Common eye problems in India
Received: 12-May-2021 Accepted Date: May 27, 2021; Published: 04-Jun-2021
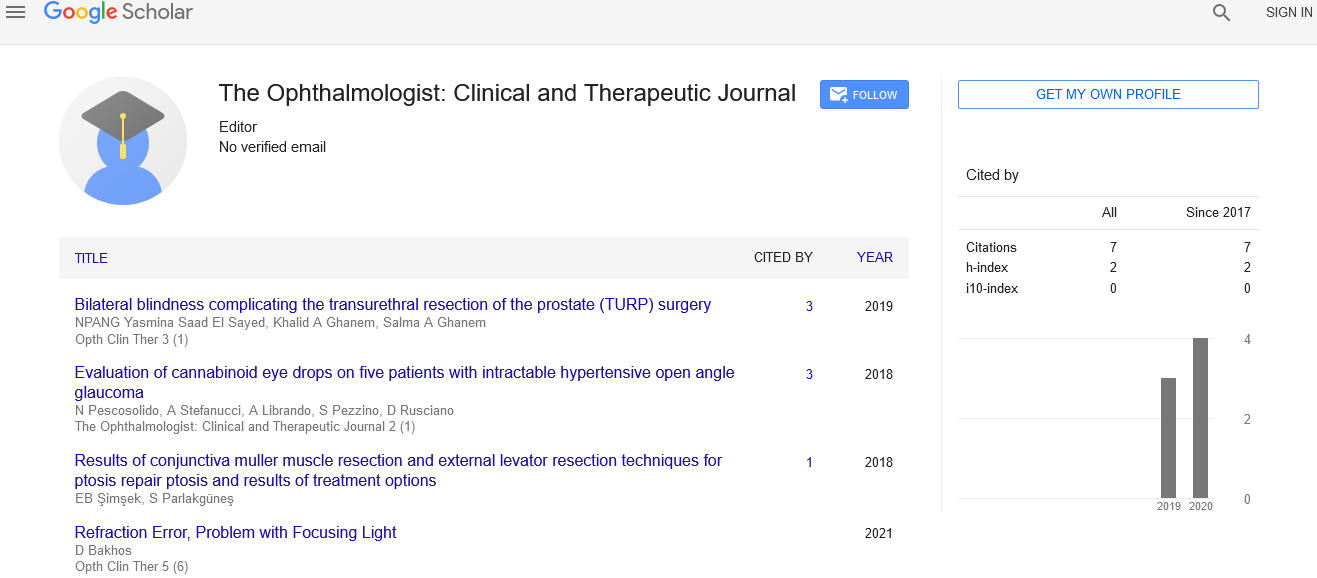
Citation: Mosavi S. Common eye problems in India. Opth Clin Ther. 2021;5(3):3.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
About the Study
Hundreds of new genes linked to blindness and other vision disorders have been identified in a screen of mouse strains, according to new research by the University of California, Davis. According to researchers, many of these genes are likely important in human vision and the results could help identify new causes of hereditary blindness in patients. No matter how much you take care of your eyes, there are times when you are most likely to suffer from at least one common eye problems. While some of these problems cause very little harm to the eyes, few of them may lead to the permanent blindness of the eyes.
Some of the most common eye diseases that a person may suffer with strain in the eyes, tears in the eyes, dry eye, eye floaters, eye cancer and tumors, tired eyes, red eyes, blurred vision, allergic conjunctivitis, night blindness, lazy eye, color blindness, yellow eyes, shingles in the eye, age is an important factor. Age, urban residence, occupation and socio-economic affluence were found to be high risk-factors for developing the disease.
Dry eye disease could occur due to inadequate tear production (aqueous deficient), tear film instability due to evaporation or mixed type. Over 20.5% had dry eye disease caused by inadequate tear production, 35.5% due to tear film instability (evaporative) and 40% being mixed.
It is essential to note that age plays a significant part in affecting the eyes. The infant eye problems are pretty different from that of growing teens, adults and senior citizens. At every point of life, a person is prone to get an eye disease which, if not treated at the right time, may prove to be very harmful to the vision.
For the first time, a large-scale, hospital-based study in India involving over 14.5 lakhs patients had found the incidence (number of new cases occurring each year) of dry eye disease to be 21,000 (1.46%). At over 12,500 cases, the incidence in urban areas was higher than in rural areas (over 8,700 cases). With a large ageing population, growing middle-class and chronic nature of the disease, India is on the verge of a dry eye disease epidemic, says the study. The prevalence of dry eye disease will be in about 40% of the urban population by 2030.
Since the disease tends to be progressive with age, once corneal damage becomes irreversible it can lead to visual impairment and even blindness. Early diagnosis and treatment is therefore important. The disease is hugely under diagnosed in India.
After uncomplicated cataract surgery, patients can generally be discharged from the recovery area once they are awake and alert with stable vital signs, demonstrate safe emergence from any anaesthetic or sedative agents given and report minimal or no pain. A plan for safe transport to the patient's home or other recovery location must be clear. Detailed written and verbal instructions must be given to the patient and any escort available with the patient. There should be a definite plan for a follow-up appointment and contact information to reach the operating physician and/or a designated medical partner who is qualified to care for the patient if that physician is unavailable.
Conclusion
Vogt-Koyanagi-Harada syndrome necessitates aggressive systemic therapy to shorten disease duration and to reduce the risk of extraocular complications or progression to a chronic stage. The first line of treatment is typically oral or intravenous corticosteroids. Oral corticosteroids are typically dosed at 1-2mg/kg/day and intravenous methylpresdnisone is dosed at 1mg/day for three days followed by a slow oral taper. According to Read et al, there is no statistically significant difference in final visual acuity or risk of cataract formation between VKH patients treated with oral corticosteroids versus IV and oral corticosteroids. Any concomitant anterior uveitis should also be treated with 1% prednisolone acetate, in addition to the systemic steroid therapy.