Classical open aorto-bi-femoral grafting is a gold standard technique in aorto-iliac occlusive disease: The technique of double layered reinforcing aorto-graft proximal anastomosis with anterior augmentation patchplasty and its advantages
Received: 29-Jun-2018 Accepted Date: Jul 13, 2018; Published: 20-Jul-2018
Citation: Haridas AK, Bhat BS. Classical open aorto-bi-femoral grafting is a gold standard technique in aorto-iliac occlusive disease: The technique of double layered reinforcing aorto-graft proximal anastomosis with anterior augmentation patchplasty and its advantages. J Vas Dis Treat. 2018;2(2):7-13.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Incidence of peripheral vascular disease has increased worldwide. It is associated with significant morbidity and mortality. Infra renal aorto-iliac occlusive disease is the commonest subset. This subset can be associated with or without distal vessels involvement. It is critical to manage such cases earliest, to salvage the limbs and to avoid the mortality. Classical open aorto bi femoral grafting is the gold standard technique. Endovascular stenting has been slowly but steadily, accepted in selective cases of AIOD. Less heard laparoscopic and robotic assisted surgery, practised in a small series of cases but they are yet to prove themselves. Proximal anastomotic technique is varied with surgeons. Individual techniques have their own merits and demerits.
Objective: To study the patients presenting with aorto-iliac occlusive disease and their outcome after open aorto bi femoral grafting using proximal, side to end double layered reinforced aorto-graft anastomosis with anterior augmentation patchplasty. We reviewed and compared our technique with other contemporary techniques available for AOID.
Method: We did a retrospective study of patients from December 2014 to December 2017 suffering from aorto-iliac occlusive disease and outcome of open aorto bi femoral grafting using proximal, side to end double layered reinforced aorto-graft anastomosis with patchplasty technique. Case history was reviewed in detail about the nature of group and way of their presentations. Computed tomograms, coronary angiograms of peripheral and coronary vessels were evaluated to study pattern of disease along with associated distal vessels involvement. All patients underwent classical open aorto bi femoral grafting using the technique of proximal, side to end double layered reinforced aorto-graft anastomosis with anterior augmentation patchplasty with or with distal bypass. Post-op outcome, complications and patency of graft was evaluated over the period of 3 years.
Result: The majority of the patients were less than 60 years with the male predominance. Smoking was strongly associated co morbid condition. Smokers had bad non graft able vessels requiring more grafts. Delayed presentation with pre-gangrene or gangrene had an increased incidence of morbidity and mortality. Technique of open aorto Bi femoral grafting using proximal, side to end double layered reinforced aorto-graft anastomosis with anterior augmentation patchplasty is superior in reducing post-op complication and it allows graft to stay parallel to native vessels so, avoids the distortion or kinking of the graft. Dacron graft had the higher incidence of early and late graft occlusion and needed redo surgery.
Conclusion: Infrarenal aorto occlusive disease is second commonest subset of peripheral vascular disease. Classical open aorto bi femoral grafting is the gold standard technique. Laparoscopic and endovascular surgeries are suitable in very selective patients. Technique of open aorto bi femoral grafting using proximal, side to end double layered reinforced aorto-graft anastomosis with anterior augmentation patchplasty is superior in reducing complications and increasing greater patency rate. PTFE graft has the better long-term patency rate. The incidence of the redo surgeries were higher with Dacron grafts compared to PTFE grafts.
Keywords
Vascular disease; Coronary artery; Smoking; Thrombosis; Embolism; Graft
Introduction
Aorto-iliac occlusive disease is an important cause of lower extremity ischemic symptoms [1]. Peripheral arterial disease (PAD) is a complex disease and highly prevalent among the smokers. Aorto-iliac occlusive disease is a second most common subset of peripheral arterial disease next to infra inguinal femoral artery disease involving an atheromatous occlusion of the infrarenal aorta, common iliac arteries, or both. Patients commonly present with intermittent claudication, rest pain, critical limb ischemia with or without gangrene. The leriche syndrome is rarely seen in the triad of symptoms, claudication, impotence, and decreased peripheral pulses in male patients. Peripheral vascular disease is a systemic disease and it is not unusual to see associated coronary artery disease [2].
The commonest underlying pathology is atherosclerosis. Its progression is enhanced either because of co-morbid conditions like diabetes, hypertension, hyperhomocysteinaemia, dyslipidemia or chronic smoking [3]. It is also associated with inflammatory disorders like Takayasus arteritis, Buerger’s disease and rarely pelvic radiation.
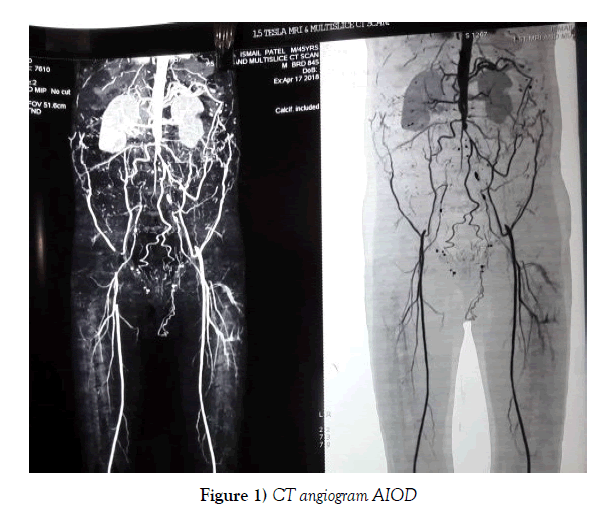
CT angiogram is the best non-invasive diagnostic test to delineate the peripheral vascular system and the lesions to plan the surgical approach. Coronary angiogram is needed in the patient presenting with the cardiac symptoms.
Patients with peripheral vascular disease (PAD) may be associated with coronary artery disease (CAD). Patients with both PAD and CAD, require surgery in the form of aorto bi femoral graft (ABFG) and coronary artery bypass graft (CABG), which needs to be prioritized as per severity of disease. In a small group of patients, it is imperative to operative both PAD and CAD together. The surgical approach in such cases is varied. It can be staged or concurrent, anatomical or extra anatomical ABFG with CABG and priority order of ABFG as well as CABG has to be decided as per symptoms of individual patient [4,5].
It is standard to use a single layer proximal aorto-graft anastomosis. This is one of the commonest causes of post-operative bleeding from anastomotic site, hence increases the post-operative morbities. The favoured, end to end proximal aorto-graft anastomosis, gives most hemodynamic flow due to position of graft parallel to native vessel which is deficient in end-to-side anastomosis. In the absence of patch plasty or anterior augmentation in a side to end anastomosis, it is difficult to lay distal graft without kinking or distortion. It is specially while rerouting of graft limbs to infra inguinal area for distal grafting. It could be the reason for the high rate of graft occlusion and increased need for reintervention in end to side aorto-graft anastomotic technique [6].
It is the technique of anastomosis, type of graft and the number of distal graft that dictates the patency of the bypass graft. It is found that risk factor modification by treating hypertension, dyslipidemia, diabetes, cessation of smoking and regular exercise controls the progression of atherosclerosis which in turn helps to improve patency of bypass graft longer than expected [7,8].
Materials and Methods
Material
It is a retrospective study. Patients with aorto-iliac occlusive disease, who subsequently underwent open aorto bi femoral grafting using proximal, side to end double layered reinforced aorto-graft anastomosis with anterior augmentation patchplasty were considered for the study. Case history, investigation report (Figure 1), operating findings and procedure were evaluated in details. Post-operative complications, morbidities and mortality were assessed.
Method
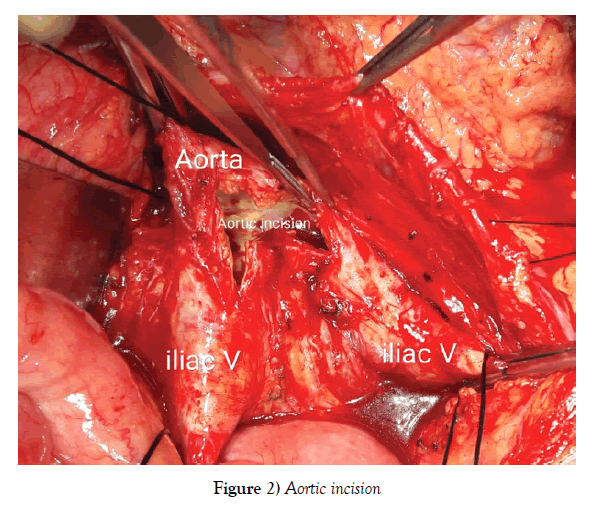
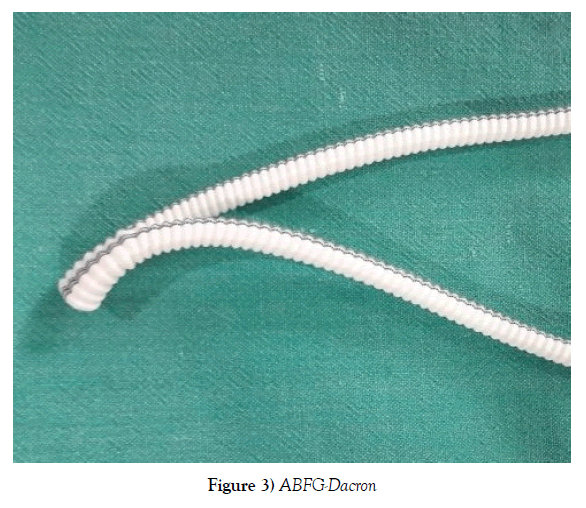
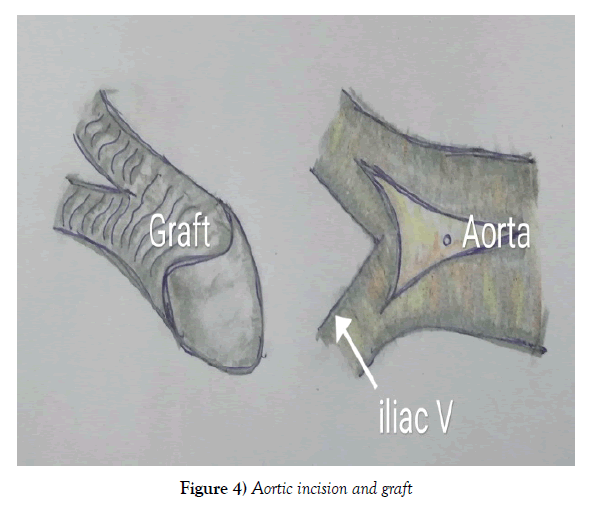
Cases were operated in the supine position under general anaesthesia. The mid line abdominal incision was taken and transperitoneal aorta was approached. The supra or infrarenal aorta and bilateral iliac vessels were exposed and looped. Bilateral infra inguinal femoral artery was exposed. Inj Heparin 100 units per kg, is given, before clamping the vessels. Bifurcating Grafts made of either PTFE or Dacron were used for the procedures. Aorta at the level of bifurcation was opened involving 2/3rd distal aorta and 1/3rd proximal iliac vessels. The 5 to 6 cm of proximal graft was kept before bifurcation and the graft ends were beveled (Figures 2-4).
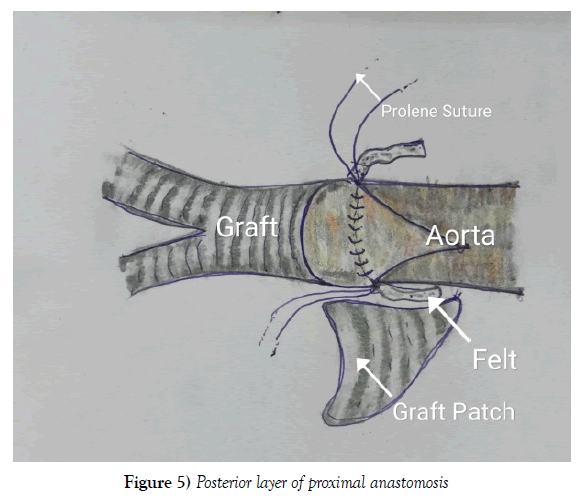
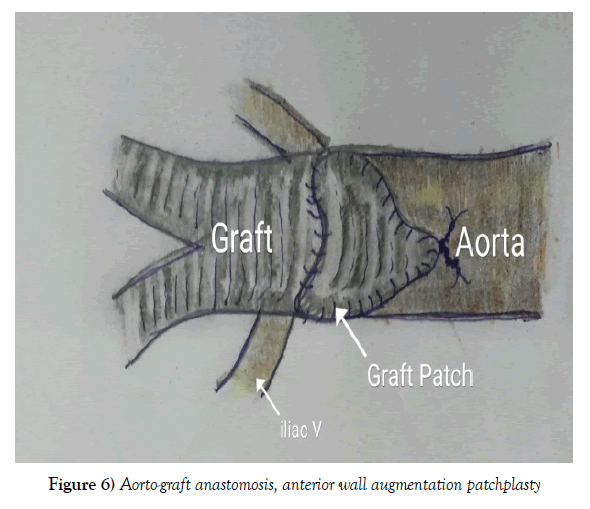
Proximal aorto-graft anastomosis in side to end fashion was done in two layers reinforced with PTFE felt. First layer with 4-0 polypropylene and the second layer of reinforcing stitch using 3-0 polypropylene for leak proof anastomosis. Once posterior suture line was done, anterior gap between graft and aortic opening, was measured. A triangular patch of a graft was taken (Figures 5 and 6). The anterior gap was augmented with patch and sutured (Figure 6).
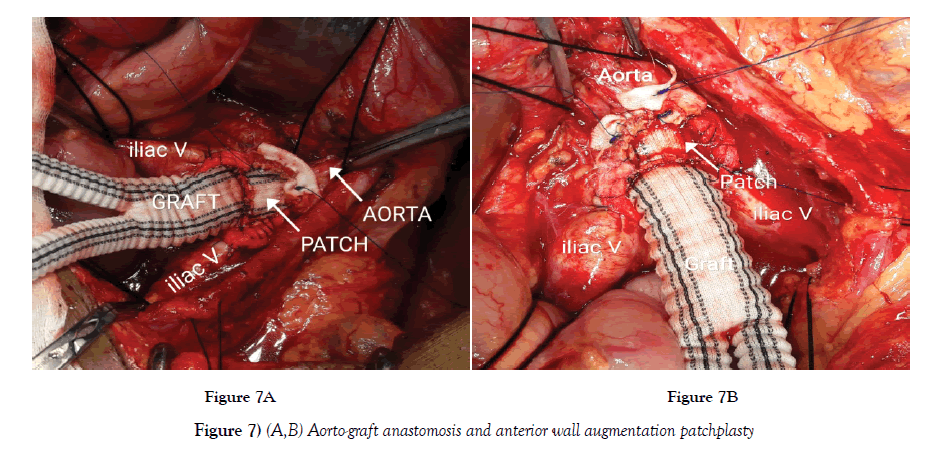
The anterior augmentation patchplasty allows graft to stay close and parallel to native vessels (Figure 7A and B). This prevents likely chance of kinking or distortion of graft limbs. The hemodynamic blood flow would be like seen in end-to-end anastomosis, as graft stayed in line with the native vessels.
The distal grafting to femoral area was done, after proximal anastomosis. It allows better exposure for primary anastomosis and it is easy to handle suture bleeding from posterior layer after release of proximal vascular clamp. Left and right graft limbs were routed to femoral area in their shortest distance. Distal anastomosis to femoral artery was done, Using 5-0 or 6-0 polypropylene, based on quality of vessel wall (Figure 8). Profundaplasty was contemplated only if it was involved in the disease.
Distal bypass for femoro- popliteal artery and infra popliteal arteries were done, using either reversed saphenous or 6 mm PTFE graft. In localised stenosis, endarterectomy followed by patch plasty was done, using PTFE patch. In selected cases, concomitant CABG and ABFG had to be done. First the CABG, followed by the anatomical ABFG surgery was done in the same sitting.
Results
Total n=150 patients studied retrospectively, who had undergone aorto-bi- femoral grafting with special technique of proximal aorto-graft, side to end double layered reinforced anastomosis with anterior wall augmentation using patchplasty.
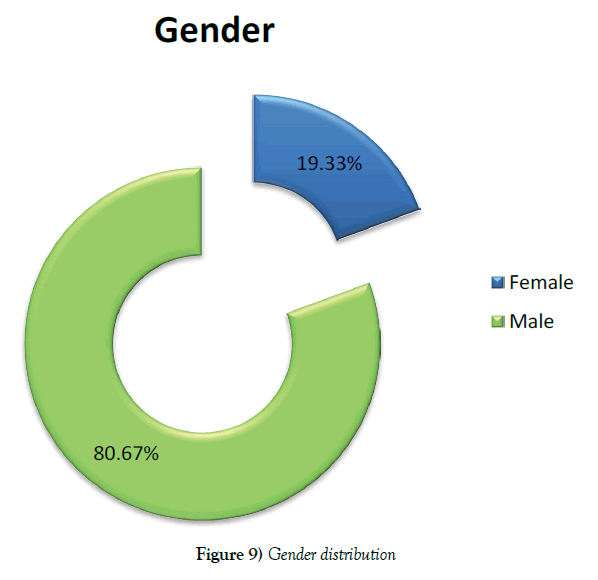
Study involved predominantly 121 male (80.67%) and 29 female (19.33%) patients (Figure 9).
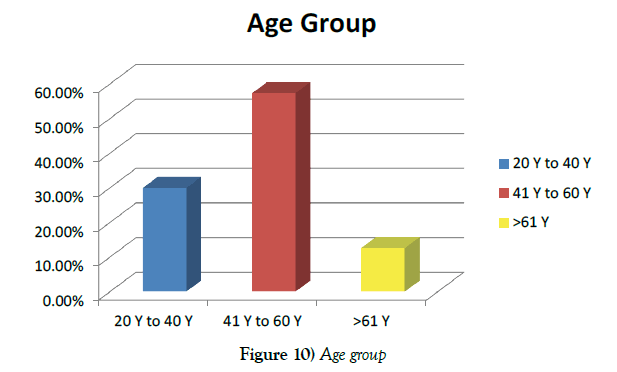
Among the study group, Forty-five patients were between 20 to 40 years (30%), eighty-six patients were between 41 to 60 years (57.33%) and nineteen patients were above 61 years (12.67%) (Figure 10).
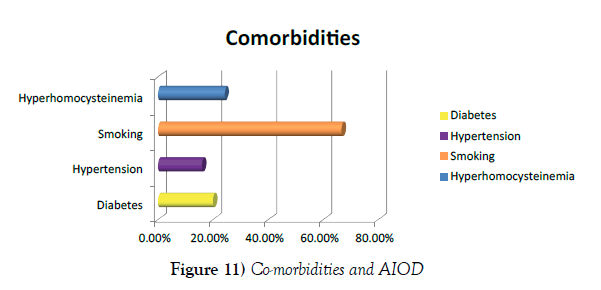
Among co morbities, 100 patients were chronic smokers (66.67%), 36 had hyperhomocysteinaemia (24%), 30 patients were diabetics (20%) and 24 patients were hypertensive (16%) (Figure 11).
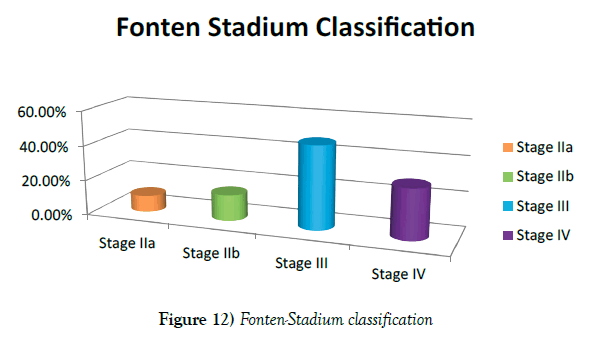
Based on Fonten stadium classification, Fourteen (9.33%) patients had claudication discomfort (Fonten stadium IIa), 22 (14.67%) disabling claudication discomfort (Fonten stadium IIb), 71 (47.33%) rest pain (Fonten stadium III), and 43 (28.67%) gangrene (Fonten stadium IV) (Figure 12).
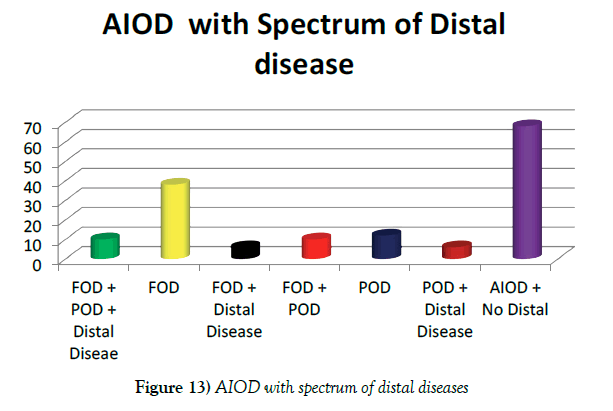
Isolated aortoiliac occlusive diseases with intact femoro-popliteal segment (Type I) were found in 68 (45.33%) patients, combined aorto-iliac and superficial femoral artery disease (Type II) in 38 (25.33%) patients, combined aorto-iliac and femoro-popliteal diseases (Type III) in 22 (14.67%) and combined aorto-iliac, femoro-popliteal and distal disease (Type IV) in 22(14.67) patients (Figure 13).
Among Twenty-seven coronary artery diseases (18%) patients associated with aorto-iliac occlusive disease, sixteen patients had concurrent ABFG and CABG (10.67%) surgeries in this series.
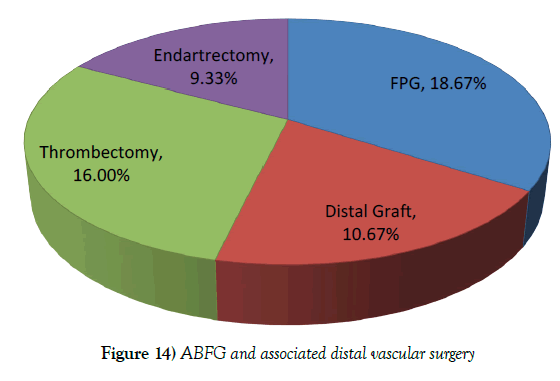
Total 150 aorto-bi- femoral grafting (100%), 28 femoro-popliteal grafting (18.67%), 16 distal infra popliteal grafting (16%), 24 thrombectomy (16%), 14 endarterectomy with patchplasty (9.33%) and nine major amputations (6%) done (Figure 14).
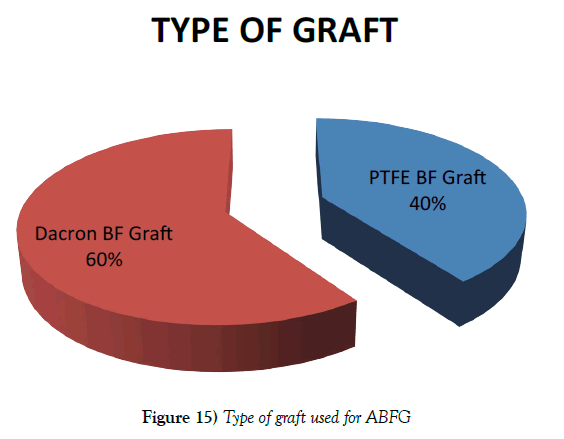
Out of 150 ABFG surgery, in 60 patients PTFE grafts (40%) and in 90 patients Dacron grafts (60%) were used (Figure 15).
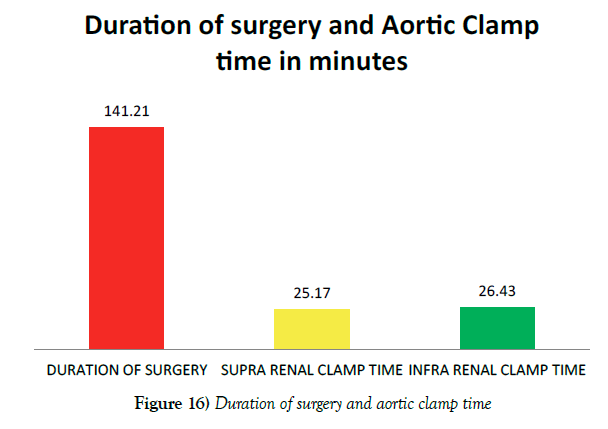
Mean duration of surgery was 141.21 minutes (SD-20.060). The Suprarenal mean clamp time was 25.17(SD-14.520) minutes and infer renal mean clamp time was 26.43(SD-16.580) minutes. In view of the critical renal ischemic time, proximal anastomosis was done in a faster pace in the suprarenal clamped patients compared to the infrarenal clamp patients during ABFG surgery (Figure 16).
Figure 16) Duration of surgery and aortic clamp time
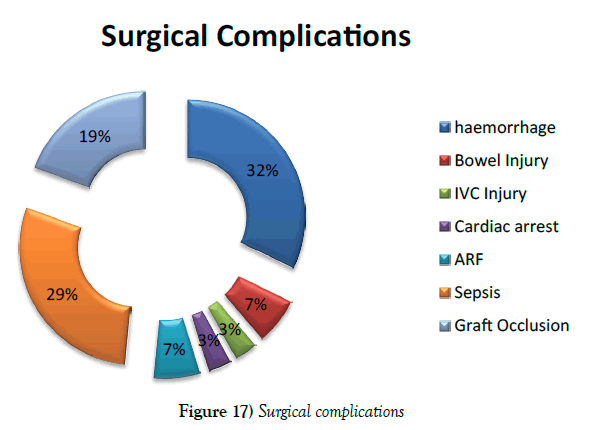
Post operatively, mean of 47.29 ml blood loss from abdominal drainage tube. The ten patients had drainage more than 100 ml and highest blood loss was 210 ml. Very few to mention, complication occurred and majority of them managed conservatively. Immediate Complication like, ten had bleeding (6.67%), two had bowel injury (1.33%), one had inferior vena cava injury (0.67%) and six had graft occlusion (4%). Out of six grafts occlusion, one had PTFE graft and remaining 5 had Dacron grafts. Bowel and IVC injury repaired on table and post operative recovery uneventful (Figure 17).
Majority of bleeding managed conservatively. One patient had to be reexplored for bleeding and extra suture taken on proximal anastomosis. Six patients underwent embolectomy (15.38%) for immediate post operative graft occlusions. The mean hospital stay was 7.87 days (SD-1.830).
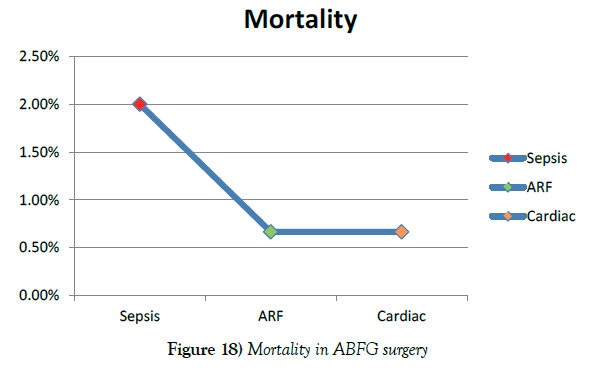
In this series, we lost 5 patients due to sepses in three (2%), acute renal failure in one (0.67%) and cardiac arrest in one (0.67%) within 30 days of post operative period. There were no late deaths (Figure 18).
Over a period of 3 years follow up, ten patients had ABFG occlusion. Out of which two patients were with PTFE grafts and eight with Dacron grafts. In PTFE graft group blood flow established with mere thromboembolectomy using Fogarty arterial and Fogarty graft embolectomy catheter. Out of eight patients in Dacron graft group, two patients’ blood flows re-established with thromboembolectomy but remaining six patients needed re do ABFG surgery using PTFE graft. Post operative period uneventful.
Discussion
Incidence of peripheral vascular disease (PAD) have increased due to increased co morbities and smoking among general population. Majority have a multilevel localization of atherosclerotic diseases. More than half of aorto-iliac occlusive diseases are associated with distal lesions in femoral, popliteal and much smaller distal vessels, requiring simultaneous intervention [9]. Majority of PAD present in the advanced stage. Surgical revascularization for lower limb ischemia remains an important component for optimization of quality of life and symptoms in patients with peripheral arterial disease. It is challenging to choose a right form of surgery to salvage the limbs and the life.
Aorto-femoral bypass (AFB), ilio-femoral bypass (IFB), and aortoiliac endarterectomy (AIE) are the three most common techniques for anatomical surgical revascularisation for patients with aorto-iliac occlusive disease (AIOD). Commonest being aorto bi femoral graft (ABFG) surgery. Ilio-femoral bypass is easy to do but long-term patency is dismal. Endarterectomy and patch plasty is used in localised selected lesions with reasonable acceptable results [10].
The gold-standard treatment for AIOD disease is aorto bi femoral bypass surgery, according to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) study [11]. This procedure has been performed for many years with good long-term results [12]. Classical open ABFG is commonest technique used by most surgeons, worldwide to treat aorto-iliac disease. It gives, ease of access to aorta, ease of anastomosis with able to control complications and the good long term graft patency. No other technique is proved better than open technique which can be used universally to treat AIOD patient. The long-term patency rate is 85%-90% at 5 years and 75%-80% at 10 years. It is best among the interventions for an aorto-iliac occlusive disease.
It is very rare to come across major complications while doing open ABFG. Immediate complications in ABFG are vascular damage, bleeding, intestinal damage, ileus, myocardial infarction and renal failure. Late complications are aorto-enteric fistula, sexual dysfunction, infection, graft thrombosis and anastomotic pseudo-aneurysm [13].
Minimally invasive surgeries, such as laparoscopic and robotic assisted ABFG surgeries are done. They have been studied in a small group of patients, with an ambiguous outcome. Such procedures are case selective. Endovascular intervention is a well accepted alternative modality for AIOD worldwide. Extra-anatomic bypass for AIOD is considered if above options are not feasible. In fact, direct anatomic aortic reconstruction, catheter based endovascular and extra anatomic graft chosen diligently as per patient unique anatomic and risk characteristics [14].
Classical open technique of ABFG, most widely used but controversy exists over which is best. Open techniques is being accepted lesser and lesser in the era of a minimal incision but an argument about long term outcome of low risk extra anatomic repair and endovascular intervention is yet to be answered satisfactorily. Each approach has a selective role to play in the overall management of aortoiliac occlusive disease if applied in appropriate settings. Majority of them are chosen as per location, and severity of the disease [15].
Endovascular stenting is widely accepted worldwide is selected patients. Its primary patency rate is poor. Rate of reintervention and cost of procedure is high [16]. Femoro-femoro jump graft possesses superior long-term durability and patency when implemented in combination with aorto-uni-iliac stent grafts and does not seem to compromise the endpoint success of endovascular treatment [17,18].
The technical success rate was significantly lower in the Aorto iliac stent group, 83% than 100% in the surgery group. The primary 1, 3, and 5 year patency rates were 93.6%, 90.2%, and 90.2%, respectively, in the surgery group, compared to 91.4%, 81.8%, and 64.2%, respectively, in the endovascular stent group. No differences were observed in survival rate, limb salvage, or secondary patency. Endovascular intervention success rate claimed to be high but it has its own complications. The most common complications are migration of stent, parastent leak, adjacent vascular occlusion, peudoaneurysm, arterial dissection and rupture, wire access site hematomas, distal embolization, and iliac artery ruptures. The complications were most often treated conservatively or using percutaneous techniques. Endovascular stent appear to be a safe, minimally invasive, and reliable procedure for patients with chronic infrarenal aortoiliac occlusion in selected patients with or without surgery [19]. Open ABFG surgery is still the first choice for the patients who can endure the surgery. Endovascular treatment is an option for patients with high risk [20]. Compared with ABFG, endovascular stenting is associated with decreased primary patency, decreased perioperative morbidity, and shorter hospital stay [21,22].
Endovascular intervention opened a path for minimal invasive surgery. Minimal incision aortic surgery (MIAS), total laparoscopic, laparoscopic-assisted, and laparobotic techniques have been used to treat AIOD. Totally laparoscopic aorto-bi-femoral bypass is a safe alternative to open surgery in selected patients, with excellent long-term patency rates, albeit at the cost of a steep learning curve [23,24].
Laparoscopic abdominal aortic surgery is feasible and may offer good postoperative recovery with excellent mid-term patency with a shorter hospital stay. A steep learning curve is needed. For these reasons laparoscopic video-assisted technique can be considered a third means of treating severe occlusive and aortic aneurysm. Role of its usage in all procedure is not advocated [25]. Whatever the minimal approach, the aorto-prosthetic graft anastomosis is a major difficulty making those techniques unpopular despite obvious advantages for the patients [26].
Major shortcomings of laparoscopic aortic surgery are the long operating times and the steep learning curve required for these procedures. The mean operating time was 250 minutes, including an aortic cross-clamp time of 40 to 120 minutes. Hand-assisted laparoscopy is a minimally invasive technique with operating times and outcomes similar to those of conventional procedures [27]. However, in spite of the many technical improvements that have already been made, totally laparoscopic and even laparoscopically assisted aortic surgery remains technically demanding [28]. They are accepted options but indicated only in minuscule cases of AIOD. Laparoscopy failed to gain acceptance in the vascular surgery community due to intrinsic procedural challenges and complications worldwide. Minimal incision aorto bi femoral graft and endovascular intervention might provide a mortality and morbidity benefit in higher risk patients with acceptable short- and long-term outcomes [29].
Anatomical repair is straightforward and widely accepted. In certain special situation nonanatomical repair is accepted if patient is critically ill and unable to tolerate open technique or anatomy is not suitable for endovascular intervention. Ring-reinforced, 8-mm expanded polytetrafluoroethylene grafts or plain Dacron grafts are used but long-term benefits are dismissal [30]. Axillo-femoral bypass is a hemodynamically inferior reconstruction that should be performed only in high-risk patients, considered in hostile abdomen and short life expectancy of life [31,32].
There are two types of bifurcated synthetic grafts available for ABFG surgery. Dacron and polytetrafluoroethylene (PTFE) grafts. In many papers these grafts were compared in aorto-bi-femoral position. Karner and Lord, found no significant difference between them after aorto-bi-femoral reconstructions. Paaske et al. wrote about a new stretch bifurcated PTFE graft in aorto-bi-femoral position. Comparing this material with standard Dacron graft, he only found a shorter operating time [33].
The type of graft material and technique of anastomosis of graft, have an impact on long-term patency of graft. PTFE bifurcating graft is most suited and reliable graft with least chance of immediate reintervention. Its suture line bleeding is worrisome and graft is expensive compared to Dacron graft. Dacron Bifurcating graft is easily available, cheap and has no suture hole bleeding. Dacron graft wall leaks on stretching and has a high rate of thrombosis if adequate activated clotting time (ACT) is not maintained during immediate post-op period. Incidence of immediate and late thrombosis is high with Dacron graft needing immediate embolectomy and late redo bypass. The Dacron graft thrombosis is very high, particularly in those patients who stop oral anticoagulation. Significant number of patients with Dacron graft had to undergo redo surgery either in the form of thrombectomy or redo fresh aorto-bi-femoral grafting.
The proximal aorto-graft anastomosis can be done either end to end or side to end anastomosis. Studies have shown, side to end anastomosis has a higher incidence of immediate and late graft occlusion compared to end to end anastomosis [7].
In our technique, all proximal anastomosis were side to end anastomosis with anterior wall augmentation using patchplasty. Proximal body segment of bifurcation graft should be as small as possible but adequate enough to do proximal graft anastomosis. Anterior wall augmented with the triangular patch, keeps graft parallel to the native aorta, which avoids deforming or kinking of graft limbs. This could be the reason for natural hemodynamic flow of blood like seen in an end to end anastomosis leading to longterm patency of our grafts as that of end-to-end anastomosis. Side to end anastomosis reduces the suture edge bleeding. If bleeds occurs, it is easy to control compared to end to end anastomosis. Transabdominal rerouting of bifurcating limb, to infra-inguinal femoral vessels, should be in shortest distance. The rerouting of left graft limb directly, instead of taking through sigmoid colon mesentery, gives better lie of graft. It avoids likely chance of a kink or deformity [7].
Although primary patency was similar between grafts, secondary patencies were better with Dacron at 10 years. Dacron prosthetic grafts are superior to PTFE grafts in above-knee femoro-popliteal arterial bypass procedures [34]. In our study results were otherwise. We found PTFE graft patency is better than Dacron. Incidence of Graft occlusion and redo surgery was high with Dacron grafts. Location of distal anastomosis on femoral artery dictates graft patency. The reasons for the early graft occlusions are stenosis of distal anatomises and poor run off due to distal diffuse disease. The reasons for late graft occlusion are abnormal hemodynamic blood flow, proximal and distal progression of atherosclerotic diseases, distal anastomotic stenosis, and anastomotic neointimal hyperplasia [4,35].
Conclusion
Aorto-iliac occlusive disease is commonest subset among the PAD. It is known to associate with co morbid condition like diabetes, hypertension and coronary artery disease. Chronic smoking is a strong risk factor for a younger group PAD. The smoking hastens the pathophysiology of underlying atherosclerosis and peculiarly involves vasculature diffusely with poor graftable targets.
The aorto-iliac occlusive disease is associated with coronary artery disease, staged procedure is found to have better outcome with the lesser morbidity and mortality
Classical open technique of open aorto bi femoral grafting using proximal, side to end double layered reinforced aorto-graft anastomosis with anterior wall augmentation patchplasty is superior in reducing post op complications and improves greater graft patency rate. It prevent graft deformity in turn improves, distal natural hemodynamic blood flow like found in, end to end anastomosis and so in turn reduces the incidence of immediate and late graft occlusion.
Nature and make of graft does make the difference in outcome of long-term patency. Dacron grafts showed the high rate of occlusion requiring redo surgery.
Diffuse diseases with poor targets, needing higher number of bypass, subsequently have the higher incidence of reintervention and increased morbidities.
Stringent oral anticoagulation, anti platelate drugs and modification of risk factors gives best long term graft patency and symptom free life.
Minimally invasive and Endovascular stent have worthy role in selected patients, in spite higher cost and steep learning curve.
REFERENCES
- Sanchez LA, Wain RA, Veith FJ, et al. Endovascular grafting for aortoiliac occlusive disease. Semin Vasc Surg. 1997;10(4):297-309.
- Wooten C, Hayat M, du Plessis M, et al. Anatomical significance in aortoiliac occlusive disease. Clin Anat. 2014;27(8):1264-74.
- Haridas AK, Bhat BS. Relationship between hyperhomocysteinemia and severity of peripheral vascular disease and its outcomes. Int J Sci Res. 2018;7(5):1-3.
- Zakhariev T, Grozdinski D, Stankev M, et al. Strategy of the surgical approach to combined coronary and peripheral atherosclerosis. Khirurgiia (Sofiia). 2000;56(6):5-9.
- Rajendran S, Prabhu AD, Thazhakuni I, et al. Simultaneous off-pump coronary artery bypass grafting and ascending aortobifemoral bypass graft via ventral abdominal route. Innovations (Phila). 2007;2(2):84-5.
- Brien TO, Walsh M, McGloughlin T. On reducing abnormal hemodynamics in the femoral end-to-side anastomosis: The influence of mechanical factors. Ann Biomed Eng. 2005;33(3):310-22.
- Schainfeld RM. Management of peripheral arterial disease and intermittent claudication. J Am Board Fam Pract. 2001;14(6):443-50.
- Khan S, Cleanthis M, Smout J, et al. Life-style modification in peripheral arterial disease. Eur J Vasc Endovasc Surg. 2005;29(1):2-9.
- Chiu KW, Davies RS, Nightingale PG, et al. Review of direct anatomical open surgical management of atherosclerotic aorto-iliac occlusive disease. Eur J Vasc Endovasc Surg. 2010; 39(4):460-71.
- Davidovic LB, Lotina SI, Kostic DM, et al. Factors determining late patency of aortobifemoral bypass graft. Srp Arh Celok Lek. 1997;125(1-2):24-35.
- Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007;45:S5-67.
- Chiu KW, Davies RS, Nightingale PG, et al. Review of direct anatomical open surgical management of atherosclerotic aortoiliac occlusive disease. Eur J Vasc Endovasc Surg. 2010; 39(4):460-71.
- Batt M, Baptiste EJ, O’Connor S, et al. Early and late results of contemporary management of 37 secondary aortoenteric fistulae. Eur J Vasc Endovasc Surg. 2011;41(6):748-57.
- Brothers TE, Greenfield LJ. Long-term results of aortoiliac reconstruction. J Vasc Interv Radiol. 1990;1(1):49-55.
- Sen I, Stephen E, Agarwal S. Clinical profile of aortoiliac occlusive disease and outcomes of aortobifemoral bypass in India. J Vasc Surg. 2013;57(2):20-5.
- Jongkind V, Akkersdijk GJ, Yeung KK, et al. A systematic review of endovascular treatment of extensive aortoiliac occlusive disease. J Vasc Surg. 2010;52(5):1376-83.
- Kavaliauskiene Z, Antusevas A, Kaupas RS, et al. Recent advances in endovascular treatment of aortoiliac occlusive disease. Medicina (Kaunas). 2012;48(12):653-9.
- Lun Y, Zhang J, Wu X, et al. Comparison of midterm outcomes between surgical treatment and endovascular reconstruction for chronic infrarenal aortoiliac occlusion. J Vasc Interv Radiol. 2015;26(2):196-204.
- Lun Y, Zhang J, Shen S, et al. Comparison of mid-term outcomes between surgical treatment and endovascular reconstruction for chronic aortoiliac occlusion. Zhonghua Wai Ke Za Zhi. 2015;53(5):368-72.
- Hans SS, DeSantis D, Siddiqui R, et al. Results of endovascular therapy and aortobifemoral grafting for Transatlantic Inter-Society type C and D aortoiliac occlusive disease. Surgery. 2008;144(4):583-9.
- Psacharopulo D, Ferrero E, Ferri M, et al. Increasing efficacy of endovascular recanalization with covered stent graft for TransAtlantic Inter-Society Consensus II D aortoiliac complex occlusion. J Vasc Surg. 2015;62(5):1219-26.
- Lecot F, Sabbe T, Houthoofd S, et al. Long-term Results of Totally Laparoscopic Aortobifemoral Bypass. Eur J Vasc Endovasc Surg. 2016;52(5):581-87.
- Ricco JB, Cau J, Biancari F, et al. Outcome After Open and Laparoscopic Aortic Surgery in Matched Cohorts Using Propensity Score Matching. Eur J Vasc Endovasc Surg. 2016;52(2):179-88.
- De Caridi G, Alimi YS, Hartung O, et al. The role of laparoscopic surgery in the treatment of occlusive and abdominal aortic aneurys. Review of the literature. Minerva Chir. 2009;64(2):211-23.
- Segers B, Horn D, Bazi MO, et al. New development for aorto bifemoral bypass--a clampless and sutureless endovascular and laparoscopic technique. Vascular. 2014;22(3):188-92.
- Kolvenbach R, Da Silva L, Deling O, et al. Video-assisted aortic surgery. J Am Coll Surg. 2000;190(4):451-7.
- Fourneau I, Daenens K, Nevelsteen. Minimal-access aortic surgery: the potentials of hand-assisted laparoscopy. Acta Chir Belg. 2004;104(5):499-504.
- Pascarella L, Aboul Hosn M. Minimally Invasive Management of Severe Aortoiliac Occlusive Disease. J Laparoendosc Adv Surg Tech A. 2018;28(5):562-68.
- Dion YM, Gracia CR. A new technique for laparoscopic aortobifemoral grafting in occlusive aortoiliac disease. J Vascular Sur. 1997;26(4):685-92.
- Samson RH, Showalter DP, Lepore MR, et al. Improved patency after axillofemoral bypass for aortoiliac occlusive disease. J Vasc Surg. 2018;30419-1.
- Schneider JR, Golan JF. The role of extraanatomic bypass in the management of bilateral aortoiliac occlusive disease. Semin Vasc Surg. 1994;7(1):35-44.
- Akingboye AA, Patel B, Cross FW. Femorofemoral Crossover Bypass Graft Has Excellent Patency When Performed with EVAR for AAA with UIOD. South Med J. 2018;111(1):56-63.
- Davidovic LB, Lotina SI, Kostic DM, et al. Dacron and polytetrafluoroethylene aorto-bifemoral grafts. Srp Arh Celok Lek. 1997;125:75-83.
- Rychlik IJ, Davey P, Murphy J, et al. A meta-analysis to compare Dacron versus polytetrafluroethylene grafts for above-knee femoropopliteal artery bypass. J Vasc Surg. 2014;60(2):506-15.
- Becquemin JP, Melliere D, Benhaiem N. Late occlusion of aorto-bifemoral grafts. Causes and management. J Cardiovasc Surg. 1987;28(1):12-7.