Carriage of HBsAg in pregnant women at the university clinic of obstetric gynecology of Cotonou, Benin: Prevalence and associated factors
2 University Clinic of Gynecology-Obstetrics, CNHU-HKM of Cotonou, Benin, Email: ChristianTshabu@hotmail.com
3 Department of Internal Medicine, CNHU-HKM of Cotonou, Benin, Email: KouessiAnthelme90@hotmail.com
4 Department of Internal Medicine, University Hospital Center Oueme-Plateau (CHUD-OP) of Porto-Novo, Benin, Email: FinangnonArmand90@hotmail.com
5 St. Paul Infectious Disease Associates, 1973 Sloan Place, Suite 245 St. Paul MN 55117, USA, Email: FinangnonArmand90@hotmail.com
Received: 05-Aug-2018 Accepted Date: Sep 10, 2018; Published: 25-Sep-2018
Citation: Kpossou AR, Aguemon CT, Dougnonet FF, et al. Carriage of HBsAg in pregnant women at the university clinic of Obstetric gynecology of Cotonou, Benin: Prevalence and associated factors. J Hepato Gastroenterol. 2018;2(2):44-6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
INTRODUCTION: Perinatal transmission is the dominant mode of transmission of the hepatitis B virus in sub-Saharan Africa. The purpose of the present study was to determine the prevalence of HBsAg positivity in pregnant women attending prenatal clinics, and to identify the associated factors. METHODS: It was a descriptive and analytical cross-sectional study, with data collection over a period of one month at the Obstetrics and Gynecology Department (CUGO) at Hubert Koutoukou Maga National Hospital Center (CNHU-HKM) affiliated with the Medical School in Cotonou, Benin. The study population is all pregnant women of all gestational age who received prenatal care at the CUGO during the study period. Pregnant women who signed a consent form were screened using the Determine® Ag HBs rapid diagnostic test. The Pearson Chi-square statistical test was used for comparisons (p<0.05). RESULTS: Of the 250 pregnant women cared for during the study period, 166 consented to the screening. The prevalence of carriage of HBsAg was 14%. Anti-HBc and HBeAg were negative in all cases, indicating chronic infection. A history of hepatic pathology (p=0.01) and the presence of HIV infection (p=0.01) were significantly associated with the carriage of HBs Ag. CONCLUSION: The frequency of HBsAg carriage was high in pregnant women. It is essential to set up a systematic vaccination program, in the first hours of life, for all newborns in our country.
Keywords
Hepatitis B; Pregnant women; Screening; Cotonou.
Introduction
Infection with the hepatitis B virus (HBV) is one of the most common infections worldwide. In fact, about two billion people have markers of previous exposure to HBV, of which nearly two hundred and fifty-seven million subjects are chronic carriers of HBsAg. They constitute a reservoir for the perpetuation of viral transmission [1-4]. The risk of HBV transmission decreases in a setting where there is a periodic perinatal HBV screening, immunoprophylaxis given to infants born to HBV infected mothers and hepatitis B vaccine administered both to high risk mothers and to all newborn infants. Prevention of mother-to-child (vertical) transmission of HBV is a universal public health strategy. The risk of vertical transmission can indeed reach 90% depending on the viral load of the mother [2]. Screening for HBsAg is therefore essential in pregnant women. Indeed, prior knowledge of the HBsAg positive status in the pregnant woman makes it possible to take emergency preventive measures in the hours following birth (twelve to twenty-four hours). In Benin, especially in Cotonou, Bigot et al. [5) found in 1992 and HBsAg carriage prevalence of 8.2% in pregnant women at CUGO at CNHU-HKM and the Hospital of the Mother and Child Lagune (HOMEL) [5]. The objective of our study is to determine the current prevalence of HBsAg in pregnant women 14 years after the previous study and to identify factors associated with HBsAg carriage in order to limit vertical transmission of Hepatitis B in Benin.
Methods
This was a descriptive and analytical cross-sectional study. Data were collected during a 30 day-period from April 15 to May 15, 2017, at the CUGO of CNHU-HKM Cottoned. The study population was all pregnant women of all gestational age who received prenatal care at the CUGO during the study period. The first step of the study involved a one-on-one interview with each pregnant woman aimed at providing education on the basics of HBV infection including modes of transmission to the newborn and strategies to manage them. Those who consented were immediately screened using the rapid test Determine® Ag HBs (Abbott, USA) and the result was immediately communicated to them. Positive serologies were then followed by ELISA (Enzyme-Linked Immunosorbent Assay) for confirmation. Pregnant women with positive ELIZA ELISA were then seen in Hepato-gastroenterology consult. Pregnant women with positive HBsAg were screened for Anti- HBc, subtype IgM and HBeAg. All hepatitis B serologies were performed in the microbiology laboratory of CNHU-HKM. During the interview, a questionnaire was used on every pregnant woman to collect study data including age, marital status, religion, level of education, past medical history, past gynecological and obstetrical history, previous hepatic pathology (defined as a report of liver disease without specifics by a pregnant woman) and risk factors for the children. Collected data were then computerized and analyzed using the Epi data 6.1 software. Potential factors associated with carriage of HBsAg were studied by comparing the socio-cultural characteristics, the risk factors and the past histories of the study group (positive screening serologies) and the control group (Negative serologies). The Pearson Chi-square statistical test was used for this comparison and the observed difference was considered significant for a p<0.05.
Results
Characteristics of the studied population
A total of 250 pregnant women received prenatal care during the period of data collection. Of these, 166 consented to HBsAg screening. The average age of pregnant women was 30 ± 5 years, with the youngest pregnant being 19 years-old and the oldest, 45 years-old. The most represented age groups were 30 to 35 years old (33.8%) and 25 to 30 years-old (26.3%). The majority of pregnant women had a profession (80.6%) and 67.7% were Christian. Three pregnant women (1.5%) were previously vaccinated against hepatitis B. Of the 166 pregnant women, 28 (16.9%) were HIV-positive.
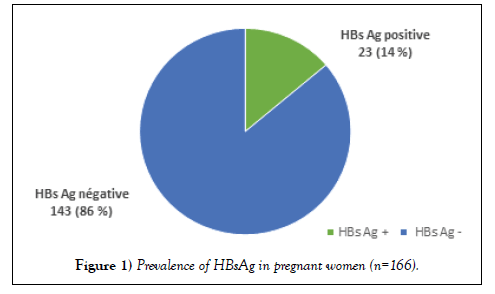
Prevalence of HBsAg in pregnant women
Of the 166 pregnant women who consented to HBV screening, 23 had a positive test with a prevalence of HBsAg of 14% (Figure 1).
Most pregnant women with positive HBsAg (11/23 or 47.8%) were in the 3rd trimester of pregnancy. All 23 pregnant women who screened positive using the Determine® Ag HBs rapid diagnostic test were confirmed positive using ELISA serology testing. HBeAg and HBc IgM Antibodies were negative in all these 23 pregnant women.
Factors associated with the carriage of HBsAg
As shown in Table 1, the history of hepatic pathology and known prior serology of HBV were significantly associated with carriage of HBsAg (p=0.01). HBsAg carriage was higher in pregnant women with a history of liver disease. HBV vaccine status did not significantly affect HBsAg carriage (p=0.32); however, the risk of this carriage was higher in unvaccinated pregnant women (against HBV) than in those who were vaccinated (Table 1).
| HBsAg | 0R | CI 95% | p-value | ||
|---|---|---|---|---|---|
| Variables | Positive | Negative | |||
| Previous hepatic pathology | n (%) | 08 (61.5) | |||
| Present | 05 (38.5) | 134 (88.2) | 4,6 | [1.37-15.77] | 0.01 |
| Absent | 18 (11.8) | 1 | |||
| Vaccination against HBV | n (%) | ||||
| Vaccinated | 01 (33.3) | 02 (66.7) | 1 | 0.32 | |
| Unvacinated | 22 (13.5) | 141 (86.5) | 3.2 | [0.27-36.58] | |
| Anterior serology of HBV | n (%) | ||||
| Positive | 09 (81.8) | 02 (18.2) | 0.01 | ||
| Negative | 01 (02.9) | 34 (97.1) | |||
| Unknown | 13 (10.8) | 107 (89.2) | |||
| HIV | n (%) | ||||
| Positive | 08 (28.6) | 20 (71.4) | 0.2 | [0.07-0.65] | 0.01 |
| Negative | 09 (08.6) | 96 (91.4) | 1 | ||
| Unknown | 06 (18.2) | 27 (81.8) | 0.5 | [0.15-1.77] | |
Table 1: Medical history and carriage of HBsAg.
HIV infection was significantly associated with carriage of HBsAg (p=0.01); (Table 1). None of the usual risk factors for HBV transmission were significantly associated with the carriage of HBsAg in our study (Table 2).
| Variables | HBs Ag | OR | CI 95% | p-value | ||
|---|---|---|---|---|---|---|
| Positive | Negative | |||||
| Multiple sex partners | n (%) | |||||
| Present | 03 (11.6) | 23 (88.4) | 0.8 | [0.22-2.98] | 0.76 | |
| Absent | 20 (14.3) | 120 (85.7) | 1 | |||
| Hepatitis B in the entourage | n (%) | |||||
| Positive | 02 (09.6) | 19 (90.4) | 0.8 | [0.06-10] | 0.85 | |
| Negative | 01 (12.5) | 07 (87.5) | 1 | |||
| Unknown | 20 (14.6) | 117 (85.4) | 1.2 | [0.13-10.25] | ||
| Manicure by common material | n(%) | |||||
| Present | 11 (14.1) | 67 (85.9) | 1.1 | [0.43-2.55] | 0.90 | |
| Absent | 12 (13.6) | 76 (86.4) | 1 | |||
| Tattoo | n (%) | |||||
| Tattoed | 07 (29.2) | 17 (70.8) | 1,6 | [0.59-4.14] | 0.36 | |
| No tattoed | 31 (21.9) | 111 (78.1) | 1 | |||
| Scarifications | n (%) | |||||
| Scarified | 17 (14.7) | 99 (85.3) | 1.3 | [0.46-3.44] | 0.63 | |
| Not scarified | 06 (12) | 44 (88) | 1 | |||
| Surgery | n (%) | |||||
| Operated | 00 (00) | 03 (100) | 0.56 | |||
| Not operated | 23 (14.1) | 140 (85.9) | ||||
| Piercings | n (%) | |||||
| Yes | 04 (21.1) | 15 (78.9) | 2 | [0.26-5.04] | 0.28 | |
| No | 19 (12.9) | 128 (87.1) | 1 | |||
| Blood transfusion | n (%) | |||||
| Transfused | 00 (00) | 11 (100) | 0.34 | |||
| Not transfused | 02 (01.3) | 153 (98.7) | ||||
| Drug IV | n (%) | |||||
| Present | 02 (20) | 08 (80) | 1.8 | [0.35-9.44] | 0.46 | |
| Absent | 21 (13.5) | 135 (86.5) | 1 | |||
Table 2: Risk Factors And Portage Of Hbs Ag
Discussion
The age group most represented in our study population was 30 to 35 years old. Iyalla [6) et al. in Nigeria in 2016 found a similar age range of 30 to 39 years [6]. Younger age groups (21 to 30 years) and (15 to 20 years) were reported by Sidibé et al. [7) in Mali in 2001 [7) and Luuse et al. [8) in Ghana in 2016 [8]. The mean age in our study was 30 ± 5 years as in the study by Iyalla et al. [6]. Sidibé et al. [7) found an average age of 34 years [6]. Sbiti et al. [9) in Morocco in 2016 reported an average age of 28 ± 6 years [7]. Luuse et al. [8) reported an average age of 27.7 years [8]. Noubiap et al. (10) meanwhile found a lower average age of 24.4 ± 5.6 years in Cameroon in 2015 [9]. This age difference could be explained by the fact that in some cultures, women do not work and get married earlier. The prevalence of carriage of HBsAg in the study was 14%. Bigot et al. [5) at CUGO and HOMEL in 1992 found a prevalence of 8.2% [5]. These data reflect that our country Benin was and remains an area of high endemicity for HBV. Indeed, according to a 2013 survey of new blood donors, the national prevalence of HBsAg was 9.9% [11]. Noubiap et al. [10) had found a prevalence of 10.2% in Cameroon in 2016 [9]. Our prevalence was higher than that reported by Luuse et al. [8) in Ghana in 2016 (2.4%) [8]. Sidibé et al. [7) reported a prevalence of 15.5% in Mali in 2001 [7]. In Morocco [9), the prevalence among pregnant women was much lower at 2.3% [11]. Tsegaye et al. [12) reported 4.3% in Ethiopia in 2015 [12]. A similar rate was found by Ngaira et al. [13) in Kenya in 2016 (3.8%) [13]. Abo Salem et al. [14) reported a prevalence of 2.3% in Egypt in 2014 [14]. Braillon et al. [15) found a prevalence of 1.8% in 2009 in France [15]. In Spain [16), a low prevalence of 0.4% was found in 2004 [16]. A much higher prevalence was found in Ivory Coast by Louhoues-Kouacou et al. [17) in 1998 (18%) [18]. Thus, the results found in sub-Saharan Africa (including Benin) were higher than those of the Maghreb, and much higher than those of Europe. These data confirm that most countries in sub-Saharan Africa (including Benin) are areas of high endemicity for HBV. Some countries in Sub-saharan Africa (Except with Ghana, Kenya, Ethiopia) are an area of high endemicity most likely because of the persistence of HBV transmission risk factors: lack of prevention policy of mother-to-child transmission, low level of information to the population about the disease, limited access to healthcare [10,11]. In our study, only 03 pregnant women (1.5%) were vaccinated against hepatitis B. This rate is similar to that found by Sbiti et al. [9) with regard to previous vaccination against hepatitis B (2.4%) [11]. It appears that new vaccination strategies need to be introduced to improve HBV vaccination coverage. There is already a change in the vaccination strategy in Benin since 2002, the hepatitis B vaccine has been introduced in the Expanded Program on Immunization, but this vaccination starts at 6 weeks of age and not the day of birth. The generation affected by the change in strategy is not of procreation age yet and as a result this study should be repeated in few years to measure the impact of the 2002 program on the risk of vertical transmission. Overall, it is necessary to introduce a dose of the vaccine at birth for perinatal transmission of hepatitis B [10,11]. All 23 pregnant women with positive HBsAg had negative HBeAg and IgM anti HBc antibody, confirming the chronicity of all the cases. However, HBeAg negative does not allow us to conclude that there is no viral replication of HBV, because of the possible existence of pre-c mutants. It would have been better to complete the assessment by measuring the viral DNA. Luuse et al. [8), on the other hand, found that 40% of pregnant women who were HBsAg positive also had positive HBeAg and therefore had active viral replication with a high risk of transmission from mother to child [[8]. As for Noubiap et al. [10), they reported that 12.1% of HBsAg positive pregnant women had positive HBeAg [9]. In the Sbiti et al’s study [9), viral DNA was detectable in 89.4% of cases while HBeAg was positive in only 21% of cases [11]. It is therefore necessary to measure viral DNA to establish the real proportion of pregnant in the replication phase. For the moment, measuring this viral load requires sending the blood sample abroad and is expensive (55,000 FCFA) with a turnaround time of 2 to 3 weeks leading to delayed availability of the result.
The government of Benin must therefore work to make available the hepatitis related molecular biology tests in our country. In this study, most pregnant women with positive HBsAg were in the 3rd trimester of pregnancy. Luuse et al. [8) also reported the similar result while in the Iyalla et al. study [6) they were in the 2nd trimester (p=0.01) [7,8]. Tsegaye et al. [12) found that carriage of HBsAg was higher in pregnant women in the first trimester [12]. It should be noted that 120 pregnant women (72.2%) did not know their previous serologic status with respect to HBV. In the Sbiti et al. study [9), 99.6% of pregnant women did not know their HBV serology [11]. In addition, knowledge of prior positive HBV serology was associated with carriage of HBsAg in pregnant women in our study. And more generally, the history of known hepatic pathology was associated with the carriage of HBsAg (p=0.01). It should be noted that in our study, 28 out of 166 pregnant women (16.9%) were HIV-positive and that HIV infection was associated with a higher risk of HBV carriage (p=0.01). This can be explained by the fact that both viruses share the same transmission modes. Finally, 20 pregnant women (12%) had a relative known to be HBsAg positive around them. However, neither the presence of a parent with HBsAg nor any of the other risk factors studied were significantly associated with the carriage of HBsAg in our study. Sidibe et al. [7) identified that scarification and tattooing would increase the risk of carrying HBsAg by a factor of 2 (p=0.01) [7]. In Tsegaye et al. [12), 12.5% of pregnant women with a history of blood transfusion were found to be positive for HBsAg [12-18]. These results could be explained by the fact that these traditional practices, which are widespread in most African societies, were often carried out under conditions of precarious hygiene; and that blood safety was not optimal. Our study did not show the role of these factors probably due to a small population.
Conclusion
The prevalence of carriage of HBsAg was very high among pregnant women in Cotonou, Benin. This prevalence of 14% of HBsAg ranks our country Benin among the highly endemic countries for HBV. It is therefore urgent to set up in our country a policy of prevention of mother-to-child transmission based on screening for HBV in all pregnant women and routine HBV vaccination of all newborns in the first hours of life.
Conflicts of Interest
The authors do not declare any conflict of interest for this work.
Contribution of the Authors
All authors participated in the writing and editing of the article. All authors have read and approved the final manuscript.
Ethical considerations
The study was validated by a local ethics committee. And the pregnant ones included gave their consent.
REFERENCES
- World Health Organization. Global Hepatitis Report 2017, WHO, Geneva. 2017;pp:83.
- Pol S. L’hépatite B demeure un problème de santé publique en France. Pediatric Archives 2010;17:1-5.
- Antona D. L’hépatite B aiguë en France: aspects épidémiologiques. Hépato-Gastro. 2006;13:51-61.
- Denis F, Berges P, Chastagner M, et al. Dépistage de l’Ag HBs in pregnant women: what coverage rate. 2003;33:157-158.
- Bigot K, Kodjoh N, Zohoun I, et al. Seroprevalence of HBsAg antigen of hepatitis B virus in pregnant women and their children. Medi Black Africa.1992;39:487-90.
- Iyalla C, Omunakwe H. A retrospective study of the seroprevalence of antibodies to HBsAg, HIV-1/2 and syphilis among pregnant women at booking in a tertiary hospital in Port Harcourt, southern Nigeria. IOSR J Dental Medi Sci. 2016;15:86-92.
- Sidibe S, Youssoufi B, Traore I. Prevalence of serologic markers of hepatitis B virus in pregnant women in Bamako district, Mali. Bull Soc Pathol Exot. 2001;94:339-341.
- Luuse A, Dassah S, Lokpo S, et al. Seroprevalence of hepatitis B surface antigen among pregnant women attending an antenatal clinic, Volta region, Ghana. J Public Health in Africa. 2016;7:81-83.
- Sbiti M, Khalki H, Benbella I, et al. Seroprevalence of HBsAg in pregnant women in central Morocco. Pan African Med J. 2016;24:1-5.
- Noubiap J, Nansseu J, Ndoula S. Prevalence, infectivity and correlates of hepatitis B virus infection among pregnant women in a rural district of the Far North Region of Cameroon. BMC Public Health. 2015;15:1-7.
- Kodjoh N. State of the fight against hepatitis B and C in Africa. Too much health. 2015;25:141-144.
- Sbiti M, Khalki H, Benbella I, et al. Seroprevalence of HBsAg in pregnant women in central Morocco. Pan African Med J. 2016;24:1-5.
- Tsegaye Y, Zerihun Z, Nega C. Seroprevalence and predictors of hepatitis B virus infection among pregnant women attending routine antenatal care in Arba Minch Hospital, South Ethiopia. Hindawi Publishing Corporation. 2016;1-7.
- Ngaira J, Kimotho J, Mirigi I, et al. Prevalence, awareness and risk factors associated with Hepatitis B infection among pregnant women attending the antenatal clinic at Mbagathi District Hospital in Nairobi, Kenya. Pan african Med J. 2016;24:315.
- Abo Salem M, Mahrous O, El-Shaarawy A, et al. Seroprevalence of hepatitis B among pregnant women attending matrnal and child health centres in Shebin El Kom district (Menoufia governorate). Menoufia Med J. 2014;27:847-852.
- Braillon A, Nguyen-Khac E, Merlin J, et al. Pregnancy and hepatitis B in Picardy: Traceability of screening and prevalence. Gynecology Obstetrics and Fertility 2010; 38: 13-7.
- Gutierrez-Zufiaurre N, Sanchez Hernandez J, Munoz S, et al. Seroprevalence of antibodies against Treponema pallidium, Toxoplasma gondii, rubella virus, hepatitis B and C virus, and HIV in pregnant women. Enferm Infecc Microbiol Clin. 2004;22:512-516.
- Lohoues-Kouacou MJ, Toure M, Hillah J, et al. Maternal-fetal transmission of hepatitis B virus in Côte d'Ivoire. Health Notebook. 1998;8:401-404.