Clinical implications of the ossified pterygospinous ligament
Sergey Lvovich Kabak1, Yuliya Michailovna Melnichenko1*, Natallia Victorovna Zhuravleva1 and Nina Alexandrovna Savrasova2
1Departments of Human Morphology, Belarusian State Medical University, Minsk, Belarus
2Radiation Examination and Radiation Therapy, Belarusian State Medical University, Minsk, Belarus
- *Corresponding Author:
- Yuliya Michailovna Melnichenko, PhD
Associate Professor, Human Morphology Department, Belarusian State Medical University, Dzerzhinskogo Avenue 83, Minsk, Belarus
Tel: +375 (296) 729153
E-mail: mjm1980@yandex.byu
Date of Received: October 4th, 2016
Date of Accepted: January 15th, 2017
Published Online: January 19th, 2017
© Int J Anat Var (IJAV). 2016; 9: 60–63.
[ft_below_content] =>Keywords
cone-beam computed tomography, ligaments, neuralgia, ossification
Introduction
Complete or partial ossification of the pterygospinous ligament that connects the posterior border of the lateral pterygoid plate to the spine of the sphenoid bone occurs in 1-31.2% of people [1,2]. The ossified pterygospinous ligament is detected on the lateral or medial side or crossing over the foramen ovale on the radiographs of the dry scull in the axial projection with the beam positioned at the right angle to the base of the skull [3].
In all cases, the presence of the ossified pterygospinous ligament was detected ex vivo. Based on the relationship between anatomical structures in the infratemporal fossa, it is assumed that ossification of the ligament may be accompanied by clinical symptoms. In particular, pressure applied to the lingual nerve by the ossified pterygospinous ligament during contraction of the medial pterygoid muscle may cause tongue numbness and pain upon talking and chewing [4,5]. According to Das and Paul, ossification of the pterygospinous ligament leads to taste disorders of the anterior 2/3 of the tongue due to compression of the chorda tympani [6]. However, no evidence of the direct relationship between the ossification of the pterygospinous ligament and neurological symptoms was found in the literature.
The aim of the present study was to assess neurological symptoms in patients with ossified pterygospinous ligament detected in vivo using the Cone Beam Computed Tomography (CBCT).
Case Report
The presence of the ossified pterygospinous ligament was revealed in three male patients using cone-beam computed tomography (CBCT). First, axial and sagittal slices of the facial skull were consistently assessed in the multiplanar reconstruction mode. The foramen ovale was also identified at the base of the skull in the same mode. Then, the soft tissue structure and density were traced on multiple slices in the direction of the posterior edge of the lateral pterygoid plate. In addition, the search of opaque shadows was performed in the sagittal section, as well as in the non-standard plane, which corresponds to the spatial position of the lateral pterygoid plate.
Patient B., 52 y. o., considered himself sick since April 2015, when after hypothermia and acute respiratory disease he started feeling lingual pain while swallowing. He was assessed and treated by an otolaryngologist. Two months after the pain onset in the tongue, he referred to a dental surgeon with the chief complaint of burning sensation and tingling in the right half of the tongue accompanied by the feeling of “swelling, awkwardness and heaviness”.
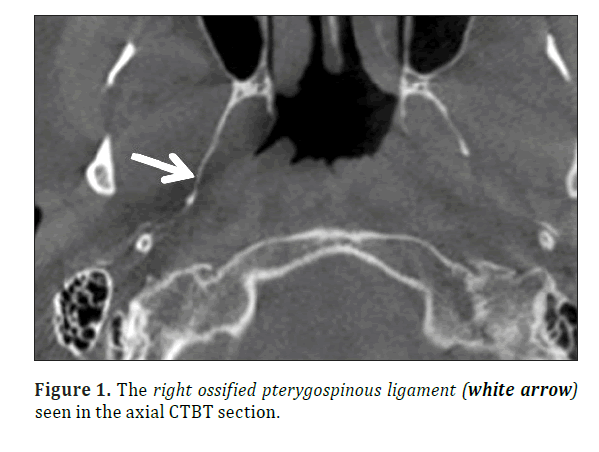
No clinical signs of paresthesia and sensitivity disruption were found. On intraoral examination, slight mucosal edema of the anterior 2/3 of the tongue (more on the right) and hypertrophy and hyperemia of filiform papillae were observed. The tongue was painful on palpation. The linear radiopaque structure of uneven thickness (0, 52-0.8 mm) connecting the bony prominence on the lateral plate of the pterygoid process to the spine of the sphenoid was visualized in the axial sections obtained with CBCT. Typical localization of the detected shadow allowed to identify it as the calcified pterygospinous ligament (Figure 1). The final diagnosis was “neuralgia of the lingual nerve on the right.”
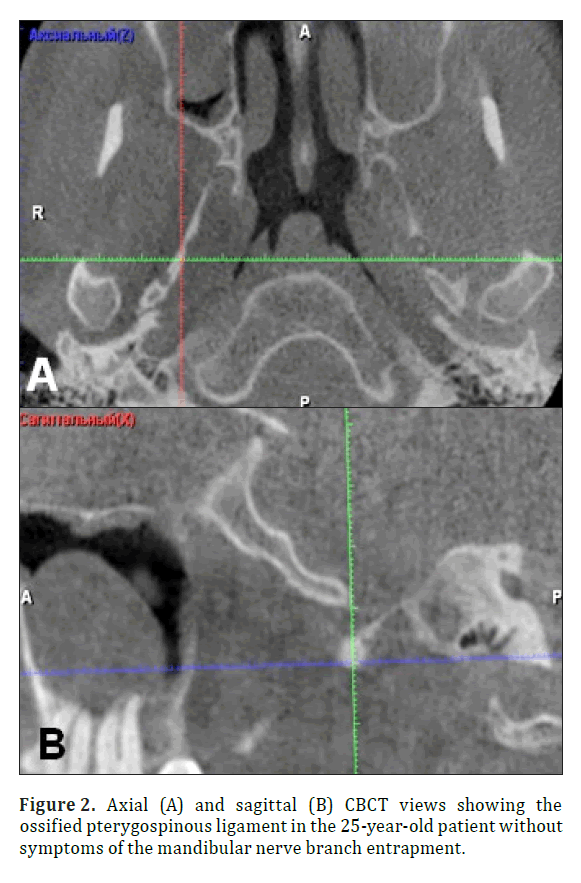
CBCT scans of two other patients (33 and 25 years old), which were referred for the maxillary sinus examination, also showed the presence of the calcified pterygospinous ligament. In both cases, it looked like the excess linear shadow of uneven thickness and bone-like density connecting the posterior edge of the lateral pterygoid plate to the spine of the sphenoid in the axial sections (Figure 2A).
In the sagittal and coronal sections, the ligament was not visualized throughout the whole length because its long axis was oriented at an angle to those planes. In the sagittal sections, it was visualized as a radiopaque fragment with unclear outlines (Figure 2A, B).
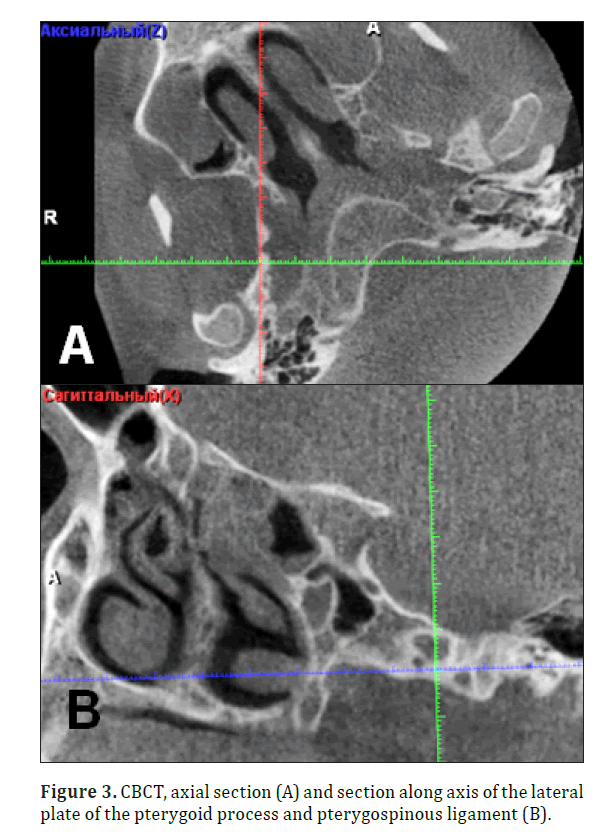
In order to visualize the whole ligament in the vertical dimension section planes were shifted in the axial and coronal view box so that they coincided with the axis of the ligament (Figure 3A). An arbitrary cross-section allowed not only to obtain an image of the pterygospinous ligament throughout its full length in the vertical plane, but also to visualize the foramen of Civinini, which was reduced due to calcification of the ligament (Figure 3B). Comparing CBCT images in the axial and arbitrary cross-sections showed that the calcified pterygospinous ligament appeared as the radiopaque band in the vertical plane with its vertical dimension greater than the horizontal size (4.18 and 1.70 mm, respectively). The same slice clearly showed the broad upper part of the lateral pterygoid plate.
The foramen within the ossified pterygospinous ligament was unexpectedly found at the level of connection to the edge of the lateral pterygoid plate (Figure 3B).
Discussion
The small bony prominence (Chivinini spine) is routinely revealed approximately in the middle of the posterior edge of the lateral plate of the pterygoid process of the sphenoid bone. That is the starting point of the pterygospinous ligament, which runs down to the spine on the lower surface of the greater wing of the sphenoid bone, near the junction with the temporal bone.
Complete ossification of the pterygospinous ligament leads to the formation of the pterygospinous foramen on the medial wall of the infratemporal fossa (Civinini foramen). Many researchers describe this foramen like an atavism in human [1,8]. Because some placental mammals, including the Old- World monkeys, always have a bony band connecting the lateral plate of the pterygoid process with the pterygoid spine [7]. Calcification of the pterygospinous ligament at a young age confirms that it is not so much of an age change as a genetically determined factor [5]. In our study, the calcified pterygospinous ligament was observed in young people.
Wide fluctuations in frequency of presence of the ossified pterygospinous ligament (from 1% to 30%) can be primarily explained by variations in the sample size, sometimes including 50 skulls [6]. In the large sample (6000 skulls), the ossified ligament was found in 5% of cases [9]. It is possible that a partially ossified ligament cannot survive skull maceration. Moreover, racial differences in the detection frequency of ossified pterygospinous ligament were observed. It was found four times more often in Caucasians than in black race (8.38% and 1.95%, respectively) [5].
In all cases described in the literature, the pterygospinous foramen was found in dry skulls posthumously or during anatomical dissection of the infratemporal fossa. In the present study, we were able to identify the completely calcified pterygospinous ligament in vivo using CBCT. Calcification makes such radiolucent structures as tendons, cartilage, ligaments visible. Their identification is mainly based on typical morphological characteristics (location, spatial position, shape, thickness) and relationship to other anatomical structures. Presence of the interrupted linear shade is a sign of partial ligament ossification. The calcified pterygospinous ligament described macroscopically by von Lüdinghausen et al., had similar shape and length on the horizontal CT scan of a dry skull [7].
Complete or partial ossification of the pterygospinous ligament is of clinical significance due to the close location of major anatomical structures such as the lingual nerve and chorda tympani [2,5].
In the infratemporal fossa the lingual nerve, the branch of the posterior trunk of the mandibular nerve, is at first located between the lateral pterygoid and tensor veli palatini muscles, where it connects with chorda tympani. Then, the lingual nerve passes downward on the surface of the medial pterygoid muscle, and follows the inner surface of the mandibular ramus [5]. Masticatory muscles contractions do not usually lead to compression or stretching of the nerve. However, calcification of the pterygospinous ligament can be the cause of the tunnel syndrome. Compression of the lingual nerve between the ossified ligament (rigid structure located outside of the nerve) and medial pterygoid muscles was first described by Peuker et al. [4]. It was an incidental finding discovered during preparation of the infratemporal fossa. Nayak et al. described the similar finding in an autopsy case [10]. Authors believed that mobility of the lingual nerve, which could prevent compression, was limited by the presence of the distal anastomosis with the inferior alveolar nerve in that case.
Our findings confirm that ossification of the pterygospinous ligament may lead to the lingual nerve neuralgia. On the other hand, even completely calcified ligament may present with no symptoms as it was observed in our study. Apparently, that is determined by individual characteristics of the course of the of the mandibular nerve branches in relation to the pterygospinous ligament. Von Lüdinghausen et al. [7] described inferior alveolar, lingual and buccal nerves passing the ligament more often on the lateral side than on the medial (5 out of 68 cases). The position of the mandibular nerve on the inner side of the ossified pterygospinous ligament gives the higher chance of compression of its branches and neurological disorders development.
Despite the block of the second and third branches of the trigeminal nerve seem to be easy, according to ESRA (European Society of Regional Anesthesia and Pain Therapy) it is not always effective [11]. For example, out of 49 mandibular blocks 4 injections are unsuccessful. The reason is the spread of a local anesthetic into the area distant from the foramen ovale and pterygopalatine fossa, where the trunks of the maxillary and mandibular nerves are located. The ossified pterygospinous ligament, which we observed in conjunction with the wide lateral plate of the pterygoid process can potentially be an obstacle in the way of the anesthetic solution to the oval foramen. Those structures prevent the movement of the needle to the trigeminal ganglion through the lateral percutaneous subzygomatic access [8].
As a conclusion, the calcified pterygospinous ligament can be detected in vivo using CBCT. Sometimes it may cause the lingual nerve neuralgia, as well as in combination with a broad plate of the pterygoid process, it may restrict the access to structures within the infratemporal fossa.
References
- B KK, K V. Anatomical study of pterygospinous and pterygoalar bar in human skulls with their phylogeny and clinical significance. J Clin Diagn Res. 2014;8(9):AC10-13.
- Goyal N, Jain A. An anatomical study of the pterygospinous bar and foramen of Civinini. Surg Radiol Anat. 2016;38(8):931-936.
- Saran RS, Ananthi KS, Subramaniam A, Balaji MT, Vinaitha D, Vaithianathan G. Foramen of civinini: a new anatomical guide for maxillofacial surgeons. J Clin Diagn Res. 2013;7(7):1271- 1275.
- Peuker ET, Fischer G, Filler TJ. Entrapment of the lingual nerve due to an ossified pterygospinous ligament. Clin Anat. 2001;14(4):282-284.
- Piagkou M, Demesticha T, Piagkos G, Georgios A, Panagiotis S. Lingual nerve entrapment in muscular and osseous structures. Int J Oral Sci. 2010;2(4):181-189.
- Das S, Paul S. Ossified pterygospinous ligament and its clinical implications. Bratisl Lek Listy. 2007;108(3):141-143.
- von Lüdinghausen M, Kageyama I, Miura M, Alkhatib M. Morphological peculiarities of the deep infratemporal fossa in advanced age. Surg Radiol Anat. 2006;28(3):284-292.
- Tubbs RS, May WR Jr, Apaydin N, Shoja MM, Shokouhi G, Loukas M, Cohen-Gadol AA. Ossification of ligaments near the foramen ovale: an anatomic study with potential clinical significance regarding transcutaneous approaches to the skull base. Neurosurgery. 2009;65(6 Suppl):60-4; discussion 64.
- Chouke KS. Injection of mandibular nerve and gasserian ganglion; an anatomic study. Am J Surg. 1949;78(1):80-85.
- Nayak SR, Rai R, Krishnamurthy A, Prabhu LV, Ranade AV, Mansur DI, Kumar S. An unusual course and entrapment of the lingual nerve in the infratemporal fossa. Bratisl Lek Listy. 2008;109(11):525-527.
- European Society of Regional Anaesthesia &Pain Therapy (ESRA). Handbook of regional anesthesia (ESRA, 2007). European Society of Regional Anaesthesia & Pain Therapy (ESRA). 2007.
Sergey Lvovich Kabak1, Yuliya Michailovna Melnichenko1*, Natallia Victorovna Zhuravleva1 and Nina Alexandrovna Savrasova2
1Departments of Human Morphology, Belarusian State Medical University, Minsk, Belarus
2Radiation Examination and Radiation Therapy, Belarusian State Medical University, Minsk, Belarus
- *Corresponding Author:
- Yuliya Michailovna Melnichenko, PhD
Associate Professor, Human Morphology Department, Belarusian State Medical University, Dzerzhinskogo Avenue 83, Minsk, Belarus
Tel: +375 (296) 729153
E-mail: mjm1980@yandex.byu
Date of Received: October 4th, 2016
Date of Accepted: January 15th, 2017
Published Online: January 19th, 2017
© Int J Anat Var (IJAV). 2016; 9: 60–63.
Abstract
The aim of the present study was to assess neurological symptoms in patients with ossified pterygospinous ligament detected in vivo using the cone beam computed tomography (CBCT). Three CBCT scans of patients from dental outpatient hospitals of Minsk, Belarus were performed on the Planmeca ProMax® 3D Max unit using standard exposure and patient positioning protocol. Reformatted panoramic and sagittal CBCT sections were analyzed. One case of entrapment of the lingual nerve by the ossified pterygospinous ligament was observed. In two other cases ossification of the pterygospinous ligament was not accompanied by any neurological symptoms. Calcification of the pterygospinous ligament can be detected in vivo using CBCT. Sometimes it may affect the lingual nerve producing symptoms of neuralgia. When combined with a broad lateral plate of the pterygoid process, it may restrict the access to structures located in the infratemporal fossa.
-Keywords
cone-beam computed tomography, ligaments, neuralgia, ossification
Introduction
Complete or partial ossification of the pterygospinous ligament that connects the posterior border of the lateral pterygoid plate to the spine of the sphenoid bone occurs in 1-31.2% of people [1,2]. The ossified pterygospinous ligament is detected on the lateral or medial side or crossing over the foramen ovale on the radiographs of the dry scull in the axial projection with the beam positioned at the right angle to the base of the skull [3].
In all cases, the presence of the ossified pterygospinous ligament was detected ex vivo. Based on the relationship between anatomical structures in the infratemporal fossa, it is assumed that ossification of the ligament may be accompanied by clinical symptoms. In particular, pressure applied to the lingual nerve by the ossified pterygospinous ligament during contraction of the medial pterygoid muscle may cause tongue numbness and pain upon talking and chewing [4,5]. According to Das and Paul, ossification of the pterygospinous ligament leads to taste disorders of the anterior 2/3 of the tongue due to compression of the chorda tympani [6]. However, no evidence of the direct relationship between the ossification of the pterygospinous ligament and neurological symptoms was found in the literature.
The aim of the present study was to assess neurological symptoms in patients with ossified pterygospinous ligament detected in vivo using the Cone Beam Computed Tomography (CBCT).
Case Report
The presence of the ossified pterygospinous ligament was revealed in three male patients using cone-beam computed tomography (CBCT). First, axial and sagittal slices of the facial skull were consistently assessed in the multiplanar reconstruction mode. The foramen ovale was also identified at the base of the skull in the same mode. Then, the soft tissue structure and density were traced on multiple slices in the direction of the posterior edge of the lateral pterygoid plate. In addition, the search of opaque shadows was performed in the sagittal section, as well as in the non-standard plane, which corresponds to the spatial position of the lateral pterygoid plate.
Patient B., 52 y. o., considered himself sick since April 2015, when after hypothermia and acute respiratory disease he started feeling lingual pain while swallowing. He was assessed and treated by an otolaryngologist. Two months after the pain onset in the tongue, he referred to a dental surgeon with the chief complaint of burning sensation and tingling in the right half of the tongue accompanied by the feeling of “swelling, awkwardness and heaviness”.
No clinical signs of paresthesia and sensitivity disruption were found. On intraoral examination, slight mucosal edema of the anterior 2/3 of the tongue (more on the right) and hypertrophy and hyperemia of filiform papillae were observed. The tongue was painful on palpation. The linear radiopaque structure of uneven thickness (0, 52-0.8 mm) connecting the bony prominence on the lateral plate of the pterygoid process to the spine of the sphenoid was visualized in the axial sections obtained with CBCT. Typical localization of the detected shadow allowed to identify it as the calcified pterygospinous ligament (Figure 1). The final diagnosis was “neuralgia of the lingual nerve on the right.”
CBCT scans of two other patients (33 and 25 years old), which were referred for the maxillary sinus examination, also showed the presence of the calcified pterygospinous ligament. In both cases, it looked like the excess linear shadow of uneven thickness and bone-like density connecting the posterior edge of the lateral pterygoid plate to the spine of the sphenoid in the axial sections (Figure 2A).
In the sagittal and coronal sections, the ligament was not visualized throughout the whole length because its long axis was oriented at an angle to those planes. In the sagittal sections, it was visualized as a radiopaque fragment with unclear outlines (Figure 2A, B).
In order to visualize the whole ligament in the vertical dimension section planes were shifted in the axial and coronal view box so that they coincided with the axis of the ligament (Figure 3A). An arbitrary cross-section allowed not only to obtain an image of the pterygospinous ligament throughout its full length in the vertical plane, but also to visualize the foramen of Civinini, which was reduced due to calcification of the ligament (Figure 3B). Comparing CBCT images in the axial and arbitrary cross-sections showed that the calcified pterygospinous ligament appeared as the radiopaque band in the vertical plane with its vertical dimension greater than the horizontal size (4.18 and 1.70 mm, respectively). The same slice clearly showed the broad upper part of the lateral pterygoid plate.
The foramen within the ossified pterygospinous ligament was unexpectedly found at the level of connection to the edge of the lateral pterygoid plate (Figure 3B).
Discussion
The small bony prominence (Chivinini spine) is routinely revealed approximately in the middle of the posterior edge of the lateral plate of the pterygoid process of the sphenoid bone. That is the starting point of the pterygospinous ligament, which runs down to the spine on the lower surface of the greater wing of the sphenoid bone, near the junction with the temporal bone.
Complete ossification of the pterygospinous ligament leads to the formation of the pterygospinous foramen on the medial wall of the infratemporal fossa (Civinini foramen). Many researchers describe this foramen like an atavism in human [1,8]. Because some placental mammals, including the Old- World monkeys, always have a bony band connecting the lateral plate of the pterygoid process with the pterygoid spine [7]. Calcification of the pterygospinous ligament at a young age confirms that it is not so much of an age change as a genetically determined factor [5]. In our study, the calcified pterygospinous ligament was observed in young people.
Wide fluctuations in frequency of presence of the ossified pterygospinous ligament (from 1% to 30%) can be primarily explained by variations in the sample size, sometimes including 50 skulls [6]. In the large sample (6000 skulls), the ossified ligament was found in 5% of cases [9]. It is possible that a partially ossified ligament cannot survive skull maceration. Moreover, racial differences in the detection frequency of ossified pterygospinous ligament were observed. It was found four times more often in Caucasians than in black race (8.38% and 1.95%, respectively) [5].
In all cases described in the literature, the pterygospinous foramen was found in dry skulls posthumously or during anatomical dissection of the infratemporal fossa. In the present study, we were able to identify the completely calcified pterygospinous ligament in vivo using CBCT. Calcification makes such radiolucent structures as tendons, cartilage, ligaments visible. Their identification is mainly based on typical morphological characteristics (location, spatial position, shape, thickness) and relationship to other anatomical structures. Presence of the interrupted linear shade is a sign of partial ligament ossification. The calcified pterygospinous ligament described macroscopically by von Lüdinghausen et al., had similar shape and length on the horizontal CT scan of a dry skull [7].
Complete or partial ossification of the pterygospinous ligament is of clinical significance due to the close location of major anatomical structures such as the lingual nerve and chorda tympani [2,5].
In the infratemporal fossa the lingual nerve, the branch of the posterior trunk of the mandibular nerve, is at first located between the lateral pterygoid and tensor veli palatini muscles, where it connects with chorda tympani. Then, the lingual nerve passes downward on the surface of the medial pterygoid muscle, and follows the inner surface of the mandibular ramus [5]. Masticatory muscles contractions do not usually lead to compression or stretching of the nerve. However, calcification of the pterygospinous ligament can be the cause of the tunnel syndrome. Compression of the lingual nerve between the ossified ligament (rigid structure located outside of the nerve) and medial pterygoid muscles was first described by Peuker et al. [4]. It was an incidental finding discovered during preparation of the infratemporal fossa. Nayak et al. described the similar finding in an autopsy case [10]. Authors believed that mobility of the lingual nerve, which could prevent compression, was limited by the presence of the distal anastomosis with the inferior alveolar nerve in that case.
Our findings confirm that ossification of the pterygospinous ligament may lead to the lingual nerve neuralgia. On the other hand, even completely calcified ligament may present with no symptoms as it was observed in our study. Apparently, that is determined by individual characteristics of the course of the of the mandibular nerve branches in relation to the pterygospinous ligament. Von Lüdinghausen et al. [7] described inferior alveolar, lingual and buccal nerves passing the ligament more often on the lateral side than on the medial (5 out of 68 cases). The position of the mandibular nerve on the inner side of the ossified pterygospinous ligament gives the higher chance of compression of its branches and neurological disorders development.
Despite the block of the second and third branches of the trigeminal nerve seem to be easy, according to ESRA (European Society of Regional Anesthesia and Pain Therapy) it is not always effective [11]. For example, out of 49 mandibular blocks 4 injections are unsuccessful. The reason is the spread of a local anesthetic into the area distant from the foramen ovale and pterygopalatine fossa, where the trunks of the maxillary and mandibular nerves are located. The ossified pterygospinous ligament, which we observed in conjunction with the wide lateral plate of the pterygoid process can potentially be an obstacle in the way of the anesthetic solution to the oval foramen. Those structures prevent the movement of the needle to the trigeminal ganglion through the lateral percutaneous subzygomatic access [8].
As a conclusion, the calcified pterygospinous ligament can be detected in vivo using CBCT. Sometimes it may cause the lingual nerve neuralgia, as well as in combination with a broad plate of the pterygoid process, it may restrict the access to structures within the infratemporal fossa.
References
- B KK, K V. Anatomical study of pterygospinous and pterygoalar bar in human skulls with their phylogeny and clinical significance. J Clin Diagn Res. 2014;8(9):AC10-13.
- Goyal N, Jain A. An anatomical study of the pterygospinous bar and foramen of Civinini. Surg Radiol Anat. 2016;38(8):931-936.
- Saran RS, Ananthi KS, Subramaniam A, Balaji MT, Vinaitha D, Vaithianathan G. Foramen of civinini: a new anatomical guide for maxillofacial surgeons. J Clin Diagn Res. 2013;7(7):1271- 1275.
- Peuker ET, Fischer G, Filler TJ. Entrapment of the lingual nerve due to an ossified pterygospinous ligament. Clin Anat. 2001;14(4):282-284.
- Piagkou M, Demesticha T, Piagkos G, Georgios A, Panagiotis S. Lingual nerve entrapment in muscular and osseous structures. Int J Oral Sci. 2010;2(4):181-189.
- Das S, Paul S. Ossified pterygospinous ligament and its clinical implications. Bratisl Lek Listy. 2007;108(3):141-143.
- von Lüdinghausen M, Kageyama I, Miura M, Alkhatib M. Morphological peculiarities of the deep infratemporal fossa in advanced age. Surg Radiol Anat. 2006;28(3):284-292.
- Tubbs RS, May WR Jr, Apaydin N, Shoja MM, Shokouhi G, Loukas M, Cohen-Gadol AA. Ossification of ligaments near the foramen ovale: an anatomic study with potential clinical significance regarding transcutaneous approaches to the skull base. Neurosurgery. 2009;65(6 Suppl):60-4; discussion 64.
- Chouke KS. Injection of mandibular nerve and gasserian ganglion; an anatomic study. Am J Surg. 1949;78(1):80-85.
- Nayak SR, Rai R, Krishnamurthy A, Prabhu LV, Ranade AV, Mansur DI, Kumar S. An unusual course and entrapment of the lingual nerve in the infratemporal fossa. Bratisl Lek Listy. 2008;109(11):525-527.
- European Society of Regional Anaesthesia &Pain Therapy (ESRA). Handbook of regional anesthesia (ESRA, 2007). European Society of Regional Anaesthesia & Pain Therapy (ESRA). 2007.