Childhood adversity as the harbinger for future affective disorders and health problems
Received: 30-Aug-2017 Accepted Date: Sep 01, 2017; Published: 04-Sep-2017
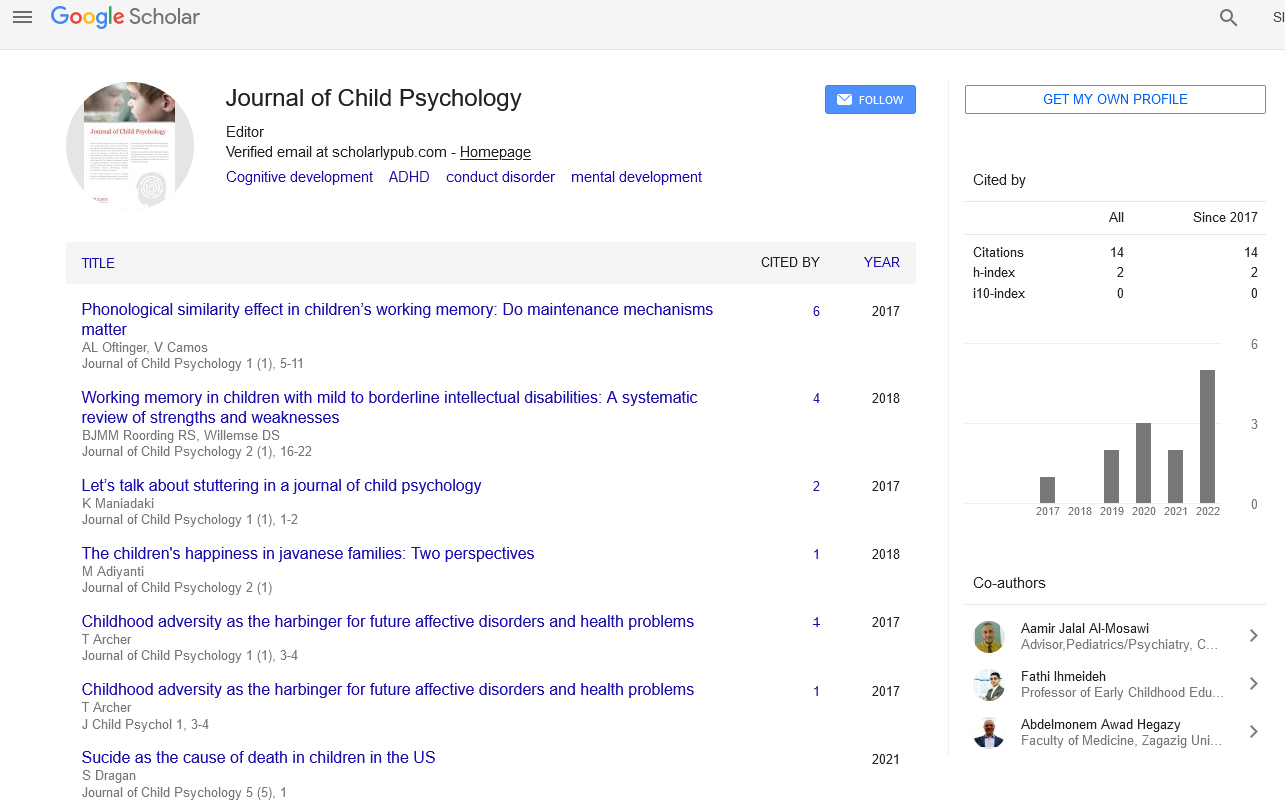
Citation: Archer T. Childhood adversity as the harbinger for future affective disorders and health problems. J Child Psychol. 2017;1(1):3-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Description
Among the several factors contributing to depressiveness among children, maternal alcohol use/abuse, prenatal smoking habit and prenatal maternal obesity and other family-based poor health encumbrances remain a consideration although modulated by social and peer associations, childhood adversity and socioeconomic status [1-7]. Adverse exposure to psychosocial traumatic events during the early part of the child’s life, which incorporates negative experiences involving child maltreatment, caregiver stress and/ or depression, and domestic or community violence, with wide-ranging effects on neural, endocrine, immune, and metabolic physiology, bear strong relationships within epidemiological studies with an elevated lifetime risk of adverse health outcomes, such as diabetes, heart disease, cancers, and psychiatric illnesses [8]. The dysregulation and disharmony of brain neural networks, neuroendocrine stress regulation disruptions, and chronic inflammation, as well as a number of other pathophysiological factors predispose the developing individuals to innumerable health hazardous disorder and risk factors across the life course. In the context of obesity, prenatal stress, adversity among mothers, was linked to reduced levels of childhood adiposity although their cord blood interleukin-6 methylation was related to an increased level of childhood adiposity among Mexican children [9]. Incremental adverse childhood experiences each reduce the infant’s birth weight by 16.33 g and decline its gestational age by 0.063 with smoking emerging as the strongest mediator of the effect on gestational age thereby causing detrimental influences upon maternal reproductive health and well-being, as manifested by mothers’ delivery of the newborn infants who were of reduced birth weight and shorter gestational age [10]. Childhood adversity has been shown to be linked to some 10% elevated risk for developing smoking behavior during adulthood with both childhood adversity and smoking behavior during adulthood related to greater levels of anxiety and depressive symptoms in adulthood [11]. Trauma during childhood, nicotine dependence combined with a greater prevalence for previous hospitalizations was observed among inpatients presenting for both cardiovascular diseases and the positive screening for depressive illness [12].
Several aspects of childhood adversity are associated with later-life health problems and neurodevelopmental detriment. For example, demographic features and depression, such as the long-lasting fear of a family member, long-lasting financial difficulties within the family, serious conflicts in the family, parental divorce and separation, serious or chronic illnesses in the family and alcohol and/or problems within the family were shown to be harbingers for fibromyalgia, expressed through widespread pain and a variety of somatic symptoms [13]. Childhood maltreatment and trauma presents also an increased risk for a pre-diabetic status which is substantiated by the affected individuals’ glucose intolerance, impaired insulin sensitivity, increased levels of C-reactive protein and tumor necrosis factor-α levels, and beta cell function dysregulation [14]. In this regard, it has been shown that omega-3 composition and general trauma during childhood estimates had no relationship to each other although both factors were correlated, in the predicted directions, with negative emotionality with low omega-3 composition and a history of childhood trauma related to the persistence of depressive symptoms during follow-up analysis [15]. It has been found that telomeric length is reduced in individuals exposed to psychosocial stress and in those with depression [16,17]. In male and female participants screened for stressors, depressive status, social interaction, coping strategies and telomere length, it was observed that depressive status and age had direct negative effects on telomere length and both stressors in childhood and recent adulthood had indirect negative effects on telomere length among the female participants whereas for mae participants the effects of stressors and depressive status on telomere length were mediated by social interaction and the coping strategy worry for failure [18]. Childhood adversity, e.g. those traumatic events experienced or perceived violence, low socioeconomic status, maternal depression, family disruption, and institutionalization, all exert an impact on telomere length implying exposed individuals show signs of accelerated erosion of telomeric ends from an early age. Telomere shortening relates to negative health outcomes later on in the lives of these individuals as well as presenting a biomarker to predict health and longevity outcomes [19]. Finally, among patients presenting major depressive disorder it was observed that the exposure to both early and recent stressful environments exerted a widespread effect on white matter microstructure, i.e. reduced fractional anisotropy and axial diffusivity, with the latter correlating negatively with adverse childhood events and the latter with recent stressful events [20].
Adverse childhood experiences exerted a direct effect on depression and relational resilience, i.e. the development of mutually empowering, growthfostering connection in the face of adverse conditions, but not upon individual, i.e. behaviors, thoughts, and actions that promote personal wellbeing and mental health, or contextual, i.e. the influence of environment (context) environment with associated capacity to facilitate growth, resilience [21]. It has been observed that ongoing and life-long expressions of “deliberate self-harm” occurred more frequently among children presenting depression, attention-deficit/hyperactivity disorder and/or oppositional defiant disorder, and also in the context of multiple disorders models accounting for demographic variables and co-occurring neuropsychiatric disorders [22]. They have found that the incidence of maternal anxiety was associated strongly with ongoing and life-long expressions of “deliberate selfharm” in their children, and alternative, among small children particularly expressions of “deliberate self-harm” were related to the mothers’ mood disorders. Similarly, parental adverse childhood experiences were important in the experiences of development of eventual offsprings’ psychological problems [23]. It has been found also that the inattentional component of attention-deficit/hyperactivity disorder and executive functioning problems were associated with childhood depression according to parental ratings [24]. Longitudial analyses of childhood suicide attempters has proved evidence of three types of patient: (i) those individuals presenting all low depressive/ anxious (n=32%), (ii) those presenting all high depressive/anxious (n=16%), and (iii) those presenting high depressive/anxious combined with low aggressive (n=52%) symptom-profiles [25]. Individual presenting the highest likelihood of all the symptom-profiles evidenced a greater probability of reporting younger age-levels for suicide attempts accompanied by substance abuse disorders and violent criminal behaviors.
A marked positive relationship between a variety of adverse life events during childhood and prenatal depression scores among women presenting perinatal depression combined with excessive adrenocorticotropic hormone reactivity to the cold-pressor test has been indicated [26]. Furthermore, those patients presenting a history of any type of adverse life event description displayed a blunted cortisol response to the cold-pressor test and at four weeks showed a heightened adrenocorticotropic hormone stress reactivity to the test. The cold-pressor test presents a cardiovascular performance estimate by immersing the individual’s hand into an ice water container, often for one minute, and measuring changes in blood pressure and heart rate with eventual changes relating to vascular responding and pulse excitability. Additionally, the authors observed a positive and markedly strong correlation between pain tolerance estimates and the cortisol response in the coldpressor test over the whole sample. It was shown also that among female patients presenting a history of childhood onset depression but no evidence of anxiety disorder (n=37) there was a reduction in electroencephalogram left lateral frontal activity in comparison with a group of psychiatrically-healthy control individuals [27] whereas those women patients presenting a history of childhood-onset depressive disorder with pathological levels of anxious apprehension estimated through concurrent generalized anxiety disorder, obsessive compulsive disorder, or separation anxiety disorder diagnoses showed profiles that were indistinguishable statistically from the healthy control group. The authors have presented three conclusions: (i) prefrontal electroencephalogram activity asymmetry provides a neurophysiological marker for depressive illness, (ii) the co-morbidity inherent to depression and anxiety expressions, and (iii) the failure to observe the prevailing relationship between prefrontal electroencephalogram activity asymmetry and levels of diagnosed depression. The children’s mothers’ history of childhood maltreatment and adversity was shown to bear a marked relationship to their offsprings’ internalizing and externalizing problems while maternal antenatal depression, postnatal depression and offspring child maltreatment were indicated as mediating significantly this relationship independently [28]. In a self-report study of rumination, sadness and anger, and depressiveness among children (aged 7–14 years), it was found that anger rumination presented a trans-diagnostic factor for the depressive symptoms and aggressiveness of the children whereas sadness moderated the association between anger rumination and aggression [29].
Perinatal stress-related/inflammatory symptoms are common in women during pregnancy and are risk factors for neurobehavioral disorders, particularly affective and associated co-morbidities and health hazards [30]. Exposure to childhood trauma and adverse environments, mediated by dysregulation of hypothalamic-pituitary-adrenal axis function and a plethora of stress hormone and neuro-immune mobilization of biomarkers, appears to impair a multitude of psychophysiological and health-benefitting process to the eventual detriment of individuals over the life-span.
REFERENCES
- Wolfe JD. Maternal alcohol use disorders and depression in emerging adulthood: Examining the relevance of social ties, childhood adversity, and socioeconomic status. Psychiatry Res. 2017;257:441-5.
- Gould GS, Bovill M, Clarke MJ, et al. Chronological narratives from smoking initiation through to pregnancy of Indigenous Australian women: A qualitative study. Midwifery. 2017;52:27-33.
- Mina TH, Lahti M, Drake AJ, et al. Prenatal exposure to very severe maternal obesity is associated with adverse neuropsychiatric outcomes in children. Psychol Med. 2017;47:353-62.
- Gressier F, Guillard V, Cazas O, et al. Risk factors for suicide attempt in pregnancy and the post-partum period in women with serious mental illnesses. J Psychiatr Res. 2017;84:284-91.
- Dennison-Farris M, Sisson SB, Stephens L, et al. Obesogenic Behaviors, Self-Efficacy, and Depressive Symptoms in American Indian Children. Am Indian Alsk Native Ment Health Res. 2017;24:18-39.
- Kozyrskyj AL, Letourneau NL, Kang LJ, et al. Associations between postpartum depressive symptoms and childhood asthma diminish with child age. Clin Exp Allergy. 2017;47:324-30.
- Merwin SM, Leppert KA, Smith VC et al. Parental depression and parent and child stress physiology: Moderation by parental hostility. Dev Psychobiol. 2017.
- Berens AE, Jensen SKG, Nelson CA. 3rd Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Med. 2017;15:135.
- Wu S, Gennings C, Wright RJ, et al. Prenatal stress, methylation in inflammation-related genes, and adiposity measures in early childhood: the PROGRESS cohort study. Psychosom Med. 2017.
- Smith MV, Gotman N, Yonkers KA. Early Childhood Adversity and Pregnancy Outcomes. Matern Child Health J. 2016;20:790-8.
- Sheikh MA. Confounding and Statistical Significance of Indirect Effects: Childhood Adversity, Education, Smoking, and Anxious and Depressive Symptomatology. Front Psychol. 2017;8.
- Barreto FJN, Garcia FD, Prado PHT, et al. Childhood trauma and factors associated with depression among inpatients with cardiovascular disease. World J Psychiatry. 2017;7:106-113.
- Varinen A, Kosunen E, Mattila K et al. The relationship between childhood adversities and fibromyalgia in the general population. J Psychosom Res. 2017;99:137-42.
- Li L, Garvey WT, Gower BA. Childhood Maltreatment Is an Independent Risk Factor for Prediabetic Disturbances in Glucose Regulation. Front Endocrinol (Lausanne). 2017;8.
- Coryell WH, Langbehn DR, Norris AW, et al. Polyunsaturated fatty acid composition and childhood adversity: Independent correlates of depressive symptom persistence. Psychiatry Res. 2017;256:305-11.
- Fair B, Mellon SH, Epel ES et al. Telomere length is inversely correlated with urinary stress hormone levels in healthy controls but not in un-medicated depressed individuals-preliminary findings. J Psychosom Res. 2017;99:177-80
- Wang X, Sundquist K, Hedelius A, et al. Leukocyte telomere length and depression, anxiety and stress and adjustment disorders in primary health care patients. BMC psychiatry. 2017;17:148.
- Liu JJ, Wei YB, Forsell Y, et al. Stress, depressive status and telomere length: Does social interaction and coping strategy play a mediating role? J Affect Disord. 2017;222:138-45.
- Coimbra BM, Carvalho CM, Moretti PN. Stress-related telomere length in children: A systematic review. J Psychiatr Res. 2017;92:47-54.
- Sara P, Veronica A, Silvia B, et al. Impact of early and recent stress on white matter microstructure in major depressive disorder. J Affect Disord. 2017;225:289-97.
- Howell KH, Miller-Graff LE, Schaefer LM, et al. Relational resilience as a potential mediator between adverse childhood experiences and prenatal depression. J Health Psychol. 2017.
- Simioni AR, Pan PM, Gadelha A, et al. Prevalence, clinical correlates and maternal psychopathology of deliberate self-harm in children and early adolescents: results from a large community study. Rev Bras Psiquiatr. 2017.
- Johnson K, Woodward A, Swenson S. Parents' adverse childhood experiences and mental health screening using home visiting programs: A pilot study. Public Health Nurs. 2017.
- Fenesy MC, Lee SS. Association of ADHD and Executive Functioning with Childhood Depression. J Atten Disord. 2017.
- Hart SR, Van Eck K, Ballard ED, et al. Subtypes of suicide attempters based on longitudinal childhood profiles of co-occurring depressive, anxious and aggressive behavior symptoms. Psychiatry Res. 2017;257:150-5.
- Lara-Cinisomo S, Grewen KM, Girdler SS et al. Perinatal Depression, Adverse Life Events, and Hypothalamic-Adrenal-Pituitary Axis Response to Cold Pressor Stress in Latinas: An Exploratory Study. Womens Health Issues. 2017.
- Nusslock R, Shackman AJ, McMenamin BW et al. Comorbid anxiety moderates the relationship between depression history and prefrontal EEG asymmetry. Psychophysiology. 2017.
- Plant DT, Jones FW, Pariante CM et al. Association between maternal childhood trauma and offspring childhood psychopathology: mediation analysis from the ALSPAC cohort. Br J Psychiatry. 2017.
- Harmon SL, Stephens HF, Repper KK et al. Children's Rumination to Sadness and Anger: Implications for the Development of Depression and Aggression. J Clin Child Adolesc Psychol. 2017;1-11.
- Archer T, Abedini Y. Regional dysregulation and aberrant functional connectivity in ADHD. J Neurosci Neuropsychol. 2016;1:101.