Circulating androgen levels are not affected by the administration of vaginal micronized progesterone for withdrawal bleeding in patients with polycystic ovary syndrome
2 Biostatistics Unit , Instituto Universitario, Dexeus, Spain, Email: ignacio@dexeus.com
Received: 12-Aug-2017 Accepted Date: Dec 08, 2017; Published: 15-Dec-2017
Citation: Dosouto C, Rodriguez-Purata J, Alvaro B, et al. Circulating androgen levels are not affected by the administration of vaginal micronized progesterone for withdrawal bleeding in patients with polycystic ovary syndrome. J Reprod Biol Endocrinol. 2017;1(2):29-31
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
BACKGROUND: Polycystic ovary syndrome (PCOS) is the most common endocrine disorder in women of reproductive age, with hyperandrogenemia as one of its main components. Several medications have been described to properly induce withdrawal, unfortunately, most of them significantly suppress ovarian function and lower circulating androgen levels with a subsequent diagnosis bias. The present study aims to determine whether the use of vaginal micronized progesterone (VMP) to induce withdrawal bleeding in women with PCOS alters circulating androgen parameters.
METHODS: This is a prospective clinical trial, performed at an academic medical center. Fifteen reproductive-aged women with PCOS were studied. Blood samples were collected at baseline (Sample 1) and between the 3rd-5th day of withdrawal after 7 days of VMP (100 mg every 12 h) (Sample 2). Total testosterone (TT), free androgen index (FAI), sex hormone binding globulin (SHBG), dehydroepiandrosterone sulfate (DHEAS), androstenedione (A4) and 17-hydroxyprogesterone (17-OHP) levels were determined in the blood samples.
RESULTS: All 15 patients fulfilled the Rotterdam criteria for PCOS. Two patients presented spontaneous ovulation confirmed in Sample 1 and were not included in the analysis. Mean age was 29.3 ± 4.9 years and mean body mass index was 26.9 ± 6.7 kg/m2. The mean values of TT, FAI, SHBG, DHEAS, A4 and 17-OHP did not change after VMP administration.
CONCLUSION: Withdrawal bleeding with VMP in PCOS patients does not significantly alter circulating androgen levels compared to baseline and can thus be used to time blood sampling in these patients.
Keywords
Polycystic ovarian syndrome, androgens, progesterone, withdrawal, hyperandrogenism
Abbreviations
PCOS Polycystic ovary syndrome;17-OHP 17-hydroxyprogesterone; MPA Medroxyprogesterone; MP Micronized progesterone; VMP Vaginal micronized progesterone; OMP Oral micronized progesterone; TT Total testosterone; FAI Free androgen index; SHBG Sex hormone-binding globulin; DHEAS Dehydroepiandrosterone sulfate; A4 Androstendione; RIA Radioimmuno assay; FSH Follicle stimulating hormone; LH Luteinizing hormone; E2 Estradiol; BMI Body mass index
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder in women of reproductive age, affecting 7% of the female population [1]. While the etiology of PCOS is complex and not completely understood, the syndrome is characterized by oligo/anovulation with polycystic ovaries and increased androgen secretion resulting in acne and hirsutism [2]. Hormonal evaluation of women who are suspected of having PCOS involves the measurement of basal levels of androgens and 17-hydroxyprogesterone (17-OHP), which are generally used to establish the presence of hyperandrogenemia and exclude other diagnoses with similar clinical signs, as non-classic congenital adrenal hyperplasia [1]. In general, these levels are obtained during the early follicular phase to maintain sampling uniformity and avoid spurious increases due to corpus luteum function. However, because most hyperandrogenic patients are oligo/ amenorrheic, it is frequently necessary to administer a progestogen to induce withdrawal bleeding and properly time the blood sampling.
Several medications have been described to properly induce withdrawal bleeding [3], with medroxyprogesterone acetate (MPA) being the most widely used. However, synthetic compounds as MPA do not replicate precisely the constellation of biologic activities of the parent hormone [4]. Previous reports have suggested that the use of MPA in women with PCOS results in a temporary, albeit clinically relevant, suppression in ovarian function [5] and circulating androgen levels [6,7], in addition to several adverse side effects [3]. All comparative studies to date conclude that the side effects of synthetic progestins can be minimized or eliminated through the use of micronized progesterone (MP) [8-10] and consequently result in reduced hormonal suppression [11].
The putative advantage of using MP over MPA is that the former is bioidentical to the body’s own progesterone produced by the corpus luteum. Recent evidence has shown that MP displays a favorable action on blood vessels and on the brain, which may not be true for some synthetic progestins [12]. Furthermore, MPA, possibly owing to its glucocorticoid activity, may counteract some of the beneficial effects of estradiol, which is not the case with MP. Moreover, there is evidence that synthetic progestins have a teratogenic effect when administered during the first 4 months of pregnancy [10]. Woods et al previously investigated if oral MP used to induce withdrawal bleeding in women suspected of having PCOS alters circulating androgen levels [11]. The authors concluded that the administration of oral MP did not significantly alter circulating androgen or 17-OHP levels, and could be used to time blood sampling in these patients. Nonetheless, it has been previously described the dose, duration, and route of administration are critical to optimization of the treatment regimen [13].
In this study, it is hypothesized that the administration of natural progesterone vaginally, which will avoid hepatic first pass, may result in significantly less hormonal suppression. The authors test this hypothesis by prospectively determining the effect of vaginal MP (VMP) administered for the induction of withdrawal bleeding, on the circulating androgen and 17-OHP levels in women with PCOS.
Methods
Settings and ethics
All patients who came into consult of the doctor in charge of the study and responsible for the Reproductive Endocrinology Unit at Hospital Universitario Dexeus and fulfilled the inclusion criteria, were offered to participate. The study was approved by the Institutional Review Board, and all participants were provided written informed consent.
Study population
We studied women diagnosed with PCOS according the Rotterdam criteria [14]:
1. Chronic ovulatory dysfunction, defined as inter-menstrual intervals of >45 days or a total of <8 menstrual cycles per year;
2. Polycystic ovaries, defined as at least one ovary with >12 follicles between 2 and 9 mm or an ovarian volume >10 mL; and
3. Biochemical or clinical hyperandrogenism. The presence of two of the three criteria would be sufficient for diagnosis.
Patients excluded will constitute:
1. Exclusion of related disorders, such as non-classic congenital adrenal hyperplasia, hyperprolactinemia and thyroid dysfunction;
2. Drugs that could interfere with hormonal data (oral contraceptives or other) taken at least 3 months before the study.
Hormonal analysis
The levels of total testosterone (TT), free androgen index (FAI), sex hormone-binding globulin (SHBG), dehydroepiandrosterone sulfate (DHEAS), androstenedione (A4) and 17-OHP were measured by standard radioimmunoassay (RIA). Follicle stimulating hormone (FSH), luteinizing hormone (LH) and estradiol (E2) levels were also evaluated to assess eventual spontaneous ovulation. The following commercially available kits were used: Gamma Counter Wizard by Perkin Elmer for 17-OHP, A4 and FAI; Beckman Coulter (Access) for DHEAS, TT, SHBG, FSH, LH and E2. The intra-assay coefficient of variation for all steroids did not exceed 6%, except for estradiol, which was 12%.
Collection of samples
All patients were sampled on the day of the first visit at the outpatient clinic (Sample 1). Sample 2 was obtained between the 3rd and 5th day of induced withdrawal. Blood samples 2 were drawn in the morning between 8 and 11 am, after each patient had been fasting for at least 8 h and centrifuged immediately and serum was stored at -80ºC until it was assayed.
All hormonal parameters were compared before and after the administration of 200 mg of VMP (Utrogestan©; Solvay-Pharma, Suresnes, France) (100 mg every 12 h) for a 7 day course.
Statistical analysis
All statistical analyses were performed using the IBM® SPSS® Statistics v22.0 application. Data are expressed as means ± SD. Difference between the two groups was compared by Wilcoxon Rank Test for paired data. When variables were categorized (normal or abnormal) by our reference laboratory, the MacNemar test was used.
Main outcome measures
The main outcome measure was any differences on androgen level before and after VMP administration. As a secondary outcome, we evaluated whether this regimen affects the diagnosis of analytical hyperandrogenism.
Results
A total of fifteen Caucasian reproductive-aged women with PCOS were recruited. All fifteen patients fulfilled the Rotterdam criteria for diagnosis of PCOS. Of these, 13 patients were anovulatory and two patients presented spontaneous ovulation, confirmed by Sample 1 and were not included in the analysis. Ovulation was confirmed by a serum progesterone level >1.5 ng/mL.
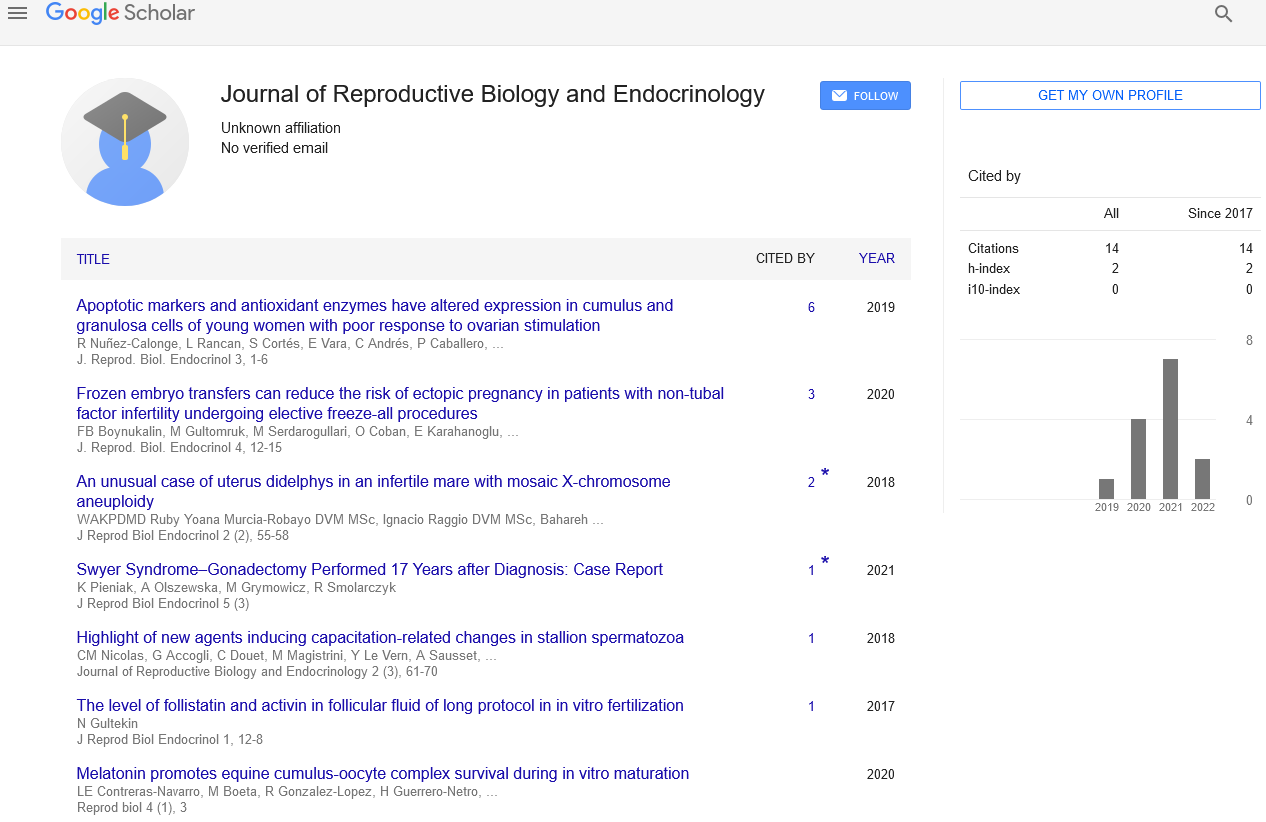
Their mean age was 29.3 ± 4.9 years and mean body mass index (BMI) was 26.9 ± 6.7 Kg/m2. Baseline hormonal characteristics of the patients are given in Table 1.
| Before VMP (n=13) |
After VMP (n=13) |
p Value | Normal value | |
|---|---|---|---|---|
| TT (ng/mL) | 0.6 ± 0.1 | 0.5 ± 0.1 | 0.39 | 0.15-0.7 |
| FAI (%) | 5.2 ± 3.2 | 4.7 ± 2.7 | 0.16 | 0.6-10.6 |
| A4 (ng/mL) | 2.5 ± 1.0 | 2.8 ± 1.3 | 0.53 | 0.4-3.4 |
| DHEAS (mcmol/L) | 2.2 ± 1.9 | 2.3 ± 2.1 | 0.46 | 0.92-11.67 |
| 17-OHP (ng/mL) | 0.6 ± 0.2 | 0.7 ± 0.5 | 0.89 | 0.11-1.8 |
| SHBG (nmol/L) | 52.3 ± 22.2 | 54.3 ± 26.7 | 0.54 | 18-144 |
| FSH (UI/L) | 5.4 ± 1.2 | 5.0 ± 1.6 | 0.40 | 1.4-9.9 |
| LH (UI/L) | 11.8 ± 7.9 | 8.1 ± 4.4 | 0.06 | 1.7-15 |
| TT (ng/mL) | 0.6 ± 0.1 | 0.5 ± 0.1 | 0.39 | 0.15-0.7 |
| FAI (%) | 5.2 ± 3.2 | 4.7 ± 2.7 | 0.16 | 0.6-10.6 |
| A4 (ng/mL) | 2.5 ± 1.0 | 2.8 ± 1.3 | 0.53 | 0.4-3.4 |
| DHEAS (mcmol/L) | 2.2 ± 1.9 | 2.3 ± 2.1 | 0.46 | 0.92-11.67 |
| 17-OHP (ng/mL) | 0.6 ± 0.2 | 0.7 ± 0.5 | 0.89 | 0.11-1.8 |
| SHBG (nmol/L) | 52.3 ± 22.2 | 54.3 ± 26.7 | 0.54 | 18-144 |
| FSH (UI/L) | 5.4 ± 1.2 | 5.0 ± 1.6 | 0.40 | 1.4-9.9 |
TT Total testosterone; FAI Free androgen index; A4 Androstenedione; DHEAS Dehydroepiandrosterone sulfate; 17-OHP 17-hydroxyrogesterone; SHBG Sex-hormone
binding globulin; FSH Follicle stimulating hormone; LH Luteinizing hormone
A Wilcoxon Rank Test for paired data was used to compute the p-value
Table 1: Group differences in hormone values between baseline and after VMP administration
The mean values of TT, FAI, SHBG, DHEAS, A4 and 17-OHP did not change with VMP administration, and neither did the mean values of FSH, LH and E2. There was a tendency to observe lower levels of LH during withdrawal bleeding in comparison with baseline values, albeit without significant differences (Table 1).
There were no significant differences when the diagnosis of analytical hyperandrogenism (normal or abnormal according to our reference laboratory) before and after the VMP regimen was compared (Table 2).
| n | TT1 (ng/mL) | TT2 (ng/mL) | FAI1 (%) | FAI2 (%) | A41 (ng/mL) | A42 (ng/mL) | DHEAS1 (mcmol/L) | DHEAS2 | 17-OHP1 (ng/mL) | 17-OHP2 (ng/mL) |
|---|---|---|---|---|---|---|---|---|---|---|
| (mcmol/L) | ||||||||||
| 1 | 1 | 0.9 | 8.23 | 6.54 | 4.1 | 3.4 | 1.05 | 1.01 | 1.03 | 0.75 |
| 2 | 0.4 | 0.4 | 4.15 | 1.67 | 1.2 | 1.6 | 1.62 | 1.28 | 0.4 | 1.5 |
| 3 | 0.6 | 0.5 | 3.13 | 2.9 | 2.3 | 2.2 | 0.9 | 0.91 | 0.82 | 0.69 |
| 4 | 0.8 | 0.9 | 6 | 4.92 | 4.2 | 5.3 | 2.27 | 6.41 | 1.25 | 2.05 |
| 5 | 0.6 | 0.4 | 2.27 | 1.68 | 2.9 | 1.8 | 1.93 | 1.51 | 0.75 | 0.34 |
| 6 | 0.5 | 0.6 | 4.24 | 4.78 | 2.7 | 5 | 2.43 | 1.75 | 0.7 | 0.99 |
| 7 | 0.7 | 0.6 | 12.28 | 10.79 | 1.8 | 2.9 | 2.4 | 3.35 | 0.36 | 0.46 |
| 8 | 0.4 | 0.5 | 4.48 | 8.27 | 1.5 | 1.4 | 1.71 | 1.48 | 0.53 | 0.35 |
| 9 | 0.5 | 0.9 | 3.13 | 4.66 | 2.3 | 2.1 | 1.34 | 1.62 | 0.85 | 0.76 |
| 10 | 0.4 | 0.5 | 1.67 | 1.61 | 1.9 | 2.1 | 1 | 1.04 | 0.5 | 0.7 |
| 11 | 0.6 | 0.4 | 3.44 | 2.66 | 2.4 | 2.4 | 2.49 | 2.37 | 0.93 | 0.31 |
| 12 | 0.7 | 0.4 | 11.52 | 4.93 | 3.2 | 1.9 | 0.87 | 0.77 | 0.73 | 0.2 |
| 13 | 0.8 | 0.5 | 6.27 | 5.85 | 3.3 | 4.7 | 8.98 | 7.3 | 0.46 | 0.48 |
Individual values for each patient before (1) and after (2) VMP administration. Abnormal values are highlighted in bold
TT Total testosterone; FAI Free androgen index; A4 Androstenedione; DHEAS Dehydroepiandrosterone sulfate; 17-OHP 17-hydroxyrogesterone
Table 2: Individual values for each patient before (1) and after (2) VMP administration. Abnormal values are highlighted in bold
Discussion
The clinical value of these studies is to help with the diagnosis of PCO, ensure withdraw and better programming of blood hormonal tests.
The data from the present study indicate that in women with anovulatory PCOS, androgen hormonal profile (TT, FAI, SHBG, DHEAS, A4) and 17- OHP did not significantly differ at baseline and after VMP administration.
The induction of withdrawal bleeding with progestins has been considered a common procedure in several studies to compare hormonal values in follicular phase among patients with PCOS. The reported data on this topic is poor, unclear, with a small number of patients assessed, and they are not homogeneous in regard to PCOS Rotterdam criteria. In many cases, withdrawal is performed with different kinds of progestins (Depot Acetate Medroxyprogesterone or oral Micronized Progesterone), rendering it incomparable [11,15].
However, the usefulness of this test requires further investigation in PCOS, as the available data are reported with MPA [5-7,11,16-21] or oral MP and for a not well-established period of time [22]. Previous studies [5-7,16], have shown that progesterone administration could suppress pituitary LH secretion, ovarian function and androgen synthesis, suggesting that this could be a diagnostic bias [17].
We used vaginal administration for several reasons. On the one hand, this form of ad-ministration could cause fewer metabolic changes by avoiding hepatic first pass [15,23]. In addition, it offers better tolerance [24], excellent absorption very close to the target organ; it avoids oral administration and is the alternative preferred by patients [23].
The progestin used in the present study (Utrogestan©) was synthesized from a precursor extracted from yams (Dioscorea sp.) and is chemically identical to ovarian progesterone [25,26]. Its micronized formulation reportedly provides optimal progesterone bioavailability after vaginal administration, reaching its maximum level after 2 to 6 h and returning to baseline values within 24 h after the last dose. One dose every 12 h ensures the least variation between individuals [27]. Thus, in our opinion, it could be an optimal regimen for the diagnostic assessment in PCOS patients, being useful to induce withdrawal bleeding without significantly changing circulating androgen levels. The fact that every patient is their own control is a strong point of the study, although our results should be taken with caution due to the small sample size and the low statistical power of the tests.
In terms of limitations, the present study only provides information about 13 patients. Measuring sex hormones on two alternate days throughout a whole menstrual cycle is demanding on the subject and expensive, and it is for such reasons that our study was limited to an initial number of 15 subjects.
Conclusion
In conclusion, withdrawal bleeding with VMP with this regimen (7 days of 100 mg every 12 h vaginal) does not significantly alter circulating androgen levels compared to baseline and can be used to time blood sampling in these patients.
This protocol optimizes schedules in daily clinical practice and offers an easier diagnostic process and clinical management without changing androgen levels.
Acknowledgement
Under the auspices of the Càtedra d’ Investigació en Obstetrícia i Ginecologia de la Universitat Autònoma de Barcelona. Authors would like to thank Dr. Rosa Tur and Dr. Fulvia Mancini for their contributions to the initial design of the study.
REFERENCES
- Azziz R. The time has come to simplify the evaluation of the hirsute patient. Fertil Steril. 2000;74(5):870-72.
- Azziz R, Carmina E, Dewailly D, et al. Positions statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: An androgen excess society guideline. J Clin Endocrinol Metab. 2006;91(11):4237-45.
- Battino S, Ben-Ami M, Geslevich Y, et al. Factors associated with withdrawal bleeding after administration of oral dydrogesterone or medroxyprogesterone acetate in women with secondary amenorrhea. Gynecol Obstetr Investig. 1996;(42):113-6.
- Bullock LP, Bardin CW. Androgenic, synandrogenic and anti-androgenic actions of progestins. Ann N Y Acad Sci. 1977;(286):321-30.
- Taylor AE. McCourt B, Martin KA, et al. Determinants of abnormal gonadotropin secretion in clinically defined women with polycystic ovary syndrome. J Clin Endocrinol Metab. 1997;82(7):2248-56.
- Anttila L, Koskinen P, Erkkola R, et al. Serum androgen and gonadotropin levels decline after progestogen-induced withdrawal bleeding in oligomenorrheic women with or without polycystic ovaries. Fertil Steril. 1992;58(4):697-702.
- Anttila L, Koskinen P, Kaihola HL, et al. Serum testosterone, androstenedione and luteinizing hormone levels after short-term medroxyprogesterone acetate treatment in women with polycystic ovarian disease. Acta Obstet Gynecol Scand. 1994;73(8):634-36.
- Hitchcock CL, Prior JC. Oral micronized progesterone for vasomotor symptoms - A placebo-controlled randomized trial in healthy postmenopausal women. Menopause. 2012;19(8):886-93.
- de Lignières B. Oral micronized progesterone. Clin Ther. 1999;21(1):41-60-62.
- Fitzpatrick LA, Good A. Micronized progesterone: Clinical indications and comparison with current treatments. Fertil Steril. 1999;72(3):389-97.
- Woods KS, Reyna R, Azziz R. Effect of oral micronized progesterone on androgen levels in women with polycystic ovary syndrome. Fertil Steril. 2002;77(6):1125-7.
- L'hermite M, Simoncini T, Fuller S, et al. Could transdermal estradiol + progesterone be a safer postmenopausal HRT? A review. Maturitas. 2008;60(3-4):185-201.
- Shangold MM, Tomai TP, Cook JD, et al. Factors associated with withdrawal bleeding after administration of oral micronized progesterone in women with secondary amenorrhea. Fertil Steril.1991;56(6):1040-7.
- Group, R.E.A.-S.P.C.W. Revised consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19-25.
- Livadas S, Boutzios G, Economou F, et al. The effect of oral micronized progesterone on hormonal and metabolic parameters in anovulatory patients with polycystic ovary syndrome. Fertil Steril. 2010;94(1):242-26.
- Christman GM, Randolph JF, Kelch RP, et al. Reduction of gonadotropin-releasing hormone pulse frequency is associated with subsequent selective follicle-stimulating hormone secretion in women with polycystic ovarian disease. J Clin Endocrinol Metab. 1991;72(6):1278-85.
- Sánchez LA, Pérez M, Centeno I, David M, et al. Determining the time androgens and sex hormone-binding globulin take to return to baseline after discontinuation of oral contraceptives in women with polycystic ovary syndrome: a prospective study. Fertil Steril. 2007;87(3):712-14.
- Kawadski JK, Dunaif A. Diagnostic criteria for polycystic ovarian syndrome: toward a rational approach. In: Dunaif A, Givens JR, Haseltine FP, Merriam GR, editors. Polycystic ovarian syndrome. Boston: Blackwell Scientific Publications. 1992.377-84.
- Chhabra S, McCartney CR, Yoo RY, et al. Progesterone inhibition of the hypothalamic gonadotropin-releasing hormone pulse generator: Evidence for varied effects in hyperandrogenemic adolescent girls. J Clin Endocrinol Metab. 2005;90(5):2810-5.
- Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: Insulin resistance and b-cell function from fasting plasma glucose and insulin concentration in man. Diabetologia. 1985;412-9.
- Fiad TM, Cunningham SK, McKenna TJ. Role of progesterone deficiency in the development of luteinizing hormone and androgen abnormalities in polycystic ovary syndrome. Eur J Endocrinol. 1996;135(3):335-9.
- Bagis T, Gokcel A, Zeyneloglu HB, et al. The effects of short-term medroxyprogesterone acetate and micronized progesterone on glucose metabolism and lipid profiles in patients with polycystic ovary syndrome: a prospective randomized study. J Clin Endocrinol Metab. 2002;87(10):4536-40.
- Ballagh SA. Vaginal rings for menopausal symptom relief. Drugs Aging. 2004;21(12):757-66.
- Novák A, de la Loge C, Abetz L, et al. The combined contraceptive vaginal ring, NuvaRing: An international study of user acceptability. Contraception. 2003;67(3):187-94.
- McAuley JW, Kroboth FJ, Froboth PD. Oral administration of micronized progesterone: A review and more experience. Pharmacotherapy. 1996;16(3):453-7.
- Maxson WS, Hargrove JT. Bioavailability of oral micronized progesterone. Fertil Steril. 1985;44(5):622-6.
- Erny R, Simoncini C, Chastellière N, et al. Variation in plasma progesterone induced by the vaginal administration of Utrogestan. J Gynecol Obstet Biol Reprod. 1989;18(2):229-34.