.05-3.41; P=0.03), despite adjusting for all other factors.
COVID Units
Working on COVID patient units increased the odds for having anxiety (OR, 1.43; 95% CI, 1.05-1.95, P=0.02). Compared with working in a non-COVID unit, working in COVID unit was associated with more severe symptoms of depression (OR, 1.56; 95% CI, 1.15-2.10; P =0.004) and possible PTSD (OR, 1.62; 95% CI, 1.202.19; P =0.002). However, these increased odds did not hold in multivariable analyses controlling for other confounding risk factors. COVID Patient Tx: The odds for moderate to severe depression (OR, 1.41; 95% CI, 1.01-1.99; P=0.02) and possible PTSD (OR, 95% CI, 1.41; 1.05-1.89; P=0.02), increased when HCWs were in the role of direct treatment of Covid patients. However, these increases were not observed on adjustment of other factors. No significant increase in odds for any level of anxiety was detected in the HCWs treating Covid patients.
COVID Symptoms
HCWs who perceived having COVID were 1.4, 1.9, and 1.6 times more likely to screen positive for anxiety (OR, 1.39; 95% CI, 1.001.93; P=0.05), depression (OR, 1.93; 95% CI, 1.41-2.65; P<0.0001) and PTSD (OR, 1.63; 95% CI, 1.18-2.25; P=0.003), respectively. These odds were significantly higher than those for respondents who did not have symptoms attributed to COVID. However, these increased odds did not remain significant after adjusting for all other variables.
The odds ratios for negative mental health outcomes in conjunction with various risk factors can be visualized in (Figure 1).
Figure 1: Odds ratio for negative mental health outcome in conjunction with various risk factors
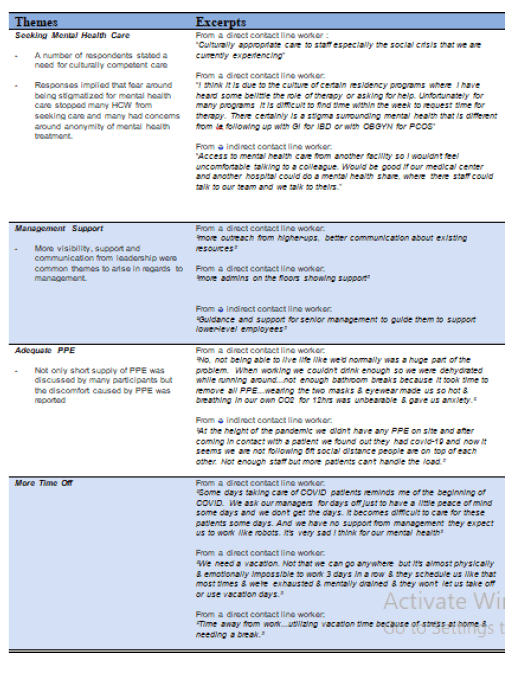
Qualitative
A total of 455 HCWs answered the questionnaire on needs for additional service and support for HCWs and provided their suggestions. Among these, 201 had direct contact with COVID patient care. This information was qualitatively analyzed for themes via Dedoose, a cloud-based data analysis package which allows to review file contents, tagging text elements and applying codes to them. The most frequent suggestions provided by HCWs regardless of their contact with COVID patients were: 1) additional mental health care support, 2) additional management support, 3) adequate PPE and 4) more time-off. (Figure 2) shows thematically grouped excerpts of suggestions from HCWs [19]. There were themes more specific to HCW groups depending on their contact with COVID patients. HCWs, those that had direct contact with COVID patients, suggested more frequently about increased staffing (“More staff on the unit could've prevent the anxiety perhaps during this pandemic crisis.”) and availability of safe spaces. On the other hand, HCWs who had no direct contact with COVID patients, more often suggested the provision of remote working options (“Being allowed to work from home had greatly enabled me to avoid stress & anxiety especially so as not to bring any infection home to and elderly relative living with me. So please support the work at home policy.”).
Discussion
Our cross-sectional survey of mental health impact on HCWs treating patients with COVID-19 are as follows: More than three-fifths of HCWs screened positive for depression. Compared to the 50.4% in the study by Lai and the 48% seen in the study by Shechter, our study found this number to be 63.4%. We also found that 57.6% of our HCWs screened positive for anxiety compared to 5.7% in the general population, 44.6% by Lai and 33% in the study by Shechter.
While HCWs in studies by Lai and Shechter were conducted during the first wave of the pandemic (January and April/2020), our study was done 6 months later (October-November 2020) and even so the percentage of HCWs who screened positive for depression and anxiety increased significantly [20]. This could be representative of HCWs’ MH progressively declining over the course of pandemic. This could also reflect a deficiency of proper mental health support, or inability to access available supports, during the course of the pandemic. This escalation in symptomology raises concerns that after two years of coping with a global pandemic, there is a possibility that our HCW mental health has further deteriorated due to its prolonged course [21].
Greater than one-quarter of HCWs reported moderate depression (PHQ≥10) and 1 out of 10 reported PHQ≥15, which indicates moderately severe depression. Moderate to severe depression can have significant impact on the functioning of the individual; most significantly to HCWs this may have impacted and continue to impact patient care [22]. This level of depression usually requires immediate psychopharmacological treatment with antidepressants and therapy, or even emergent referrals to higher level of care including inpatient psychiatric treatment given concerns of suicidal thoughts and related safety issues.
Our survey identified more than 2% of respondents with suicidal ideation. Given that HCWs have a higher likelihood of suicidality relative to other occupational groups 21-22 and the relationship between suicide ideation and traumatic life events is already well documented, this finding was to be expected. Other studies have also noted that the COVID-19 pandemic has increased the risk of suicide among HCWs [23, 24].
There is also concern that the 2% recorded in this hospital-wide study is an under-representation of the actual prevalence of suicidal ideation. Knowing that PTSD is a known risk factor for suicide, it is notable that nearly one third of HCWs screened positive for this condition. This result suggest that even only 2% of respondents reported suicidal ideations at the time of the survey, near 30% of respondents with PTSD symptoms are at risk of developing these thoughts.
Our data also revealed a significant difference in the impact of the pandemic on the mental health of HCWs with direct versus indirect contact with COVID-19. HCWs who worked directly with COVID19 patients had worse mental health outcomes (OR=1.165), and had significantly high in numbers of both moderate and severe depression (P=0.001), anxiety (P=0.002) as well as PTSD (P=0.007) compared to that of indirect contact HCWs.
More than one-fifth of HCWs (21.2%) reported increased substance use regardless of their patient exposure status.
HCWs who reported need for mental health support were more likely to score positive on depression (OR=10.487), anxiety (OR=10.117) and PTSD scales (OR=5.075).
It was found that the maintenance staff in the hospital were more like to score higher on PTSD scale (OR=6.585) than other departments in the hospital.
We expected respondents who worked clinically to have higher PTSD scores and respondents who worked remotely to have more anxiety, but also were not statically significant.
Even though a majority of HCWs (72%) at our institution were aware of the availability of help in the form of free mental health services, less than a quarter utilized them. Given that the majority of HCWs suggested for mental health support, it is important to note this underuse. This study also explore and identified barriers to seeking mental health care including the desire for culturally competent care, fear of stigma, and the desire for anonymity.
This points to the importance of education and need for open communication lines to bridge the gap between need and access to mental healthcare that would help our frontline workers.
To narrow this perceived need and access gap, various measures were implement during the course of pandemic. For example, an Employee Mental Health Clinic (EMHC) was established and continues to provide a range of services from one-time consultation to long-term psychotherapy and medication treatment for HCWs. A service known as Team Lavender now provides psychological first aid by trained team members, who respond in real time to stress-inducing situations at work. At the administrative level, identifying these individuals and offering resources or alternative roles could reduce distress to these members of the hospital team.
Conclusion
Even though a majority of HCWs (72%) at our institution were aware of the availability of help in the form of free mental health services, less than a quarter utilized them. Given that the majority of HCWs suggested for mental health support, it is important to note this underuse. This study also explore and identified barriers to seeking mental health care including the desire for culturally competent care, fear of stigma, and the desire for anonymity.
Strengths
There are several strengths in this survey. This survey included wide range of HCWs, with good response counts (N=1107), found out mental health impact of the pandemic which could easily set aside during surge using valid screening scales. We also found a difference in the mental health impact depending on the exposure state (direct vs indirect) and gathered qualitative suggestions.
Limitations
There were also limitations, including partial responses in scales which could skew the data and potentially under-reports the total scores. HCWS who chose to respond may not be representative of all the HCWS and people who were affected most might have been more likely to respond. There was a significantly higher representation of female HCWs as compared to that of other genders in this study. Finally, as respondents reported their mental health tate during the peak of the pandemic a number of months after this period of time, recall bias is another limitation.
References
- Zhang C, Yang L, Liu S. Survey of insomnia and related social psychological factors among medical staff involved with the 2019 novel coronavirus disease outbreak. Front Psych.
- Watkins A, Rothfeld M, Rashbaum WK. Top ER doctor who treated virus patients dies by suicide. 2020.
- Chong MY, Wang WC, Hsieh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br j psychiatry. 2004;185(2):127-33.
- Gray P, Senabe S, Naicker N, et al. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: A realist review. Int j environ res public health. 2019;16(22):4396.
- Causey K, Mosser JF. Learning from the COVID-19 pandemic to strengthen routine immunization systems. PLoS Med. 2022;19(2):1003934.
- Imo UO. Burnout and psychiatric morbidity among doctors in the UK: a systematic literature review of prevalence and associated factors. BJPsych bull. 2017;(4):197-204.
- Gray P, Senabe S, Naicker N, et al. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: A realist review. Int j environ res public health. 2019;16(22):4396.
- Hummel S, Oetjen N, Du J, et al. Mental health among medical professionals during the COVID-19 pandemic in eight European countries: cross-sectional survey study. J med Internet res. 2021;23(1):24983.
- Ghaleb Y, Lami F, Al Nsour M, et al. Mental health impacts of COVID-19 on healthcare workers in the Eastern Mediterranean Region: a multi-country study. J Public Health. 2021;43-42.
- Smallwood N, Karimi L, Bismark M, et al. High levels of psychosocial distress among Australian frontline healthcare workers during the COVID-19 pandemic: a cross-sectional survey. Gen psychiatry. 2021;34(5).
- Luo M, Guo L, Yu M, et al. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry res. 2020;291:113190.
- Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry res. 2020;293:113382.
- Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease. 2019. JAMA netw open. 2020;3(3):203976.
- Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen hosp psychiatry. 2020;66:1-8.
- Callahan CM. Strengthening Staff and Administrators' Sense of Workplace Belonging.
- Bernstein CA, Bhattacharyya S, Adler S. Staff emotional support at Montefiore Medical Center during the COVID-19 pandemic. Jt Comm J Qual Patient Saf. 2021;47(3):185-89.
- Yi SS. Taking action to improve Asian American health. Am J Public Health. 2020;110(4):435-7.
- Thompson CN, Baumgartner J, Pichardo C, et al. COVID-19 Outbreak—New York City. 2020. Morb Mortal Wkly Rep. 2020;69(46):1725.
- Perez NB, Lanier Y, Squires A. Inequities along the depression care cascade in African American women: an integrative review. Issues Ment Health Nurs. 2021;42(8):720-29.
- Eng M. Struggles Faced by First-Generation College Students.
- Galbraith N, Boyda D, McFeeters D. The mental health of doctors during the COVID-19 pandemic. BJPsych bulletin. 2021;45(2):93-7.
- Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment. Am J Psychiatry. 2004;161(12):2295-302.
- McFeeters D, Boyda D, Siobhan O. Patterns of stressful life events: distinguishing suicide ideators from suicide attempters. J affect disord. 2015;175:192-98.
- Kingston AM. Break the silence: physician suicide in the time of COVID-19. Mo med. 2020;117(5):426.