Combining manual lymph drainage with physical exercise after modified radical mastectomy effectively prevents axillary web syndrome
2 The department of Breast Cancer, Collaborative Innovation Center for Cancer Medicine, Guangzhou, China
3 The department of chemotherapy, Collaborative Innovation Center for Cancer Medicine, Guangzhou, China
4 The Institute for Cancer Research, Collaborative Innovation Center for Cancer Medicine, Guangzhou, China
Received: 17-Sep-2017 Accepted Date: Oct 13, 2017; Published: 16-Oct-2017
Citation: Xin M, Zhang H, Zhong Q, et al. Combining manual lymph drainage with physical exercise after modified radical mastectomy effectively prevents axillary web syndrome J Phlebol Lymphol. 2017;10(1):15-18.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Aim: To explore the effect of manual lymph drainage combined with physical exercise in preventing axillary web syndrome (AWS) after modified radical mastectomy. Background: In spite of the great progress achieved in mechanistic understanding, early detection, and adjuvant therapy, breast cancer remains the most common malignancy and the most common cause of death in women in China. AWS (aches in the upper limbs, tension at shoulder abduction, palpable cord structures, etc.) is a common early complication in breast cancer patients after axillary lymph node dissection, which reduces the quality of life of breast cancer survivors. Physical exercise is the traditional way to prevent postoperative complaints, whereas manual lymph drainage is relatively novel and is less frequently used, and its effects have not been determined. Design: A randomized controlled study. Methods: With approval from the Ethics Committee of Sun Yat-sen University (Guangzhou, China) and written informed consent obtained from all participating patients, four hundred women breast cancer patients were randomly divided into two groups (n=200/group) to receive either physical exercise alone(PE group) or self-administered manual lymph drainage as well as physical exercise(MLD group) after surgery. The presence of AWS was assessed at one, two and three months after surgery. Result: The occurrence rates in the two groups both gradually decreased over time. The numbers of patients with AWS in the PE and MLD groups at one month were 20 and 7(Pï¼ÂÂœ0.05), respectively, at two months were 29 and 5(Pï¼ÂÂœ0.01), respectively, and at three months were22 and 3(Pï¼ÂÂœ0.01), respectively. Conclusions: MLD in combination with physical exercise is beneficial for preventing AWS and increasing comfort in breast cancer patients after modified radical mastectomy.
Keywords
Breast cancer, manual lymph drainage, axillary web syndrome, modified radical mastectomy
Introduction
Axillary web syndrome (AWS) is one type of Mondor disease [1]. It is an early post-operative complication of breast cancer secondary to axillary lymph mode dissection (ALND) or sentinel lymph node biopsy (SLNB), and it can also occur in non-breast cancer patients with axillary node biopsies [2]. AWS is characterized by postoperative sudden upper limb pain that is aggravated when abducting the shoulder, with associated traction, tightness, and palpable cords in the subcutaneous tissue in the breast, axilla, medial arm, antecubital space, forearm, hand, and/or chest wall. There are no related complaints or symptoms preoperatively [3,4].
AWS is self-limited with sudden onset [5].The typical syndrome limits shoulder and elbow range of motion (ROM), affecting the quality of life of breast cancer survivors [6]. Patients and caregivers in China often lack knowledge of AWS. They tend to believe that the subcutaneous cords are caused by cancer metastasis or recurrence, which increases their psychological burden and is not conducive for postoperative physical and mental rehabilitation.
AWS is not uncommon in clinical practice, and its incidence rate has been reported as 20% and38-72% following SLNB and ALND, respectively, in breast cancer patients [7-9]. Currently, the pathophysiology of AWS has not been extensively investigated, and there is no definitive treatment for AWS [4]. Medication and physiotherapy including ROM exercises were found to be ineffective in relieving AWS in breast cancer patients [5]. In China, research on this topic is very rare. Surgeons, physicians and nurses also lack the knowledge needed to suitably judge, treat and care for AWS. Physical exercise is the traditional and gold standard for improving function in postoperative breast cancer patients. Manual lymph drainage (MLD) is a new nursing technology used in mainland China for postoperative breast cancer survivors [10].
MLD has been shown to improve blood circulation, stimulate the movement of lymphatic and other tissue fluids, and promote fluid clearance and tissue softening [11]. Early stimulation of lymphatic drainage can also modulate the pain and inflexibility associated with lymphatic vessel inflammation secondary to surgical injuries [12]. The effect of MLD in breast cancer patients with AWS remains unknown.
The purpose of this study was to evaluate the effects of physical exercise therapy (PE) combined with MLD on AWS, in comparison to PE only, in breast cancer patients. At Sun Yat-sen University Cancer Center, we are dedicated to improving the quality of life of breast cancer patients after surgical treatment. In this study, we report our observations and experiences using MLD in combination with physical exercise for the prevention and relief of the symptoms of AWS in breast cancer patients after modified radical mastectomy compared with physical exercise alone.
Methods
Patients
This study was approved by the Ethics Committee of Sun Yat-sen University (Guangzhou, China), and written informed consent was obtained from all participating patients. Four hundred women with breast cancer scheduled for modified radical mastectomy at Sun Yat-sen University Cancer Center between June 2014 and December 2014 were recruited and randomly divided into either the physical exercise group (PE group, n=200) or the MLD combined with physical exercise (MLD group). All recruited patients met the following criteria:
(1) They fully knew their disease situation. (2) They had not yet received any treatment. (3) They were to receive modified radical mastectomy at SYSUCC. (4) They agreed to participate in the research study. (4) They had a good understanding of their disease and the study and had good communication abilities.
Exclusion criteria included the following:
(1) Patients who had symptoms similar to AWS like limb pain, tightness or subcutaneous cords. (2) Patients who were lost to follow-up. (3) Patients with diseases where PE or MLD could not be implemented and/or who used anti-depression or anti-anxiety drugs.
Treatments
Patients in both groups received health education24 hours before surgery, emphasizing the post-surgical complications and the importance of nursing interventions and self-management. After the patient regained consciousness from anesthesia, PE or MLD training was given by breast-specialist nurses daily for three days and on the day of discharge (20 - 30min/session, two sessions per day). The PE was designed based on the National Lymphedema Network (NLN) Position Papers released by the NLN (American) Medical Advisory Committee (http://www.lymphnet.org/le-faqs/nln-positon-papers). The PE training consisted of four stages of exercise with varying focuses, based on the postoperative time course and clinical management. Table 1 gives an overview of the different stages, their times, and training focus.
| Stages | Times | Training focus |
|---|---|---|
| The first stage | The surgery day to the days before removal of the drainage tube (≤ 7 days) | Begin with passive exercise. Keep affected limb relaxed; abduct and lift limb; move fingers, wrist, elbow joints softly, avoid using the affected limb to support. |
| The second stage | Between removal of the drainage tube and removal of the surgical sutures (730 days) | Progress to localized active exercise; move shoulder joint softly; use fingers to touch ear and climb wall. |
| The third stage | Between the removal day of the sutures and three months after surgery | Increase the activity range of the shoulder joint. Abduct, lift and spin shoulder joint after softly massaging the shoulder and axilla. Patients can use the affected limb to comb hair, brush teeth, wash face, climb wall, buckle bra, bathe and other activities until affected limb can move normally. |
| The fourth stage | Between three months post-operation and half a year | Repeat the movement above and select some suitable aerobic exercise-eg., walking, climbing, swimming, Tai Ji, etc. But avoid vigorous activities. Patients should protect the affected limb, strictly avoiding using that limb to measure blood pressure, collect blood samples, intravenous infusion, lifting heavy things, swinging arm, etc. |
Table 1: Physical exercise guideline for post-operative breast cancer patients.
In the MLD group, in addition to the base PE training, patients also received guided instruction on MLD from the breast-specialist nurses starting from the day of surgery three times per day (morning, noon and evening) for 10 min sessions. Procedures were as follows:
(1) Open the lymphatic pathways: Patients were guided to stay relaxed during the whole process and to use mezzo strength (25 mmHg) to massage the superficial lymph nodes vertically with their thenar and hypothenar muscles or folded index, middle and ring fingers.
The massage order was preauricular lymph nodes, retroauricular lymph nodes, submandibular lymph nodes, cervical lymph nodes, supraclavicular lymph nodes, infraclavicular lymph nodes, axillary lymph nodes,shoulder lymph nodes, elbow lymph nodes, back lymph nodes and finally the inguinal lymph nodes.
(2) Lymph drainage: Patients were guided to massage the affected limb distally too proximally along the superficial lymph nodes with stationary circles, rotary propulsion or scooping propulsion techniques. The order was as follows: starting with the chest wound, drain the lymph above the wound to the contralateral infraclavicular or axillary lymph nodes; drain the inside lymph of the upper palmar forearm through the lateral forearm to the supraclavicular lymph nodes; drain the inside lymph of the dorsal forearm through the lateral forearm to the dorsal axillary lymph nodes or back through to the ipsilateral inguinal lymph nodes; drain the lymph of the opisthenar, palm, forearm and cubital fossa to the outside of forearm. The massage was to be gentle to prevent redness of the local skin.
Assessment
Social-demographic data, including name, age, level of education, marriage status, career, family monthly income and health insurance, etc., and clinico-pathologic data, including tumor pathology and clinical staging, were collected by the self-designed questionnaire. The questionnaire was filled out by the breast-specialist nurses who provided the education and who had undergone training before the study. AWS was assessed in each patient at one week and at one, two, and three months after surgery. AWS signs and symptoms consisted of pain, traction, and tightness at rest or with abducted shoulders and palpable subcutaneous cords in the breast, axilla, medial arm, antecubital space, forearm, hand, and/or chest wall.
Statistical analysis
All data analysis was performed using the SPSS 17 statistical package for the social sciences (SPSS, Inc., Chicago, IL).Continuous and categorical variables were expressed as the means ± standard deviations and as percentages, respectively. Independent t-tests and Chi-square or Fisher’s exact tests were applied to compare baseline descriptive statistics and changes in continuous and categorical variables between the two groups. AP-value of <0.05 was defined as statistically significant.
Results
Baseline comparisons between the MLD and PE groups
Age, level of education, marriage status, career, family monthly income, tumor pathology, tumor-node-metastasis staging, levels of estrogen receptor and progesterone receptor, and lymph node metastasis were not significantly different between the MLD and PE groups. Thus, patients in the two groups were comparable at baseline. (In Table 2 all P0.05).
| Characteristics | PE group (n=200) No. (%) |
MLD group (n=200) No. (%) |
P value |
|---|---|---|---|
| Age(years) <50 ≥50 |
130 (65.0) 70 (35.0) |
113 (56.5) 87 (43.5) |
0.051 |
| Marital status Married Single/divorced/widowed |
145 (72.5) 55 (27.5) |
139 (69.5) 61 (30.5) |
0.291 |
| Educational level Middle school or below High school / vocational college Bachelor degree or above |
58 (29.0) 110 (55.0) 32 (16.0) |
52 (26.0) 112 (56.0) 36 (18.0) |
0.288 |
| Income <1000RMB ≥ 1000RMB |
52 (26.0) 148 (74.0) |
46 (23.0) 154(77.0) |
0.281 |
| Pathological subtypes IDCa Others |
173 (86.5) 27 (13.5) |
178 (89%) 22 (11.0) |
0.271 |
| Estrogen receptor status | 146 (73.0) 54 (27.0) |
155 (77.5) 45 (22.5) |
0.177 |
| Progesterone receptor status | 175 (87.5) 25 (12.5) |
178 (89.0) 22 (11.0) |
0.378 |
| HER2 status | 86 (43.0) 114 (57.0) |
90 (45.0) 110 (55.0) |
0.381 |
| Lymph node metastasis | 165 (82.5) 35 (17.5) |
172 (86.0) 28 (14.0) |
0.205 |
Table 2: Baseline socio-demographic and clinico-pathologic characteristics of the patients (a IDC, invasive ductal carcinoma).
Comparison of the incidence of AWS between the MLD and PE groups
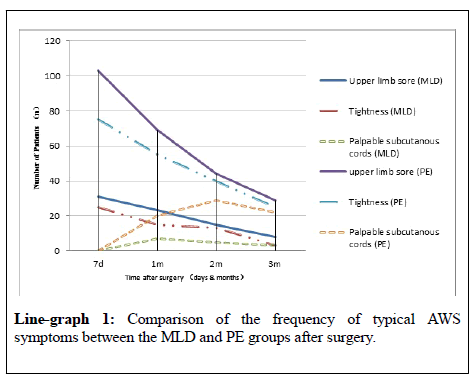
At the first week after surgery, no significant difference in the incidence of AWS was detected between the two groups. However, at one, two and three months after surgery, 7, 5 and 3 patients in the MLD group had AWS, respectively, and 20, 29 and 22 patients in the PE group had AWS, respectively. This suggests that MLD, when combined with physical exercise, is effective in reducing AWS (Table 3, all P < 0.05). The typical symptoms of AWS in the two groups were upper limb soreness, tightness and palpable subcutaneous cords. Incidences of these symptoms are shown in line-graph 1.
| Groups | One month | Two months | Three months |
|---|---|---|---|
| MLD group | 7/200 | 5/200 | 3/200 |
| PE group | 20/200 | 29/200 | 22/200 |
| Difference | 13 | 24 | 19 |
| P- value | 0.008 | <0.001 | <0.001 |
Table 3: Comparison of the incidence of AWS between the MLD and PE groups after surgery.
Discussion
In our study, we evaluated MLD in combination with physical exercise compared with physical exercise alone in the prevention of AWS in breast cancer patients after modified radical mastectomy. We found that patients in the MLD group had lower AWS incidence and lower rates of upper limb pain, tightness and cord occurrences during the follow-up period.
To the best of our knowledge, most previous studies regarding AWS have been case reports [4,13]. These studies implied that PE is a quick and effective method to remit AWS or lymphedema [14]. This is the first controlled study to evaluate MLD in breast cancer patients with AWS in mainland China. We chose to assess MLD, which is a well-known treatment method for lymphedema and AWS according to other studies that have demonstrated the effectiveness of MLD in other populations [4,15].
AWS has been reported to be associated with lymphovenous damage, lymphatic stasis, and tissue injury resulting from the disruption of superficial lymphatic structures during surgery, causing a high coagulation state of the surrounding tissue, with decreased lymphatic outflow, pipeline occlusion and inflammation [16]. Fortunately, during the postoperative healing phase, with lymphovenous reconstruction and recanalization, AWS symptoms will gradually disappear in two or three months [2]. In this study, the incidence of AWS at one, two, and three months was 10.0%, 14.5% and 11.0% in the PE group, respectively, and 3.5%, 2.5% and 1.5% in the MLD group, respectively. A systematic review has shown that the incidence of AWS was 0.6% to ~85.4% across studies with different surgical methods and related factors [17]. Therefore, further observation in different surgical styles is needed to determine the incidence of AWS to facilitate comparisons across different populations.
The typical symptoms of AWS, such as pain, tightness and palpable subcutaneous cords, limit daily life function. With a lack of knowledge of these complications, patients and caregivers tend to protect the surgical area, and AWS-induced pain can progressively restrain shoulder mobility. Additionally, these symptoms can cause patients to feel anxious about disease recurrence. For all of the above reasons, AWS can affect breast cancer survivor’s recovery from surgery and their quality of life [18].
As we know, PE based on the National Lymphedema Network (NLN) Position Papers is effective and welcomed worldwide. In Mainland China, PE has been the gold standard for nursing intervention in postoperative survivors. PE sessions have been demonstrated to improve symptoms, including decreased pain and restoration of full shoulder range of motion (ROM) [14]. Thus, a no-treatment control group was not included because we thought it would be unethical. MLD is a light, hands-on, touch massage. It works on superficial lymphatic vessels and tissue fluids in subcutaneous tissues [19]. As the results showed, MLD could be more effective in preventing or relieving AWS compared with PE alone. Additionally, no patient in either group was observed to have AWS during the first postoperative week, whereas the occurrence of upper limb pain and tightness were quite high in both groups. There was a positive correlation between the early occurrence of pain and tightness with later incidence of AWS, which indicates a potential warning sign for medical staff and patients. In this regard, patient education to identify early symptoms and signs associated with AWS, together with treatment with PE and MLD, are essential for timely diagnosis and early intervention [10].
There are several limitations in our study. First, we could not discern the natural course of AWS due to the lack of a true, no-treatment control group. Second, other adjunctive treatments were not screened during the entire follow-up period, which could be a potential confounder and may have had an impact on related symptoms. Finally, our study had a limited length of follow-up (only 3months). This was because of the time-limited quality of AWS; however, we had not observed the disappearance of all AWS and related symptoms by the end of our observation period. In conclusion, considering earlier studies regarding the prevention of lymphedema, MLD in combination with PE can be an effective strategy for preventing AWS and is a treatment needed for postoperative breast cancer survivors.
Conflict of Interest
None
Acknowledgements
We thank all patients for their contribution to the survey. Breast-specialist nurses for their technical guidance. This study was supported by the National Natural Science Foundation of China (No. 81472469), Sun Yat - sen Excellent Young Teacher Program (12ykpy15) and the CMB Excellent Young Teacher Program (10-020-201212).
REFERENCES
- Craythorne E, Benton E, Macfarlane S. Axillary web syndrome or cording, a variant of mondor disease, following axillary surgery. J Arch Dermatol. 2009;145(10):1199-1200.
- Leidenius M, Leppanen E, Krogerus L, et al. Motion restriction and axillary web syndrome after sentinel node biopsy and axillary clearance in breast cancer. Am J Surg. 2003;185(2):127-130.
- Leduc O, Fumiere E, Banse S, et al. Identification and description of the axillary web syndrome (AWS) by clinical signs, MRI and US imaging. Lymphology. 2014;47(4):164-176.
- Cho Y, Do J, Jung S, et al. Effects of a physical therapy program combined with manual lymphatic drainage on shoulder function, quality of life, lymphedema incidence, and pain in breast cancer patients with axillary web syndrome following axillary dissection. Support Care Cancer. 2015.
- Moskovitz AH, Anderson BO, Yeung RS, et al. Axillary web syndrome after axillary dissection. Am J Surg. 2001;181(5):434-439.
- Martins DSR, Rezende LF. Assessment of impact of late postoperative physical functional disabilities on quality of life in breast cancer survivors. Tumori. 2014;100(1):87-90.
- Bergmann A, Mattos I, Pedrosa E, et al. Axillary web syndrome after lymph node dissection: results for 1004 breast cancer patients. Lymphology. 2007;40:198-203.
- Fukushima KF, Carmo LA, Borinelli AC, et al. Frequency and associated factors of axillary web syndrome in women who had undergone breast cancer surgery: a transversal and retrospective study. Springerplus. 2015;4:112.
- Torres LM, Mayoral DMO, Coperias ZJ, et al. Axillary web syndrome after axillary dissection in breast cancer: a prospective study. Breast Cancer Res Treat. 2009;117(3):625-630.
- Zhang L, Fan A, Yan J, et al. Combining Manual Lymph Drainage with Physical Exercise after Modified Radical Mastectomy Effectively Prevents Upper Limb Lymphedema. Lymphat Res Biol. 2016.
- Devoogdt N, Christiaens M R, Geraerts I, et al. Effect of manual lymph drainage in addition to guidelines and exercise therapy on arm lymphoedema related to breast cancer: randomised controlled trial. BMJ. 2011;343:d5326.
- Torres LM, Yuste SM, Zapico GA, et al. Effectiveness of early physiotherapy to prevent lymphoedema after surgery for breast cancer: randomised, single blinded, clinical trial. BMJ. 2010;340:b5396.
- Wei P, Zhu L, Chen K, et al. Axillary web syndrome following secondary breast-conserving surgery: a case report. World J Surg Oncol. 2013;11:8.
- Fourie WJ, Robb KA. Physiotherapy management of axillary web syndrome following breast cancer treatment: discussing the use of soft tissue techniques. Physiotherapy. 2009;95(4):314-320.
- OToole J, Miller CL, Specht MC, et al. Cording following treatment for breast cancer. Breast Cancer Res Treat. 2013;140(1):105-111.
- Rashtak S, Gamble GL, Gibson LE, et al. From furuncle to axillary web syndrome: shedding light on histopathology and pathogenesis. Dermatology. 2012;224(2):110-114.
- Yeung WM, Mcphail SM, Kuys SS. A systematic review of axillary web syndrome (AWS). J Cancer Surviv. 2015;9(4):576-598.
- Martins DSR, Rezende LF. Assessment of impact of late postoperative physical functional disabilities on quality of life in breast cancer survivors. Tumori. 2014;100(1):87-90.
- Olszewski WL, Jain P, Ambujam G, et al. Topography of accumulation of stagnant lymph and tissue fluid in soft tissues of human lymphedematous lower limbs. Lymphat Res Biol. 2009;7(4):239-245.