Children with attention deficit hyperactivity disorder, autism spectrum disorder, and co-occurring attention deficit hyperactivity disorder and autism spectrum disorder exhibit autistic traits and empathy.
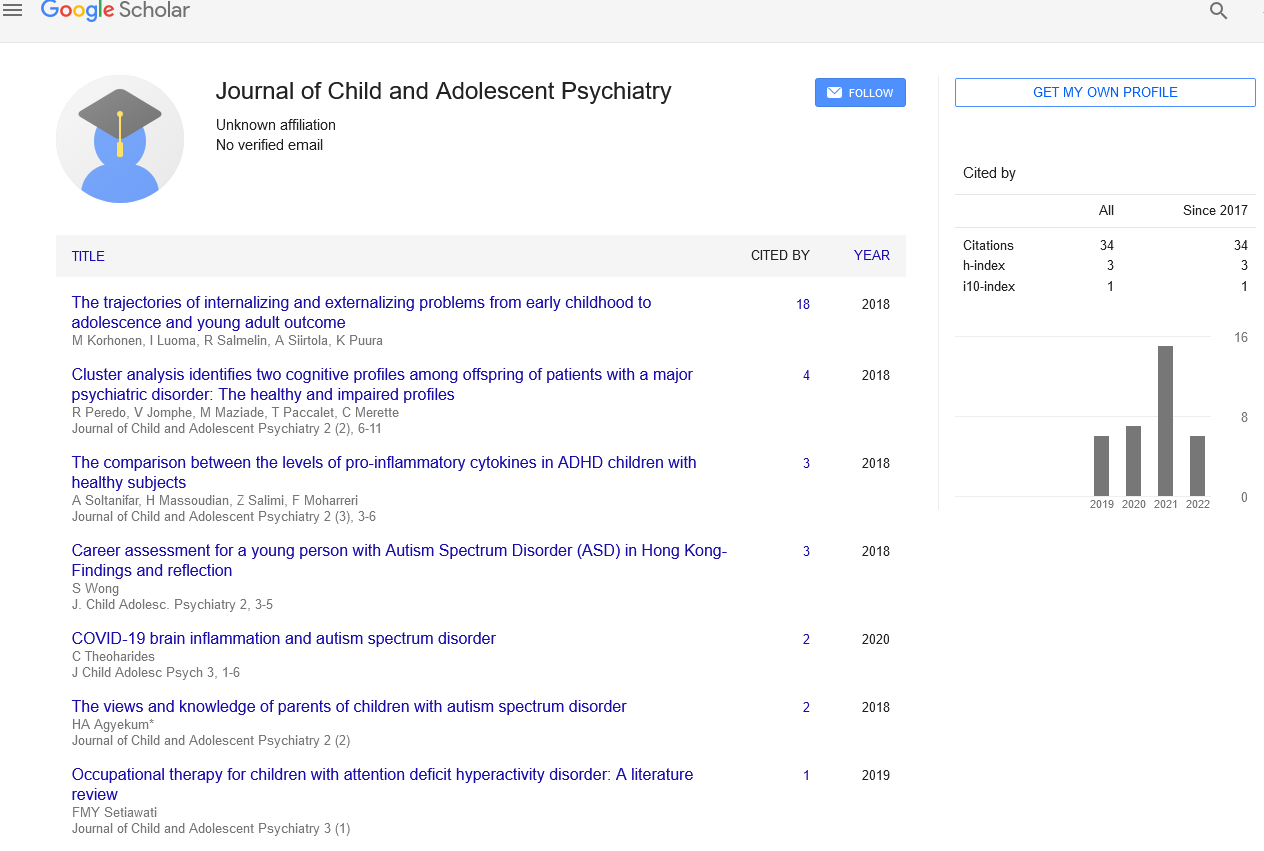
Received: 04-Aug-2022, Manuscript No. PULJCAP-22-5434; Editor assigned: 12-Aug-2022, Pre QC No. PULJCAP-22-5434(PQ); Accepted Date: Aug 30, 2022; Reviewed: 16-Aug-2022 QC No. PULJCAP-22-5434(Q); Revised: 04-Sep-2022, Manuscript No. PULJCAP-22-5434(R); Published: 04-Sep-2022, DOI: 10.37532/puljcap.2022.6(5);33-34.
Citation: James S. Children with attention deficit hyperactivity disorder, autism spectrum disorder, and co-occurring attention deficit hyperactivity disorder and autism spectrum disorder exhibit autistic traits and empathy. J Child Adolescence Psychiatry. 2022; 6(5):33-34.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
One of the most prevalent neurodevelopmental disorders in children is Attention Deficit Hyperactivity Disorder (ADHD), which is closely followed by Autism Spectrum Disorders (ASD). The DSM-5's diagnostic change, which permits a combination diagnosis of ADHD and ASD, introduces new clinical issues related to diagnostic overshadowing, the reliability of clinical judgement, and the potential delay in an ASD diagnosis in kids who present with ADHD. By contrasting children with ASD with and without comorbid ADHD with children presenting ADHD only and children with usual development, we attempted to disentangle the clinical phenotype and uniqueness of the two cooccurring diseases in relation to autism features and empathy. A total of 198 male children between the ages of 6 and 12 were given the child versions of the Autism Quotient (C-AQ) and the Empathy Quotient (CEQ) having verbal abilities commensurate with age and average IQ. Children with ASD and children with ASD+ADHD did not significantly differ in their C-AQ total and subscale scores, C-EQ, or C-EQ scores, according to a univariate analysis, but children with ADHD alone displayed a phenotype that was intermediate between ASD and TD. A Receiver Operating Characteristic (ROC) analysis was used to distinguish between the various phenotypes. Our results support the validity of the C-AQ and C-EQ as behavioural indicators to distinguish TD and an ADHD state from ASD (independent of comorbid ADHD). Intriguingly, in our group, the presence of ADHD does not worsen the clinical phenotype in terms of the distribution of autism features and empathy, indicating that the psychological indicators identified by the two quantitative instruments are accurate regardless of ADHD characteristics. The translational efforts to provide more individualised treatments and prevention measures will benefit from this evidence.
Introduction
A new paradigm of neurodevelopmental disorders was introduced in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, marking Syndrome, "Pervasive Developmental Disorder Not Otherwise Specified," and "Disintegrative Disorder" in favour of a dimensional approach to symptom severity, as well as the possibility a significant transition from a categorical to a dimensional approach of diagnosis. One of the neurodevelopmental disorders in children that is currently most commonly represented in the DSM-5 has had notable changes: Autism Spectrum Disorder (ASD). The removal of sub-diagnoses such as "Autistic Disorder," "Asperger's of a comorbid diagnosis of "ADDHD," were the main changes in the ASD diagnostic category. Restricted repetitive activities have been connected to cognitive rigidity, hyper focus, and problems with predictive coding within the autism phenotype. Numerous studies have confirmed a deficit in Executive Functions (EF) in the ASD population, including verbal working memory, inhibition, and fast visual scanning. EFs, also known as "Hot Executive Functions," are also known to assist people in self-regulating their emotions and empathising with others. These skills are known to be impaired in autistic children, who also have significantly higher deficits in Emotional Regulation (ER) than children with other neurodevelopmental and psychiatric disorders. In addition, those who have trouble controlling their emotions frequently internalise issues like anxiety and despair. ADHD is characterised by underlying cognitive deficits in EF and self-regulation. It's interesting to note that children with ADHD have also been found to have weak social viewpoint assumptions, impaired social cognition, a lack of pragmatic language, and a lack of empathy. According to research on empathy subdomains, ADHD is primarily distinguished by a deficit in emotional empathy rather than its cognitive component, as is typically shown in ASD. Children with ADHD often exhibit violent and/or oppositional behaviours, mood and anxiety disorders, and other internalising and externalising issues, which can make it challenging for them to get along with their peers. Additionally, a lot of kids with ADHD exhibit hyper focus on subjects that appeal to their personal interests and struggle with working memory and processing speed. Previous research has shown that the symptoms of ADHD and ASD can co-occur, with 40%–70% of children with ASD showing co-occurring ADHD and 18%–50% of children with ADHD exhibiting clinical levels of ASD symptoms. When ASD and ADHD co-occur, diagnostic precision may be much more difficult to achieve. In fact, the cognitive and behavioural overlap between the two disorders raises crucial issues about diagnostic overshadowing and necessitates a thorough investigation to shed light on any potential common etiologies. Studying the cooccurrence of the two disorders at an early age is also essential to understanding how they develop and, subsequently, how their routes change as children develop. The improvement of focused treatment is dependent on this longitudinal perspective.
According to prior research, ADHD is intermediate between ASD and control groups in the socio-communicative domain. Therefore, it is possible that ASD and ADHD are two distinct symptoms of a single spectrum condition that is part of the same continuum. According to a recent study, having an ADHD comorbidity was linked to poorer performance on cognitive tasks when compared to ASD alone. Other research showed that having both ASD and ADHD was linked to a worse quality of life, lower adaptive functioning, more anxiety, and greater social interaction deficits. Additionally, a recent study showed that children with comorbid ASD and ADHD have higher externalising problems than ASD alone and lower externalising symptoms than children with ADHD alone in terms of their emotional and behavioural profiles. Similar to this, children with ADHD who exhibited more autistic symptoms had weaker cognitive and social abilities, and the presence of autistic traits predicted a more serious outcome.
Keywords
Functional motion disorders