Clinical reflection and leadership in efficient management of patients in the Intensive Care Unit
Received: 25-May-2020 Accepted Date: Nov 13, 2020; Published: 16-Nov-2020
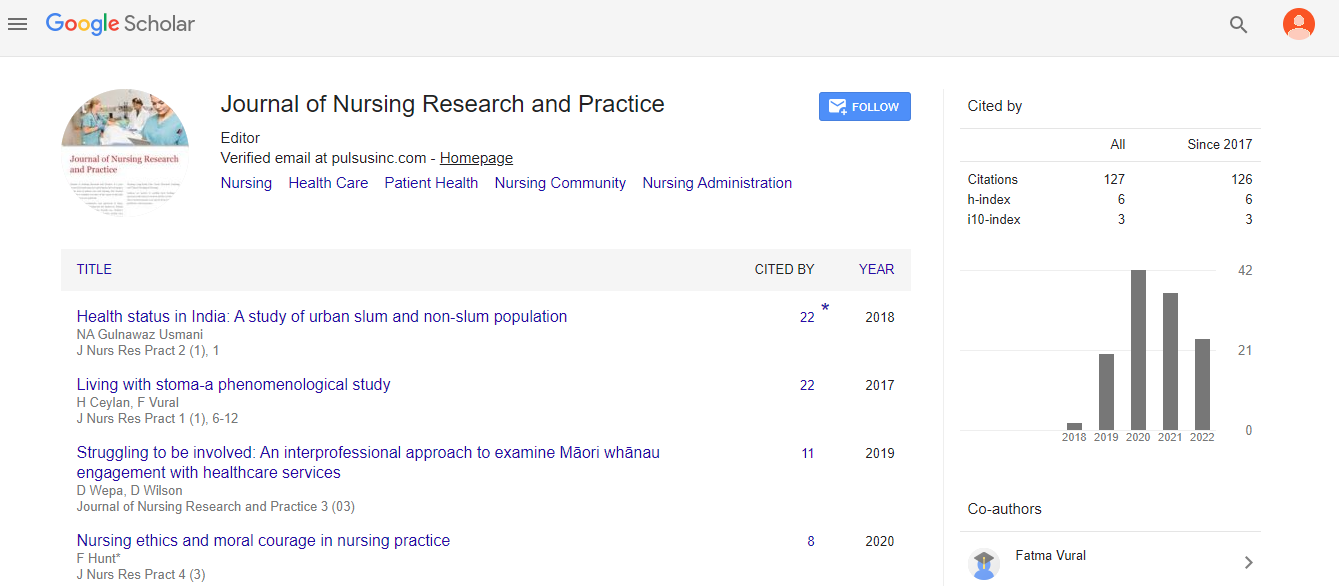
Citation: Alharthi N. Clinical Reflection and leadership in efficient management of patients in the Intensive Care Unit. J Nurs Res Pract. 2020;4(5):1-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Reflection is made on the strengths and limitations of a transformational leadership style in the context of providing care to patients in critical care units, collaborating with other healthcare practitioners and the patient’s family. This involves a case study of a 49-year old patient admitted to an intensive care unit (ICU) due to severe chest pain; later transferred to cardiac catheter laboratory is presented. As part of reflective practice, the author’s role in the team is explored using Belbin’s 9 team roles as a guide. ICU is seen to be a complex, dynamic setting with healthcare practitioners fulfilling highly specialized roles. Conflicts in the team were avoided since all team members respected the roles of each team member. A discussion on how hierarchies in the team could possibly result in poor teamwork was also explored against what the author was experiencing in the ICU. A discussion follows how transformational leadership developed the author’s emotional intelligence and improved team members’ satisfaction with the quality teamwork. A critique is put forward on the importance of effective communication. Both verbal and nonverbal messages are critical in conveying and receiving important information in an ICU team. Although positive communication skills are defined, there are still some gaps in practice such as a need to develop therapeutic communication skills for positive health outcomes in patients. An evaluation of power in the team and an imbalance in power was observed. Power in a team is seen as critical in determining if resources in ICU were sufficiently used and that patients received quality, timely care and the dynamic nature of an ICU environment is examined. Patient’s needs, interventions can change quickly in an ICU environment which leads to complexities especially if a patient is clinically deteriorating. Recommendations are made on the importance of developing inter professional collaborations, effective leadership and communication among team members.
Keywords
Intensive Care Unit (ICU); Nursing practice; Teamwork; Midwifery
Introduction
Nurses play crucial roles in delivering and leading high-quality patient care, acting as patient advocates and in ensuring that patient-centered care is practiced in all levels of care [1]. In response to the increasing complexities of healthcare delivery, registered nurses have taken additional roles, which include nurse prescribers, policymakers, and leaders and advanced nurse practitioners [2]. As a registered nurse working in intensive care units for the last five years at King Faisal Hospital in Saudi Arabia, I have seen the current challenges that ICU nurses face. One of these include understaffing of ICU nurses, which can have an impact on the quality of care and lead to inevitable bed closure due to lack of nursing staff members [3]. However, these challenges can be addressed through effective leadership [4]. In Ireland, intensive or critical care nurses are expected to advocate for critically ill patients and their families and to become leaders in this area of care (Irish Association of Critical Care Nurses [5]. Critical care nurses are also strongly encouraged to engage in healthcare policy development and future critical care strategies [5].
Literature Review
The Nursing and Midwifery Council’s (NMC) [6] Code of Conduct has stressed the importance of nursing leadership and the promotion of health and wellbeing of patients. Since nurses are in direct contact with patients in different healthcare settings, they are able to recognise the health and social care needs of the patients [7]. In this essay, the development of leadership skills and how these could be applied in a team setting will be critically discussed. Past personal experiences and evidence from published studies and policies will be used to underpin the discussion in this essay.
Critical reflection on self
Reflection in healthcare settings is strongly promoted since this has been associated with professional development and improvements in the quality of patient care [8]. In nursing settings, reflection is described as a tool that allows nurses to generate professional knowledge [9]. It is also defined as a process that helps nurses examine and explore an incident or issue in more depth and use learnings from these experiences to improve current and future nursing practice [10]. Learning from practice is also essential since this will help develop a culture of enquiry, learning and exploration within teams [9]. A culture of learning within a team or organisation could help clarify roles and improve performance [11]. For instance, more senior nurses can share knowledge and expertise with junior colleagues, which in turn can help foster a culture of support and development. The importance of reflection in supporting registered and student nurses in professional learning and development is also emphasised by the Nursing and Midwifery Council (NMC) [6].
Despite the importance of reflection, this practice may be viewed negatively due to its exhaustive application in different care settings [9]. Although some negative perceptions may persist, the evidence-base on the effectiveness of reflection in improving practice is well established [12]. Further, nursing curricula now integrate reflection in practice to prepare student nurses to become reflective practitioners once they become registered nurses [13]. The theory of reflective practice in nursing is identified as a middle-range theory [14]. This theory proposes that reflective practice involves the following: reflection before actions; reflection in action; refection on action and reflection beyond action [15]. Reflection before action involves reflection in advance of a learning situation or prior to entering clinical practice [16]. This type of reflection allows nurses to become mindful of future actions and provides them with opportunities to consider any particular skills that would be needed for a specific clinical situation. [16] Reiterates that through reflection before action, nurses become better prepared as they anticipate situations or scenarios in clinical practice.
Reflection in action entails reflection while nurses are immersed in the clinical situation [17]. Meanwhile, reflection on action requires retroactive analysis to recreate incidents in clinical practice [18]. This type of reflection helps nurses connect theories to actual practice [16]. Reflection beyond action, on the other hand, requires an analysis of one’s clinical practice and how nurses developed. The main aim of reflection is for healthcare practitioners to become more equipped in providing high quality care and improve care outcomes [15]. Reflection is critical in improving healthcare and in the context of this essay, this type of practice is necessary in forming leaders who are emotionally competent [19].
Leaders who are emotionally competent are known to be high in emotional intelligence [20] describes emotional intelligence as the ability to manage one’s emotions and the emotions of other team members. In nursing practice, emotional intelligence is known to promote the wellbeing of nurses, which in turn has an impact on their patients and family members [21]. In general, emotional intelligence allows nurses to manage their patients in a more effective manner, improve relationships, make better decisions and improve the quality of care of the patients [19,21,22]. Reflection has been suggested to improve the nurse’s emotional intelligence since critical appraisal of incidents involves identifying the emotions felt during these scenarios [23,24] reiterates that in leadership, it is important for nurses to be self-aware, to have emotional intelligence and to reflect on their own practice. During reflection, a nurse practitioner is encouraged to undergo critical self-reflection in order to become self-aware, which is all necessary in improving one’s emotional intelligence.
In leadership practice, emotional intelligence has been recognised as an important factor in the success of leaders [25] reinforce that emotional intelligence helps individuals work more effectively and manage conflicts within teams. Further, emotional intelligence improves performance and leadership, which are important in promoting the effectiveness of leaders [26]. In a study conducted by Nabih et al. [27], results suggested that emotional intelligence has a positive effect on leadership effectiveness. Leadership effectiveness is described as the extent in which team members perceive their managers as successful leaders [27]. Recent theories suggest that the personality of the leaders, quality characteristics of employees and the conditions in the workplace impact leadership effectiveness [28]. It is argued that health leadership requires communicating with and understanding individuals who have different characteristics and background in a variety of situations and not only focusing on producing health outcomes and processes. Hence, in healthcare settings, leaders who possess emotional intelligence can inspire passion and influence team members to achieve goals that might have been difficult to achieve [22].
One of the leadership styles associated with emotional intelligence is the transformational leadership style. The transformational leadership style promotes positive leadership qualities and inspires followers to achieve team goals through clearly communicating visions and expectations [29]. One of the most important qualities of transformational leaders is their ability to motivate their followers through recognising and addressing their feelings, concerns and perceptions [29]. Emotionally intelligent leaders are also known to demonstrate compassion and teamwork [20]. Further, they are able to develop therapeutic relationships with their patients and team members [20]. In nursing practice, transformational leadership is also associated with greater job satisfaction, lower nursing burnout and reduced nursing turnover [30].
In my own practice as a critical care nurse in the intensive care unit/critical care unit in Saudi Arabia, I am developing the transformational leadership style. Due to the severe conditions of patients admitted in the ICU or critical care units (CCU), leadership style used should be able to address the needs of the patients. Within these settings, nurses should be able to address the complex needs of the patients. Hence, leadership skills are necessary in helping staff members achieve the best health outcomes for the patients and the team [4]. Due to the care environment in the ICU, it is vital that nurse leaders are able to address the different healthcare needs of the patients in a timely and organised manner. In the succeeding part of this essay, I will reflect on a case study that demonstrated my clinical knowledge, leadership skills and emotional intelligence. I will use [31] Gibbs Model of Reflection since this helps me examine and evaluate my own feelings and actions during the incident. This model begins with describing the incident followed by an examination of how I felt about my experiences. An analysis of my actions followed by evaluation will then be done. The Gibbs model [31] also ensures that an action plan is created following the identification of practice gaps.
During a night shift in in the ICU, a 49-year old patient named Mohammed (a pseudonym) was admitted due to severe chest pain. The nursing team providing care performed an assessment to rule out a myocardial infarction. His medical history revealed hypertension, and high cholesterol level. He smokes 1-2 pack of cigarettes each day while his blood pressure and heart rates were elevated. Since Mohammed had difficulty breathing, he was administered with oxygen. After completing an assessment, I observed the patient’s pain levels. A 12-lead electrocardiogram (ECG) was used to assess the patient’s heart. Blood tests were done to evaluate Mohammed’s cardiac enzymes to determine damage in the cardiac muscles. I then related all findings to the cardiologist to help form a care plan for the patient. Following the test results, the cardiologist and the rest of the team informed Mohammed of his laboratory results. Following patient education and obtaining informed consent, the team, transferred Mohammed to the cardiac catheter laboratory to restore the patient’s blood flow.
During the incident, I contemplated on my own thoughts and emotions when caring for Mohammed. I felt confident that the team can help provide relief to Mohammed’s chest pain and provide timely intervention should he suffer from a myocardial infarction. I had worked with the rest of the team in ICU for several months. Hence, I am aware of our team roles and how we communicate with each other. I was aware that Mohammed could suffer a cardiac arrest any time during his admission in the ICU. However, I was confident that the team can provide him with the best care since we have been trained on how to respond to a cardiac arrest. In the case study, Mohammed was transferred to the cardiac catheter laboratory following a discussion between the team and Mohammed. Involving patients in decisionmaking regarding his care plan and interventions/treatment is consistent with the NMC [6] Code of Conduct on promoting patient-centred care.
An analysis of the team’s action and my leadership skills within the ICU nursing team revealed that we were able to respond promptly to the care needs of the patient and followed hospital protocol on the assessment of patients in ICU settings. Since I have been working with the team for several months, it was not difficult to identify our team roles and use this knowledge to improve communication and teamwork. According to Belbin [32], there are 9 roles common in a team. These include team working, monitorevaluator, coordinator, specialist, shaper, planner, completer-finisher, implementer and resource investigator. In clinical settings, a single person may demonstrate two or more roles in a team [32]. Importantly, it is not necessary for a team to have all 9 roles present before it can achieve its vision or goals. On evaluation, I see myself as a completer-finisher, implementer, coordinator and specialist. All these roles were essential in leading the team during Mohammed’s assessment and in coordinating care with the cardiologist. Through recognising individual team roles, I am able to delegate tasks during assessment. Further, examining the team roles assumed by my team members helped me identify the strengths and weaknesses of my team. It also helped me identify strategies that are necessary to address the weaknesses of the team. During the care of the patient, I also realised the importance of effective communication. Since the ICU is a highly dynamic healthcare setting that requires specialist knowledge and skills, it is essential for ICU nurse leaders and team members to communicate effectively. I was able to communicate through verbal and non-verbal messages with my team members. Practising effective communication skills such as listening attentively to my team mates would help them feel that they are valued and part of the team [33].
This self-reflection also helped me develop my emotional intelligence since I was able to manage my emotions during patient care. My previous experiences in the ICU settings and use of evidence-based care also helped me make decisions regarding Mohammed’s care. As an ICU nurse in the last five years, I realised that I should continue to learn and support junior ICU nurses in their own learning and development. Through reflection, I learned the importance of positive role modelling for my junior colleagues. I realised that part of modelling involves helping them increase their self-confidence through teaching them clinical and non-clinical skills and helping them develop emotional intelligence. The latter would involve showing compassion and empathy to the patient while they are receiving care in the ICU settings. Patients who are admitted in these settings often report increased anxiety and fear [34]. Hence, as a nurse leader, I should also address this concern in the ICU setting. Hence, part of my professional development plan is to improve my ability to manage anxiety and fear of patients in ICU settings. There is also evidence that families also suffer from anxiety when their family members are receiving care in ICU settings [34]. I should also participate in trainings on how to support families who are experiencing anxiety while their patients are in the ICU. Through attendance in these trainings, I will be able to further enhance my emotional intelligence as I learn how to support patients who are experiencing fear and anxiety when undergoing medical interventions in the ICU.
Critical reflection is not only limited to personal development but also in improving team functioning [4]. Team reflection can help members evaluate their own roles and the roles of the team members. In turn, this will help them identify the individual strengths and weaknesses of the team. In the next section of this essay, a discussion will be made on leadership within the team.
Leadership within a team
Effective leadership is crucial in ensuring that patients receive optimal care and achieve positive health outcomes [2]. Key characteristics of effective leaders include excellent communication skills and high emotional intelligence [33]. In healthcare settings, effective communication is a crucial component in providing quality care [4]. Leaders have to communicate with team members, patients and family members during healthcare decisions and when providing patient education [33]. Communication is also required when coordinating care with other members of the nursing team or multidisciplinary team. Hence, the ability to communicate effectively is a key characteristic of effective leaders. Effective leaders are also known to promote change through identifying the factors that promote and deter change and helping team members accept change in practice [33]. Promotion of change would require empowering team members to be responsible and accountable on the quality of care delivered to the patients. Empowerment would involve supporting the members in their roles and offering educating and training to enhance skills and knowledge necessary for patient care [35]. Effective leadership should also have the ability to articulate a clear vision to their team members [2].
In clinical settings, a team is described as a unit that is composed of at least two or more individuals who coordinate their work in order to achieve the goals of the team [36]. In application to nursing practice, a team may be described as a nursing team or a multidisciplinary team [4]. A nursing team is composed of nurses, patients, advanced nurse practitioners, nurse managers and healthcare assistants [37]. Meanwhile, a multidisciplinary team comprises of nurses, occupational therapists, physical therapists, nutritionists, dietitians, social care workers and other health and social care professionals who work together to optimise the care received by a patient [37]. Multidisciplinary teams are often formed to address the needs of patients with long-term conditions. In ICU settings, a nursing team is present to lead care and to refer cases to healthcare specialists.
Teams may be formed to offer support to patients with long term conditions or they may be established in acute care settings to address immediate healthcare needs of patients and their family members [37]. Tuckman’s model on how teams are formed suggests that there are five stage processes that teams undergo [37]. In the first stage, teams are formed and members start to define the goals of the team and the strategies required to reach these goals. In this stage, members are beginning to develop trust. In the second stage, which is called storming, team members may experience conflicts as they adjust to their new team roles. In the third stage or norming, members have spent sufficient time to accept their roles and the team’s expectations for their members. In the performing stage or fourth stage, team members are able to resolve conflicts more easily since members have developed attachments. Team members are able to understand how the team works and the factors that could deter teamwork. In the fifth stage or adjourning stage, teams have achieved their original goals and hence, working together is no longer necessary.
In the UK and Republic of Ireland, ICU nursing teams have been increasingly recognised as pivotal in the success or failure in the delivery of patient care. These nurses do not only coordinate care but also act as leaders and patient advocates [5]. The ICU nursing teams also collaborates with other nursing teams in the care of the patient. For example, ICU nurses have to coordinate care with ward nurses once patients are discharged from the ICU to the medical ward. However, unclear roles and hierarchies within healthcare settings could deter effective teamwork [38]. The lack of coordination and respect of team roles could result to conflicts, which can result to fragmentation of care [4]. Effective leadership is important in addressing fragmentation of care. This can be done through collaboration and practising the transformational leadership style. It has been shown that transformational leadership style could improve communication between team members, which in turn will help them discuss their team roles and how to address the challenges facing the team [35]. Further, transformational leadership will help empower members to achieve the team goals.
In healthcare settings, common leadership problems include managing team members and stakeholders, developing team members, inspiring others and leading a team [4]. Addressing these challenges would require the ability to delegating tasks, clearly establishing goals of the team, communicating expectations to team members and getting feedback to improve leadership [37]. Apart from these challenges, conflicts could also deter teams from attaining their goals. However, in clinical practice, conflicts are often seen as necessary to help team members examine different perspectives on patient care. Hence, not all conflicts are negative to the team. Instead, the ability to show empathy to different team members and understanding their own perceptions on a health issue could help resolve conflicts within teams [35].
In the case study, the team experienced little to no conflicts since the ICU is a highly complex and dynamic system that requires healthcare practitioners to receive sufficient training and education. This means that role ambiguity is addressed and the roles of each member in the team have been clarified prior to coordinating care of a critically ill patient. However, there are still instances where hierarchies exist. The differences in the professional background of the members could contribute to these hierarchies, which in turn can affect the quality of patient care [28]. Some nurses may choose not to participate in decision-making on patient care especially when specialists and trained surgeons or physicians are leading the team. This lack of participation is associated with feelings of being lesser than physicians and other specialists [28]. When nurses perceive that hierarchies are present, this could affect teamwork and communication with the team. In my personal experience, presence of hierarchy in the ICU could lead to conflicts and poor teamwork.
During the care of Mohammed in the ICU, I learned that some elements in patient care were missing. These included being more assertive when providing care and referring cases to the cardiologist [37]. This quality will help address concerns of hierarchy and power. I also learned that hierarchical structures could be addressed through valuing the contributions of all members in the team [36]. I also learned the importance of collaboration. When concerns are raised, involvement of several members of the team could help resolve these concerns [36]. In addition, communication is another area that should be further enhanced. Although nurses often receive training on how to develop therapeutic communication skills, these skills are not sufficient when communicating with other team members who have different professional backgrounds [4]. The type of communication between team members should involve respect and trust. Once effective communication is practised, this could lead to better health outcomes and increased willingness to identify solutions to healthcare issues and concerns [39].
Meanwhile, power is another important issue in the ICU and other healthcare settings. According to Miller T, et al. [40], power is defined as the ability to use or acquire and create resources that will help achieve personal and team goals. The case study presented in this essay shows that healthcare resources were readily available in the ICU and in the Cardiac Catheter Laboratory. Hence, it would have been easy to acquire these resources to achieve the team goals. However, the roles of the team members and their expected contributions influenced their ability to use resources within the ICU. For example, referral to the Cardiac Catheter Laboratory was dependent on the evaluation of the entire team and not only limited to a single member. Cardiologists have ready access to the Cardiac Catheter Laboratory and could use this resource in improving the health outcomes of Mohammed. The ease of access to the Cardiac Catheter Laboratory was due to the power and professional background of the cardiologist. In my ICU setting, inter-professional teamwork enabled the delivery of quality care. However, miscommunication could still occur during the care of patients in the ICU due to the highly dynamic natures of the environment. Hence, it is necessary to improve inter-professional teamwork since this could help members create policies, guidelines and clinical pathways that would be used to address the needs of critically ill patients.
Discussion and Conclusion
Effective leadership is critical when addressing the needs of critically ill patients. The transformational leadership style has been shown to be effective in helping team members feel valued and empowered to achieve team goals. Leaders demonstrating this style have high emotional intelligence and are able to show compassion and empathy to team members and patients. Since ICUs are highly dynamic, team members should be adequately prepared to meet the changing needs of patients in these settings. Hence, effective communication is necessary to coordinate and collaborate within the nursing team and with the multidisciplinary teams. The process of critical reflection could help identify gaps in practice and result to the creation of action plans that would improve patient outcomes.
Learnings I gained from this module is beneficial in my current practice as an ICU nurse. As a leader, I have learned the importance of effective communication, resolving conflicts and showing compassion and empathy to my colleagues and patients. I also learned the importance of transformational leadership and developing emotional intelligence to meet the needs of the patients by reading all materials posted by the module leader online The module also helped me develop my skills in critical reflection. In turn, this enhanced my ability to identify gaps in own practice and enhance my abilities as a nurse leader. I also learned how power could allow nurses to deliver high quality care. Finally, inclusion of trainings on how nurse leaders could support junior colleagues as they develop leadership traits and emotional intelligence could help improve the learning module.
REFERENCES
- Marshall E. Transformational leadership in nursing: from expert clinician to influential leader. London: Springer Publishing Company, UK. 2010.
- NHS Leadership Academy. Healthcare Leadership Model: The nine dimensions of leadership behavior. London: NHS Leadership Academy [Online]. 2013.
- Faculty of Intensive Care Medicine. Critical Capacity: A short research survey on critical care bed capacity. London: FICM, UK. 2018.
- Marquis B, Huston C. Leadership roles and management functions in nursing: theory and application. 7th ed. Philadelphia: Lippincott Williams & Wilkins, USA. 2012.
- Irish Association of Critical Care Nurses (IACCN) Your voice, represented. The National voice of critical care nurses. Ireland: IACCN [Online]. 2019.
- Nursing and Midwifery Council (NMC). The Code: Professional standards of practice and behaviour for nurses, midwives and nursing associates. London: NMC, UK. [Online]. 2018.
- Mellor P, Gregoric C. Ways of Being: Preparing Nursing Students for Transition to Professional Practice. Journal of continuing education in nursing. 2016; 47(7):330-340.
- Howatson-Jones L. Reflective practice in nursing. Exeter: Learning Matters. 2010.
- Coward M. Encouraging reflection in professional learning. Nursing Management. 2018.
- Rolfe G, Jasper M, Freshwater D. Critical reflection in practice: Generating knowledge for care. 2nd ed. Hampshire: Palgrave Macmillan, UK. 2011.
- Shirey M. Leadership practices for healthy work environments. Nursing Management. 2017;48(5):42-50.
- Goulet M, Larue C, Alderson M. Reflective practice: A comparative dimensional analysis of the concept of nursing and education studies. Nursing Forum. 2016; 51(2):139-150.
- Fragkos K. Reflective practice in healthcare education: An umbrella review. Education Sciences. 2016;6(3):1-16.
- Walker L, Avant K. Strategies for theory construction in nursing. 4th ed. Upper Saddle River, New Jersey: Prentice Hall, USA. 2005.
- Galutira G. Theory of reflective practice in nursing. International Journal of Nursing Practice. 2018; 8(3):51-56.
- Edwards S. Reflection differently, new dimensions: Reflection-before-action and reflection-beyond action. International Practice Development Journal. 2017;7(1): 1-14.
- Armstrong D, Asselin M. Supporting faculty during pedagogical change through reflective teaching practice: An innovative approach. National League for Nursing. 2017.
- Bulman C, Shutz S. Reflective practice in nursing. 5th ed. West Sussex: John Wiley and Sons, NY, USA. 2013.
- Pisanos D. Emotional intelligence: It’s more than IQ. Journal of Continuing Education. 2011;42(10):439-440.
- Raghubir A. Emotional intelligence in professional nursing practice: A concept review using Rodgers’s evolutionary analysis approach’, International Journal of Nursing Sciences. 2018;5(2): 126-130.
- Renaud M, Rutledge C, Shepherd L. Preparing emotionally intelligent doctor of nursing practice leaders’, Journal of Nursing Education. 2012;51(8):454-460.
- Bulmar Smith K, Profetto-McGrath J, Cummings G. Emotional intelligence and nursing: An integrative literature review. International Journal of Nursing Studies. 2009;46(12):1624-1636.
- Lopes P. Emotional intelligence in organizations: bridging research and practice. Emotion Review. 2016; 8(4):316-321.
- Thomsen D, Tonnesvang J, Schnieber A, et al. Do people ruminate because they haven’t digested their goals? The relations of rumination and reflection to goal internalization and ambivalence. Motivation and Emotion. 2011;35:105-117.
- Rosete D, Ciarrochi J. Emotional intelligence and its relationship to workplace performance outcomes of leadership effectiveness. Leadership and Organization Development Journal. 2005;26(5):388-399.
- Leary M, Reilly M, Brown F. A study of personality preferences and emotional intelligence. Leadership and Organization Development Journal. 2009;30(5): 421-434.
- Nabih Y, Metwally A, Nawar Y. Emotional intelligence as a predictor of leadership effectiveness. The Business and Management Review. 2016;7(5):133-142.
- Grossman S, Valiga T. The new leadership challenge: Creating the future of nursing. 3rd ed. Philadelphia: FA Davis. 2009.
- Clavelle J, Drenkard K, Tullai-McGuinness S, et al. Transformational leadership practices of chief nursing officers in Magnet organizations. Journal of Nursing Administration. 2012;42(4):195-201.
- Lin P, MacLennan S, Hunt N, et al. The influence of nursing transformational leadership style on the quality of nurses’ working lives in Taiwan: A cross-sectional quantitative study. BioMed Central Nursing. 2015;14:33.
- Gibbs G. Learning by doing: A guide to teaching and learning methods. London: Further Education Unit. 1988.
- Belbin M. Team roles at work. 2nd ed. Oxford: Routledge. 2012.
- Kourkouta L, Papathanasiou I. Communication in nursing practice. Mater Sociomedicine. 2014;26(1):65-67.
- Chlan L, Savik K. Patterns of anxiety in critically ill patients receiving mechanical ventilatory support. Nursing Research. 2011;60(3): 50-57.
- Mckimm J, Phillips K. Leadership and Management in Integrated Services. Learning Matters. 2009.
- Nash S, Govier I. Effective team leadership: techniques that nurses can use to improve team-working. Nursing Times. 2009;105(19):22-24.
- Huber D. Leadership and nursing care management. 4th edition. Philadelphia: W. B. Saunders. 2010.
- Hewison A, Morrell K. Leadership development in the English National Health Service: A counter narrative to inform policy. International Journal of Nursing Studies.2014; 51(4): 677-688.
- Brown J, Lewis L, Ellis K, et al. Conflict on interpersonal primary health care teams- can it be resolved. Journal of Interprofessional Care. 2011;25(1): 4-10.
- Miller T, Trubyk S. Kelly P, et al. Nursing Leadership and Management. Toronto: Nelson Education Ltd. 2016; 356-358.