Colonic volvulus in children: A single center experience
2 Department of Obstetrics and Gynecology, Enugu State University Teaching Hospital, Enugu, Nigeria
Received: 23-Feb-2022, Manuscript No. puljphcm-22-4361; Editor assigned: 28-Feb-2022, Pre QC No. puljphcm-22-4361; Accepted Date: Mar 26, 2022; Reviewed: 12-Mar-2022 QC No. puljphcm-22-4361; Revised: 23-Mar-2022, Manuscript No. puljphcm-22-4361; Published: 30-Mar-2022, DOI: 10.37532/puljphcm.2022.5(2).19-22
Citation: Emeka CK, Nnanyereugo OL, Patrick AL. Colonic volvulus in children: A single center experience. J Pedia Health Care Med. 2022; 5(2):19-22.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Colonic volvulus is an uncommon cause of bowel obstruction in children. The aim of this study was to evaluate our experience in the management of children who were confirmed to have colonic volvulus at surgery. Materials and Methods: This was a retrospective study of children aged 15 years and below who were managed for volvulus of the colon over a 10 year period at the pediatric surgery unit of a tertiary hospital in Enugu, Nigeria.
Results: Over the study period, 5 cases of colonic volvulus were confirmed at surgery and managed appropriately. Four were male and one was female. The mean age of the patients was 14 years. Abdominal pain was the consistent presenting symptom in all the patients. All the patients had abdominal x-ray and abdominal ultrasound. However, abdominal x-ray was only suggestive of colonic volvulus in patients with sigmoid volvulus. Abdominal ultrasound was not diagnostic in any of the patients. Intra-operatively, three (60%) patients had sigmoid volvulus, one (20%) had cecal volvulus and there was one (20%) volvulus of the transverse colon. All the patients had resection of the involved colon. Four (80%) patients had bowel resection with primary anastomosis but one (20%) patient (with sigmoid volvulus) required a temporary colostomy. None had colonoscopy because of absence of the facility. Surgical site infection was the most common post-operative complication. There was no mortality.
Conclusion: Sigmoid volvulus is more common than cecal and transverse volvulus. Imaging investigation may be helpful in making a diagnosis; however, confirmation can only be made at surgery. A high index of suspicion is required for early diagnosis and treatment.
Keywords
Children; Colonic volvulus; Sigmoid; Resection; Anastomosis
Introduction
Colonic volvulus occurs when a mobile portion of the colon twists around a fixed base causing obstruction of a segment of the colon at the point of maximum torsion. It is a closed loop obstruction [1]. When compared with midgut volvulus, colonic volvulus is a very rare cause of pediatric bowel obstruction [2]. Colonic obstruction accounts for about 10% of all mechanical obstruction of the intestinal tract and is the third leading cause of large bowel obstruction [1, 3]. The most common sites of colonic volvulus are in the sigmoid and cecal area [1]. One study from New York, United States of America reported the incidence of colonic volvulus as follows: sigmoid volvulus (60.9%), cecal volvulus (34.5%) and transverse volvulus (3.6%) [4]. The definitive diagnosis of colonic volvulus is usually made intra-op. Volvulus of the colon is a rare surgical emergency and the diagnosis is challenging to the surgeon. Clinical features such as nausea and vomiting are late symptoms because the obstruction is distal in the intestinal tract and physical examination findings are non-specific. High index of clinical suspicion allows early diagnosis of colonic volvulus and avoidance of morbidity and mortality associated with delayed diagnosis [5]. The population of patients mostly affected by colonic volvulus resides in the “Volvulus Belt” of Africa, the Middle East, India and Russia. In this volvulus belt, volvulus occurs at a younger age. Unlike in adults where colonic volvulus is more common in patients with neuropsychiatric disorders and in those in nursing home facilities, pediatric volvulus is more common in chronic constipation and mega colon [1]. The aim of this study was to evaluate our experience in the management of children who were confirmed to have colonic volvulus at surgery.
Materials and Methods
This was a retrospective study of children aged 15 years and below who were managed for volvulus of the colon between January 2011 and December 2020 at the pediatric surgery unit of Enugu State University Teaching Hospital (ESUTH) Enugu, Nigeria. Patients who had volvulus of the cecum, transverse and sigmoid colon were recruited into the study. Patients older than 15 years of age and those whose colonic volvulus could not be confirmed intra-op were excluded from this study. ESUTH is a tertiary hospital located in Enugu, South East Nigeria. The hospital serves the whole of Enugu State, which according to the 2016 estimates of the National Population Commission and Nigerian National Bureau of Statistics, has a population of about 4 million people and a population density of 616.0/km2. The hospital also receives referrals from its neighboring states. Information was extracted from the case notes, operation notes, and operation register and admission-discharge records. The information extracted included the gender, age at diagnosis, presenting symptoms, duration of symptoms before presentation, time interval between presentation and intervention, intra-operative finding, operative procedure performed, complications of treatment, duration of hospital stay and outcome of treatment. The follow-up period was 10 months. Ethical approval was obtained from the ethics and research committee of ESUTH and informed consent was not obtained from the patients’ caregivers due to the retrospective nature of the study and identities of the patients were not revealed. Statistical Package for Social Science (SPSS) version 21 (manufactured by IBM Corporation Chicago Illinois) was used for data entry and analysis. Data were expressed as percentages, mean, and range.
Results
Patients’ characteristics
Over the 10 year study period, 5 cases of colonic volvulus were confirmed at surgery and managed appropriately. Four were male and one was female. Details of the patient’s characteristics are shown in Table 1.
TABLE 1
Patient’s characteristics
| Parameter | Value |
|---|---|
| Mean age of the patients | 13 years (12-14) |
Gender
|
4 (80%) 1 (20%) |
| Mean interval between onset of symptoms and presentation | 4 days (2-5) |
| Mean interval between presentation and surgery | 2 days (1-3) |
| Duration of hospital stay | 10 days (7-14) |
Presenting symptoms of the patients
All the patients presented with abdominal pain. This abdominal pain was worse on lying supine and relieved by sitting upright. Other presenting symptoms are shown in Table 2.
TABLE 2
Presenting symptoms
| Symptoms |
Number of patients (%) |
|---|---|
| Abdominal pain |
5 (100%) |
| Abdominal distension |
4 (80%) |
| Vomiting |
3 (60%) |
| Constipation |
2 (40%) |
| Non-specific symptoms (e.g. weakness, anorexia etc.) |
1 (20%) |
Investigations performed
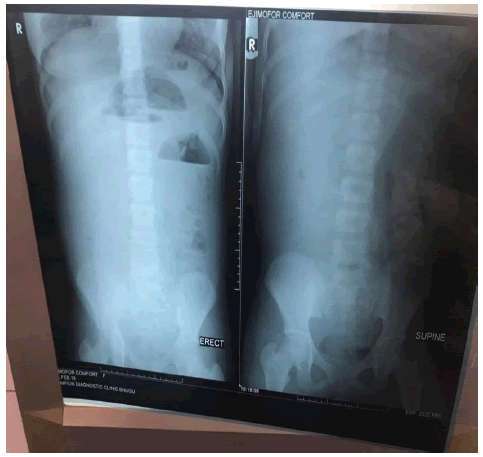
All the patients had plain abdominal radiograph and abdominal ultrasound. Plain abdominal radiograph could diagnose sigmoid volvulus but not in transverse volvulus or in cecal volvulus. Figures 1 and 2 shows the radiograph of one of the patients with sigmoid volvulus with the positive coffee bean sign. Abdominal ultrasound was not diagnostic in any of the patients.
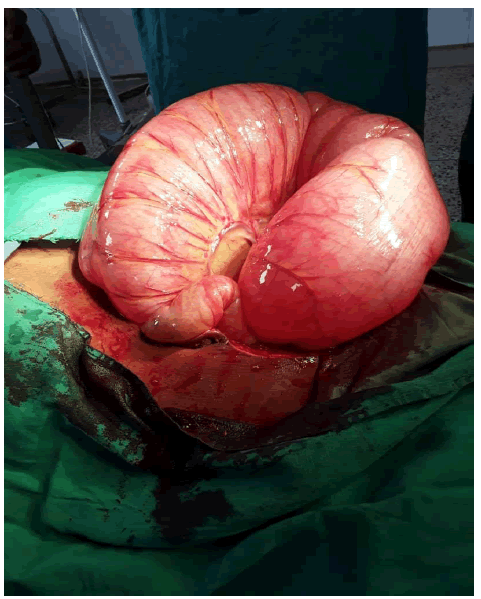
Intra-operative finding
Three (60%) patients had sigmoid volvulus, one (20%) had cecal volvulus and there was one (20%) volvulus of the transverse colon. Figures 3 and 4 show the intra-operative picture of the patients that had sigmoid volvulus and cecal volvulus respectively.
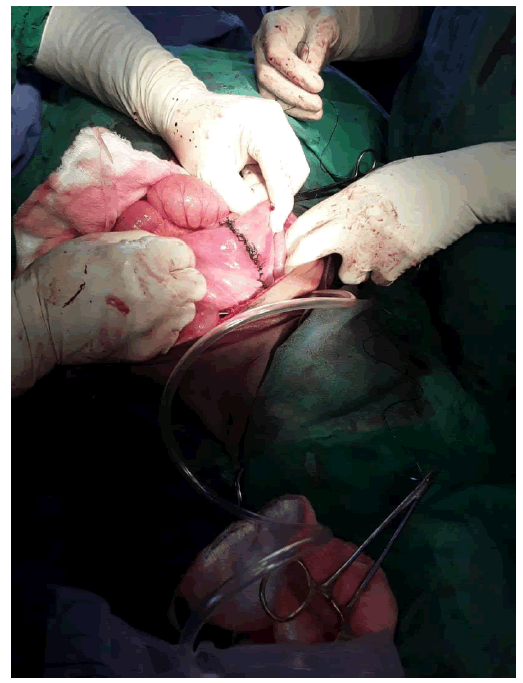
Operative procedure performed
All the patients had resection of the involved colon. Four (80%) patients had bowel resection with primary anastomosis but one (20%) patient (with sigmoid volvulus) had a temporary colostomy. None had colonoscopy because of absence of the facility. Figure 5 shows the anastomotic site following bowel resection and anastomosis of a patient with sigmoid volvulus.
Complications of treatment
Surgical site infection was the most common post-operative complication. Other complications are reflected in Table 3.
TABLE 3
Complications of treatment
|
Post-operative complications |
Number of patients (%) |
|---|---|
|
Surgical site infection |
2 (40%) |
|
Intra-abdominal abscess |
1 (20%) |
|
Adhesive bowel obstruction |
1 (20%) |
Outcome of treatment and associated anomaly
All the patients achieved good recovery and there was no mortality. The entire resected specimens (colon) were sent for histopathological examination. However, the histology of one of the patients who had sigmoid volvulus showed absence of ganglion cells which suggest an underlying Hirschsprung’s disease. All other histologies were essentially normal.
Discussion
The word “volvulus” is derived from the Latin “volvere” which means to twist. In colonic volvulus, there is twisting of the colon in a manner leading to bowel obstruction and if left untreated, may lead to ischemia and gangrene [1]. There are ancient documentations of colonic volvulus. The Papyrus Ebers, 1550 BC, described the natural course of volvulus to be spontaneous reduction or “rotting” of the bowel [4]. In the book “Affections”, Hippocrates published that the treatment for volvulus involved injecting a large quantity of air into the intestines through the anus. In the book entitled “Diseases”, Hippocrates also advocated the insertion of suppositories 10 digits (approximately 22 cm) long [4]. Twenty-first century, endoscopic decompression of colonic volvulus uses instruments of comparable length [1]. In 1841, Rokitansky described volvulus as a cause of intestinal strangulation. This was the first mention of colonic volvulus in western literature [6]. Atherton in 1883, described laparotomy and lysis of adhesion for the treatment of volvulus. In mid-20th century, surgical management became the mainstay of treatment of colonic volvulus [1]. In 1947, Brusgaard described decompression of sigmoid volvulus through sigmoidoscopy and placement of rectal tube in patients without peritonitis [7].
In the present study, the mean age of the patients was 13 years. This finding is comparable to the report of other series on pediatric colonic volvulus [3, 5]. Salas and colleagues reviewed the past 50 years of the literature related to pediatric colonic volvulus and they found the median age of the patients to be 7 years. Colonic volvulus has also been reported in newborns as young as 4 hours old [2]. More males were involved in the current series. This male predominance is consistently reported by other authors [8]. The reason for the male predominance is not known. However, Carmo et al published a case report of sigmoid volvulus in a 16-year old female teenager [5]. None of the patients in the current study presented within 24 hours of onset of their symptoms. The insidious and intermittent onset of symptoms of colonic volvulus may explain this delayed presentation. Also, the rarity and non-classical presentation of colonic volvulus in children may have delayed referral by the general medical practitioners. Moreover, colonic volvulus may self-rectify [9]. Similar to small bowel volvulus, delay in diagnosis of colonic volvulus can result in bowel ischemia, perforation and peritonitis [10]. Laparotomy for the patients in the current series was not performed emergently. This is due to the fact that the diagnosis of colonic volvulus could not be made clinically; imaging investigation was required and the diagnosis confirmed at surgery.
Abdominal pain is the consistent presenting complaint in children with colonic volvulus. The abdominal pain may be intermittent if there are periods of spontaneous untwisting of the volvulus. The exact reason why the abdominal pain is relieved by sitting upright is not clear. However, the release of pressure on the abdominal viscera, when the patient sits, may explain it. In chronic cases of colonic volvulus, the symptoms may be vague [5]. Tannouri et al reported abdominal pain and abdominal distension as the most common presenting symptoms in pediatric colonic volvulus [11]. The part of the colon involved in the volvulus may determine the degree of abdominal distension. For instance, there will be more abdominal distension in the sigmoid volvulus than in cecal volvulus.
Generally, imaging investigations in colonic volvulus show the presence of bowel obstruction evidenced by dilated bowel loops and air-fluid levels. However, in sigmoid volvulus the markedly dilated sigmoid loops with bent inner tube appearance are seen. Other radiological features of sigmoid volvulus include bird peak sign, coffee bean sign, ace of spade sign, omega or horse shoe sign, inverted V sign, Y sign and northern exposure sign [12]. Sigmoid volvulus is differentiated from cecal volvulus by its austral wall [13].
The diagnosis of colonic volvulus is confirmed at surgery; particularly in cecal and transverse colonic volvulus where imaging investigation may only be suggestive of large bowel obstruction. It is pertinent to state that most diagnoses of colonic volvulus are made intra-op. Four-fifth (80%) of the patients had large bowel resection and primary colo-colic anastomosis. However, one-fifth (20%) had a sigmoid colostomy. The indication for the colostomy was gross peritoneal contamination following gangrene and perforation of the sigmoid colon. Other researchers have also reported the role of temporary colostomy in the management of colonic volvulus when there is necrotic bowel [14, 15].
Surgical site infection was the most common post-operative complication encountered in our patients. This finding is consistent with the report of other published works on colonic volvulus [16, 17]. The high bacterial and fecal loads encountered in colonic surgeries may explain the occurrence of wound infections.
The overall outcome of management of colonic volvulus is good. No mortality was recorded in the present study. Howbeit, Salas et al reported overall mortality of 6% and emphasized on the association between colonic volvulus and Hirschsprung’s disease [2]. In fact, one study from Ethiopia documented that Hirschsprung’s disease may present as sigmoid volvulus [18].
Conclusion
Volvulus of the large bowel is an uncommon cause of bowel obstruction in children. Sigmoid volvulus is more common than cecal and transverse volvulus. Imaging investigation may be helpful in making a diagnosis; however, confirmation can only be made at surgery. Options of treatment of colonic volvulus include endoscopic decompression (when available), bowel resection with primary anastomosis/temporary colostomy. A high index of suspicion is required for early diagnosis and treatment.
REFERENCES
- Gingold D, Murrel Z. Management of colonic volvulus. Clin Colon Rectal Surg. 2012; 25(4): 236-244.
Google Scholar Cross Ref - Salas S, Angel CA, Salas N, et al. Sigmoid volvulus in children and adolescents. J Am Coll Surg. 2000; 190(6): 717-723.
Google Scholar Cross Ref - Al-Doud MA, Al-Omari MA, Dboush HG, et al. Large bowel obstruction as a consequence of transverse colon volvulus: A case report. Int J Surg Case Rep. 2020; 76: 534-538.
Google Scholar Cross Ref - Ballantyne GH. Review of sigmoid volvulus: history and results of treatment. Dis Colon Rectum. 1982; 25(5): 494-501.
Google Scholar Cross Ref - Carmo L, Amaral M, Tridade E, et al. Sigmoid volvulus in children: Diagnosis and therapeutic challenge. GE Proct J Gastroenterol. 2018; 25(5): 264-267.
Google Scholar Cross Ref - Von Rokitansky C. Manual of pathological anatomy. Braumuller and Seidel. 1846; 1:1804-1878.
Google Scholar Cross Ref - Brusgaard C. Volvulus of the sigmoid colon and its treatment. Surgery. 1947; 22(3): 466-478.
Google Scholar Cross Ref - O’ Keefe LM, Hu YY, Thaker S, et al. Sigmoid volvulus: A pediatric case report and review of management. J Pediatr Surg Case Rep. 2016; 7: 4-7.
Google Scholar Cross Ref - Ismail A. Recurrent colonic volvulus in children. J Pediatr Surg. 1997; 32(12): 1739-1742.
Google Scholar Cross Ref - Altaf MA, Werlin SL, Sato TT, et al. Colonic volvulus in children with intestinal motility disorders. J Pediatr Gastroenterol Nutr. 2009; 49(1): 59-62.
Google Scholar Cross Ref - Tannouri S, Hendi A, Gilje E, et al. Pediatric colonic volvulus: A single-institution experience. And review. J Pediatr Surg. 2017; 52(6): 1062-1066.
Google Scholar Cross Ref - Singh Y, Islam S, Arra A, et al. The steel pan sign of sigmoid volvulus-A case series. Int J Surg Case Rep. 2017; 41: 332-555.
Google Scholar Cross Ref - Jaffe T. Thompson WM. Large-bowel obstruction in the adult: classic radiographic and ct findings, etiology, and mimics. Radiol. 2015; 275(3): 651-663
Google Scholar Cross Ref - Chalya PL, Mabula JB. Sigmoid volvulus and ileo-sigmoid knotting: A five-year experience at a tertiary care hospital in Tanzania. World J Emerg Surg. 2015; 10(10): 1-8.
Google Scholar Cross Ref - Destro F, Maestri L, Meroni M, et al. Colonic volvulus in children: Surgical management of a challenging condition. Children. 2021; 8: 982.
Google Scholar Cross Ref - Mulugeta GA, Awlachew S. Retrospective study on pattern and outcome of management of sigmoid volvulus at district hospital in Ethiopia. BMC Surg. 2019; 19.
Google Scholar Cross Ref - Emna T, Atef M, Sarra S. Management of acute sigmoid volvulus: A tunisian experience. Asian J Surg. 2021; S1015-S9584(21)00210-4.
Google Scholar Cross Ref - Gosaye AW, Nane TS, Negussie TM. A case report of Hirschsprung’s disease presenting as sigmoid volvulus and literature review. Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. BMC Surg. 2021; 21: 109.
Google Scholar Cross Ref