Commentary on 'Pityriasis rosea-like eruption induced by isotretinoin'
Received: 07-Nov-2017 Accepted Date: Nov 29, 2017; Published: 07-Dec-2017
Citation: Gurel G. Commentary on 'Pityriasis rosea-like eruption induced by isotretinoin.' J Skin. 20178;2(1):1-2.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Recently in the Cutaneous and Ocular Toxicology Gurel et al. [1] published a case report describing pityriasis rosea-like eruption induced by isotretinoin. As Gurel et al. [1] emphasizes, Pityriasis rosea (PR) is a common, self-limited and inflammatory skin disease. PR-like eruption is a drug-induced skin rash with clinical features that strikingly resemble genuine PR and that often do not allow a clear distinction. In PR-like eruptions, prodromal systemic symptoms are absent; lesions are more confluent and diffuse than classic PR [2]. In 1984, Helfman et al. [3] reported a PR-like eruption in two patients with acne receiving isotretinoin.
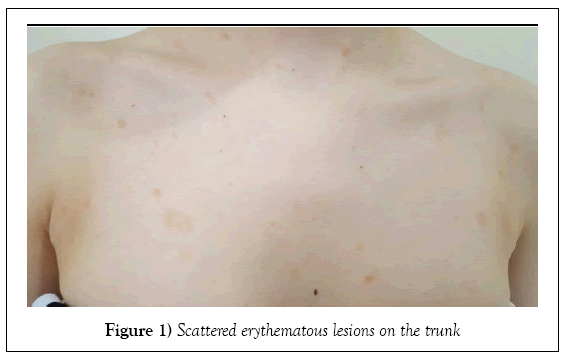
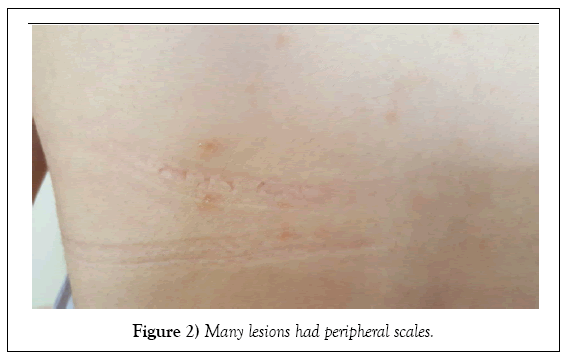
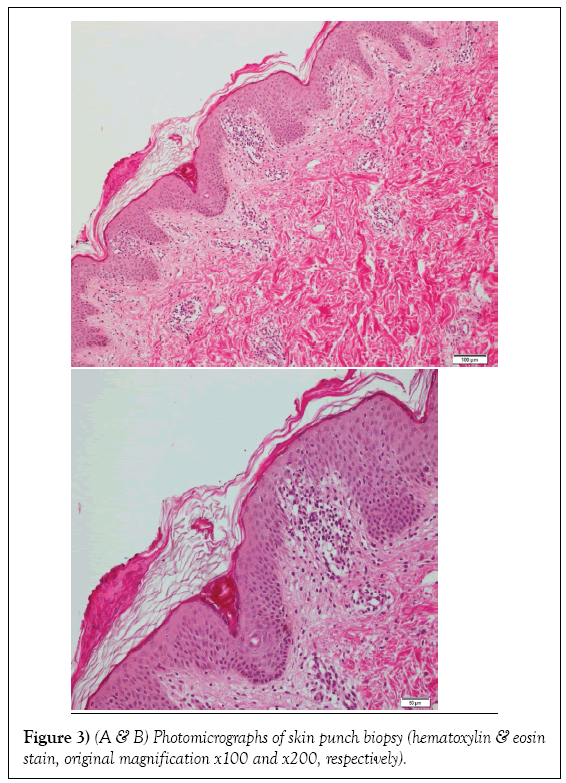
A 20 year old female patient had severe nodulo-cystic acne on the face of three years duration. The patient was started systemic isotretinoin at 40 mg/ day (0.7 mg/kg/d). There were no side effects except dryness in the first four months of the treatment. She was admitted to our clinic with a skin rash on her trunk that had developed approximately 5 days. Lesions were mild itching. She had no accompanying systemic disease and was not taking any other medication concurrently. Dermatological examination revealed scattered erythematous lesions on the trunk. Many of lesions had peripheral scales (Figures 1 and 2). Patient did not identify herald patch lesion. Patient did not describe prodromal symptoms. General physical examination was unremarkable. Laboratory test results were within normal limits. The clinical appearance of the lesions was compatible with PR. Light microscopic examination revealed areas of orthokeratosis and focal parakeratotic mounds in the skin. The epidermis showed mild irregular acanthosis, a small number of apoptotic keratinocytes and lymphocyte exocytosis. Edema was observed in the superficial dermis as well as perivascular lymphoid cell infiltration accompanied by infrequent eosinophilic leukocytes (Figure 3). Isotretinoin therapy was discontinued. Discontinuation of isotretinoin treatment brought about complete remission of the cutaneous lesions within 10 days. No new lesions had developed on follow-ups. Based on the drug history, clinical presentation, histopathological examination and clinical course our case was diagnosed as PR-like eruption induced by isotretinoin.
Figure 3: (A & B) Photomicrographs of skin punch biopsy (hematoxylin & eosin stain, original magnification x100 and x200, respectively).
Isotretinoin, a synthetic analog of vitamin A, is usually used in the treatment of resistant, nodulocytic acne and various other skin diseases. Cheilitis, xerosis, photosensitivity, dryness, hair loss and fragility of the oral and nasal mucosa are the most common adverse effects of isotretinoin [4]. The mechanism of PR-like eruption induced by isotretinoin is unknown.
Drago et al. [5] studied 15 patients with PR-like eruptions. They found that in PR-like eruptions the lesions are more itchy, diffuse and confluent than in classic PR and mucous membranes can be involved. Our patient did not have any lesions on mucous membrane. Eosinophils in the dermis, epidermal necrotic keratinocytes and junctional vacuolar degeneration are seen at histopathology in PR-like eruptions [5,6]. There were also similar histopathological findings in our patient. Histopathological examination revealed signs of a drug hypersensitivity reaction, including increased numbers of dermal eosinophils. This phenomenon may be due to a drug hypersensitivity reaction. Drago et al. [6] studied 12 patients with PR-like eruptions and they reported that all the patients recovered 2 weeks after discontinuing the drug, which is less than it takes for classic PR. After the isotretinoin therapy was discontinued, the lesions were completely resolved within 10 days. No new lesions had developed on follow-ups.
In conclusion, we report the second clinical case of isotretinoin induced PRlike eruptions.
REFERENCES
- Gürel G, Sahin S, Çölgeçen E. Pityriasis rosea-like eruption induced by isotretinoin. Cutan Ocul Toxicol. 2017;19:1-3.
- Drago F, Ciccarese G, Rebora A, et al. Pityriasis rosea: A comprehensive classification. Dermatology. 2016;232:431-7.
- Helfman RJ, Brickman M, Fahey J. Isotretinoin dermatitis simulating acute pityriasis rosea. Cutis. 1984;33:297-300.
- Demirseren DD, Kilinc F, Emre S, et al. The weeks and the cumulative doses of the first adverse events related to oral isotretinoin in acne patients: analysis of 300 patients. J Dermatol Treat. 2016;15:1-5.
- Drago F, Ciccarese G, Rebora A, et al. Pityriasis rosea and pityriasis rosea-like eruption: can they be distinguished? J Dermatol. 2014;41:864-5.
- Drago F, Broccolo F, Agnoletti A, et al. Pityriasis rosea and pityriasis rosea-like eruptions. J Am Acad Dermatol. 2014;70(1):196.