Causes, Pathophysiology, and Results of Emergency Laparotomies
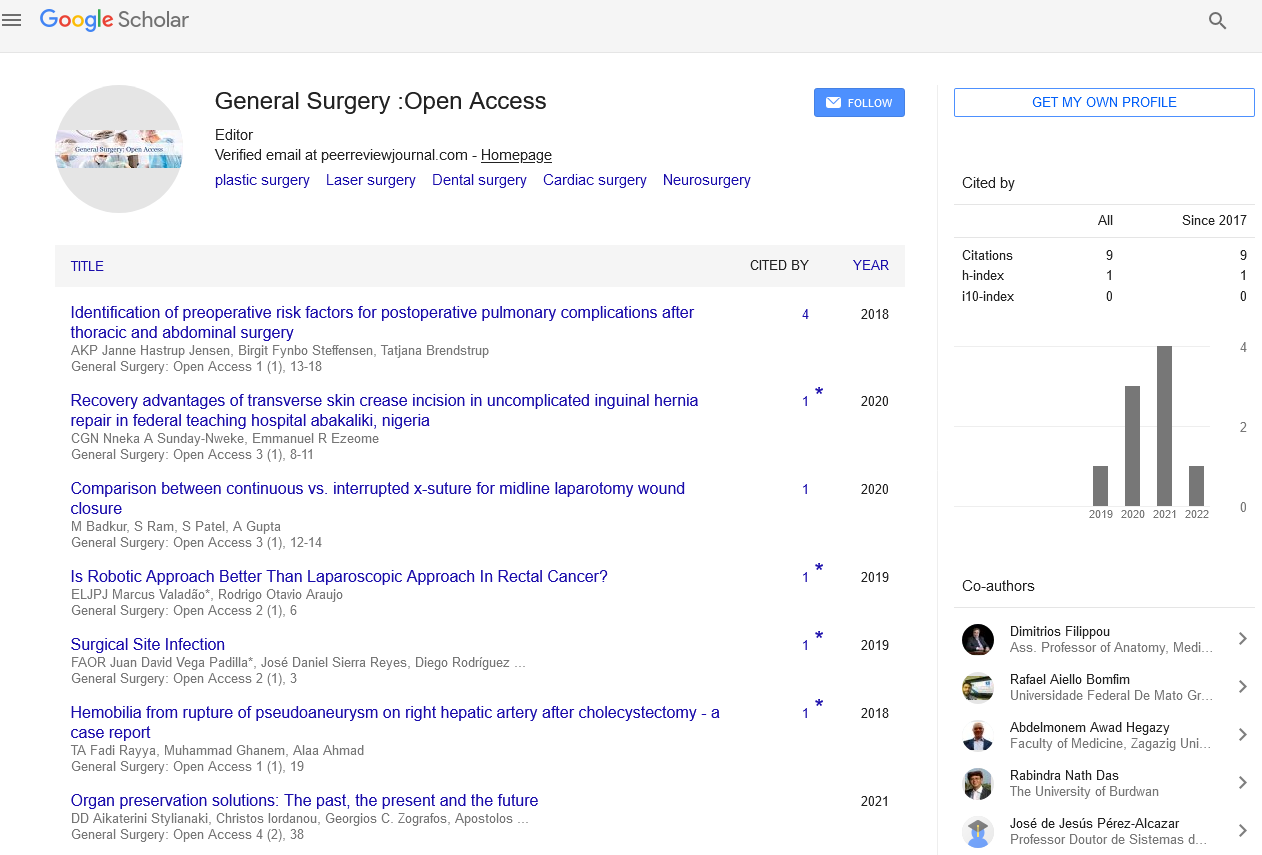
Received: 03-Jan-2023, Manuscript No. PULGSOA-23-6282; Editor assigned: 08-Jan-2023, Pre QC No. PULGSOA-23-6282(PQ); Reviewed: 18-Jan-2023 QC No. PULGSOA-23-6282(Q); Revised: 04-Feb-2023, Manuscript No. PULGSOA-23-6282(R); Published: 14-Feb-2023
Citation: Smith D., Causes, pathophysiology, and results of emergency laparotomies. Gen Surg: Open Access. 2023;6(1)1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Emergency laparotomies have remained a challenging entity for many decades. Only during the past 10 years, serious efforts have been made to improve their outcome by conducting audits and designing care pathways. Indications for emergency laparotomies can be broadly classified into trauma and non-trauma surgeries, which are either done for the control of hemorrhage or/and done for the control of sepsis and organ dysfunction. Goal-directed resuscitation for septic/hemorrhagic shock, consultant-led multidisciplinary teams, and timely transfer to intensive care units form core principles of management for these patients. Global inequity in access to standard and affordable emergency surgeries is an area of concern requiring integrated efforts at the international level.
Key Words
Emergency laparotomy, Perioperative care, Perioperative mortality, Quality improvement
Introduction
Emergency laparotomies form a broad group of time-sensitive surgeries done on a variable patient population. Broadly, they can be divided into trauma and non-trauma laparotomies. Most common non-trauma surgeries include laparotomies done for intestinal perforation and obstruction, while trauma laparotomies are done for hemorrhage control as well as control of peritoneal spillage after bowel injury. The average mortality rate after emergency laparotomies ranges from 10% to 18% in different studies which is much higher than elective surgeries [1]. There is significant global inequity among different countries in terms of access to standard emergency surgical facilities, with lower-income countries sharing the highest burden of surgical mortalities. Regular audits and perioperative care pathways have been used to enhance the outcome of these surgeries in many high-income countries [2]. As these countries already have separate well-developed trauma care networks, only non-trauma laparotomies (acute abdomen) are included in their audits and care pathways for emergency laparotomies. National Emergency Laparotomy Audit (NELA), Australian and New Zealand Emergency Laparotomy Audit-Quality Improvement (ANZELA-QI), and American College of Surgeons National Surgical Quality Improvement Program (ACSNSQIP) are some of the large national-level audit programs for improving care in this subgroup of surgical patients. NELA, a joint national audit, was started in 2012 in response to the high mortality seen in emergency laparotomy in Great Britain and Ireland. NELA gave standards of care that were subject to RAG rating (i.e., red = not met, amber = partially met, and green = met). The 30- day mortality among emergency laparotomy patients reduced from 11% in the first report in 2015 to 9.6% in the fifth report in 2019 [3].
Note that NELA includes only surgeries done on gastrointestinal tracts and excludes all appendicectomies, cholecystectomies as well as trauma, vascular, obstetric, and transplant laparotomies. Elective surgery patient care pathways like Enhanced Recovery After Surgery (ERAS) have caused a significant reduction in morbidity and length of stay for elective surgery patients, but such well-defined evidence-based pathways are still evolving in the field of emergency laparotomy. Extending the components of elective surgery pathways to emergency laparotomies is difficult because these pathways primarily work by attenuation of stress response to surgery through careful planning and preoperative optimization. Such interventions have a limited role in emergency laparotomies, as the stress response cascade has already set in by the time patient qualifies for surgery and preoperative optimization is marred by the paucity of time. Along with this, emergency laparotomies require appropriately selected fluid, electrolytes, nutrition, and pain management regimen throughout the perioperative period which are more complex and difficult to achieve due to the deranged patient physiology [4].
Conclusion
Emergency laparotomies form a heterogeneous group of surgeries with higher mortality when compared to similar elective surgeries. After the introduction of evidence-based pathways and regular audit programs, care for surgical patients has improved in many high-income countries. This is in contrast to the low-income and middle-income groups of countries, where a large number of the population lacks access to affordable basic life, saving surgical care. More dedicated efforts and collaboration at the international as well as national levels are needed to bring quality health care within reach of all inhabitants of the planet.
References
- Barazanchi AW, Xia W, MacFater W, et al. Risk factors for mortality after emergency laparotomy: scoping systematic review. ANZ J. Surg. 2020: 90(10);1895-902.
- Stephens T, Johnston C, Hare S. Quality improvement and emergency laparotomy care: what have we learnt from recent major QI efforts? Clin Med. 2019: 19(6);454.
- Boydâ?Carson H, Gana T, Lockwood S, et al. A review of surgical and periâ?operative factors to consider in emergency laparotomy care. Anaesthesia. 2020: 75;75-82.
- Martin ND, Patel SP, Chreiman K, et al. Emergency laparotomy in the critically ill: futility at the bedside. Crit. care res. pract. 2018; 26.