Comparison between the real corneal ablation excimer laser and the theoretical munnerlyns formula and the residual corneal thickness after lasik compared to safety limits
Received: 24-Aug-2020 Accepted Date: Sep 07, 2020; Published: 14-Sep-2020
Citation: Evangelos P, Evangelos K. Comparison between the real corneal ablation (excimer laser) and the theoretical (munnerlyn’s formula) and the residual corneal thickness after lasik compared to safety limits. Opth Clin Ther. 2020;4(3):1-4.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Aims: The purpose of this research is to compare the real corneal ablation (excimer Laser) with the theoretical (Munnerlyn’s Formula) and the residual corneal thickness after lasik compared to safety limits.
Sample and study design: The comparing data of 70 eyes, involved patients aged 19-59 years, undergone Lasik surgery for myopia. The data concerned the corneal flap measured by the excimer laser the real corneal ablation with the theoretical (Munnerlyn’s Formula) and the comparison of the residual corneal thickness after lasik to safety limits such as 300 μm.
Methodology, place and duration of study: University of west attica department of biomedical science course optics and optometry in collaboration with private ophthalmology clinic “Athens Opthalologiko” during the period between May 2018 until September 2018. All the refractive error surgeries were performed by the same experienced surgeon and the patients selected had healthy myopic eyes with no other ophthalmic pathology or systemic eye diseases. The myopia ranged from -1.00 to 9.25 Diopters. All participated voluntarily, maintaining their anonymity due to the protection of their personal data. Patients underwent refractive surgery with the excimer lasik method.
Results: The real flap thickness, recorded by the excimer laser was 119.74 μm ± SD 19.50. The actual ablation thickness ranged from 19.25 μm to 126.29 μm with an average value of 64.74 μm ± SD 28.39 μm and a median of 65.29 μm. The theoretical ablation thickness ranged from 12 μm to 118.52 μm, with a numerical average value of 57.79 μm ± SD 26.97 μm and a median of 53.69 μm, with correlation coefficient 0.9603 (P<0.0001). The calculated thickness of the residual stromal bed, (RSB) ranged from 308.14 μm to 490.28 μm with an average value of 374.84 μm ± SD 41.18 and median 374.10 μm. The difference of the residual stromal bed (RSB), from the safety limit of 250 μm for avoiding ektasia after Lasik, ranged from 58.14 μm to 240.28 μm, with an average value of 124.84 μm ± SD 41.18 μm and median 124.10 μm. The RSB was also compared with a safety thickness limit of 300 μm with a difference ranged from 8.14 μm to 190.28 μm, with an average value of 74.84 μm ± SD 41.18 μm and a median of 74.10 μm.
Conclusion: Our results of the ablation thickness with excimer laser lasik refractive surgery compared between the theoretical Munnerlyn’s formula and the one given by the excimer laser correlated strong with correlation coefficient 0.9603. The RSB difference with a safety thickness limit of 300 μm ranged from 8.14 μm to 190.28 μm, with an average value of 74.84 μm ± SD 41.18 μm and a median of 74.10 μm which is crucial for refractive surgery safety.
Keywords
Central corneal thickness; Refractive surgery; Lasik, Depth of ablation; Residual stromal bed; Corneal flap.
Introduction
The role of an excimer laser in a refractive surgery is very important [1,2]. The change in the curvature of the cornea determines the refractive power of the eye. An excimer laser is actually a system (medical equipment) that sculpts-sublimates the cornea (breaks down molecules and launches them into space, without any thermal damage to adjacent tissues), thus determining its shape and curvature, allowing so that the rays of light (visual stimuli) focus with great precision on the retina (change of refractive power) [3,4].
With each pulse of the laser, a small amount of corneal tissue is removed. Complex algorithms through an advanced technology software (excimer laser software) create the so-called refractive map of the cornea, programming the beam for what abnormalities will sublimate, saving corneal tissue [5,6].
The latest generation excimer laser systems support high precision flying spot technology with a minimum spot diameter per shot, which makes them corneal friendly. These offer excellent quality sculpting and unimaginable visual effects. In addition, the point beam achieves a significant reduction in the intensity of the radiation shock wave, resulting in limited corneal cell mobility, a slight increase in corneal tissue temperature, and limited transmission of the shock wave to the ocular tissues.
The radiation is released in successive steps and with a controlled repetition sequence. It used to be worth mentioning that excimer lasers used linear scanning technology. The latest generation excimer laser systems feature ocular tracker technology, also known as eye-tracker. In the eye-tracking system, the micro-movements of the eye are monitored with great accuracy (monitoring of the target through special video camera-guides the laser beam with incredible synchronization). Eye movements are in the range of 80- 100 Hz and therefore an effective eye-tracking system must necessarily have much faster tracking movements (at least 200 Hz). The movements that are perceived by the ophthalmic tracker are in X, Y axes, dynamic cyclotorsion, but also in Z-axis. Thus, even in anxious patients, the ultimate refractive correction is achieved. Today an ophthalmic tracker can operate at 1000 Hz [6-8].
Methodology
All participants volunteered, underwent refractive surgery with the excimer lasik method. According to gender the sample population consisted of 38.89% men and 61.11% women (Figure 1). An experienced surgeon operated all patients which were selected to be healthy with no other ophthalmic pathology or systemic eye diseases and moderate myopia. The myopia corrected ranged from -1.00 to 9.25 Diopters. The flap actual thickness was recorded from the Laser report post-operatively [9].
Femtosecond laser FS 200 (Wavelight, Alcon) was used in order to create the corneal flap. The ablation was performed with the excimer laser Allegretto Wave Concerto 500 Hz (Wavelight AG Erlangen Germany). With the development of femtosecond lasers, flap creation is more precise, and most surgeons use a flap thickness near 100 microns. From the data we calculated other parameters that served us in our statistical analysis. Specifically, we calculated the spherical equivalent from the relation:
Sph. Equiv.=D sph+½ D cyl
Where Sph.Equiv., the spherical equivalent in diopters, D sph. The amount of myopia in diopters and D cyl. The amount of astigmatism in diopters.
We then calculated the corneal thickness after ablation by subtracting the remaining thickness from the original thickness measured with Pentacam® AXL before refractive surgery [10-15]. We also calculated the residual thickness of the corneal layer (RSB residual stromal bed), subtracting from the initial thickness the thickness of the flap and the thickness of the ablation [16,17].
RSB=thickness before LASIK (T)-(flap thickness+ablation thickness)
In other studies, such as [18] the thickness of the flap is theoretically calculated and has a constant value of 160 m. In the present work the thickness of the flap is the real one and has been recorded as given by the laser reference. Therefore, the measurements for the remaining corneal layer are more accurate. We also compared the remaining thickness with the safety thicknesses mentioned in the literature, of 250 m or 300 m. We calculated for each patient the difference of the RSB, from the safety thickness and recorded it.
It is very important in refractive surgery to calculate the ablation thickness preoperatively in order to safely decide whether or not to operate. The remaining corneal layer, calculated from the thickness of the resection, is critical for the fear of the most dangerous LASIK complication of this area [18-20].
There are two ways to calculate thickness preoperatively. One is using the mathematical model of the Munnerlyn’s form [16,17], and the second is from the software of each excimer laser used for ablation.
Each laser unit uses a nomogram based on which it calculates how many small layers are removed for each diopter we want to correct. If we multiply the number of diopters to be corrected by the corresponding microns, we get the amount of the total ablation. An ablation zone is usually 6.5 mm. In some circumstances, the ablation zone may be 6.0 mm this is due to that a thin cornea with high correction needs a 6.0 mm treatment zone to conserve tissue. Additionally, if the patient has a small pupil size in scotopic light, a 6.0 mm ablation zone is preferred.
The mathematical formula is defined by the relation:
Ablation thickness depth (theoretical)=1/3 D*d2
Where D=spherical equivalent in diopters of the correction we want and d=diameter of the optical zone in millimeters
The ablation thickness depth is calculated in μm.
The ablation depth does not include the transition (blend) zone of the surgery which usually adds extra 8 microns [16,17].
This relationship is the approximate form of the Munnerlyn’s form [16,17] that is widely used to calculate ablation thickness preoperatively. It is simple and is based on two variables, the diopters we want to correct and the ablation zone that we will use. There is also the exact Munnerlyn’s form which uses three variables, and more complex mathematics.
There is a relationship between preoperative corneal thickness, ablation depth, and flap thickness that has occurred after a LASIK procedure.
Percentage of tissue altered=(flap thickness+ablation depth)/preoperative central corneal thickness.
If the percentage of corneal tissue altered is greater than 40% this is associated with the development of ectasia in eyes with normal preoperative topography.
Results and Discussion
The thickness preoperatively with the Pentacam® AXL topographic method ranges from 495 μm to 612 μm, with an average value of 556.26 μm ± SD 27.82 and median 563 μm. The thickness of the cornea postoperatively, including the thickness of the flap (thickness after Lasik), ranged from 435.25 μm to 588.14 μm, with an average value of 491.5 μm ± SD 36.79 and median 481.24 μm.
Regarding the flap thickness, we had the actual flap thickness, recorded by the excimer laser was 119.74 μm ± SD 19.50. The statistics of the flap thickness is shown in Table 1.
| Laser Output | |
|---|---|
| Sample size | 70 |
| Lowest value | 740,000 |
| Highest value | 1,870,000 |
| Arithmetic mean | 1,197,429 |
| 95% CI for the mean | 115,0938 to 124,3919 |
| Median | 1,185,000 |
| Variance | 3,801,648 |
| Standard Deviation | 194,978 |
| Standard error of the mean | 23,304 |
| Coefficient of Skewness | 0,5799 (P=0,0457) |
| Coefficient of Kurtosis | 1,2962 (P=0,0235) |
Table 1: Flap thickness derived from laser
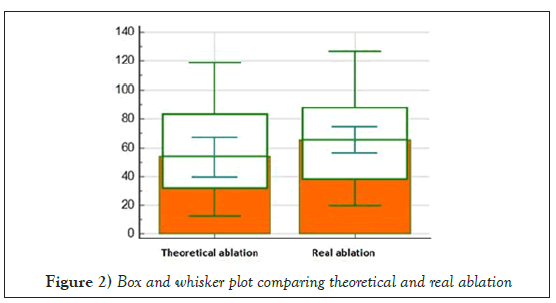
The actual ablation thickness ranged from 19.25 μm to 126.29 μm with an average value of 64.74 μm ± SD 28.39 μm and a median of 65.29 μm. The theoretical ablation thickness ranged from 12 μm to 118.52 μm, with a numerical average value of 57.79 μm ± SD 26.97 μm and a median of 53.69 μm, with correlation coefficient 0.9603 (P<0.0001) (Table 2) (Figure 2).
| Real measured | Theoretical | |
|---|---|---|
| Sample size | 70 | 70 |
| Arithmetic mean | 647,457 | 577,921 |
| 95% CI for the mean | 57,9760 to 71,5154 | 50,7160 to 64,8683 |
| Median | 65,29 | 53,69 |
| Variance | 8,060,666 | 8,806,936 |
| Standard Deviation | 283,913 | 296,765 |
| Standard error of the mean | 33,913 | 3,547 |
| Paired samples t-test | Real measured vs Theoretical | |
| Mean difference | 69,536 | |
| Standard deviation of mean difference | 82,785 | |
| Standard error of mean difference | 0,9895 | |
| 95% CI | 4,9796 to 8,9275 | |
| Test statistic t | 7,028 | |
| Degrees of Freedom (DF) | 69 | |
| Two-tailed probability | P<0,0001 | |
| Correlation | Pentacam and Ultrasound | |
| Correlation coefficient r | 0,9603 | |
| Significance level | P<0,0001 | |
| 95% Confidence interval for r | 0,9367 to 0,9752 | |
Table 2: Corneal thickness ablation
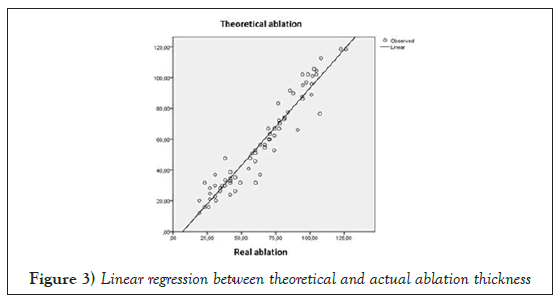
The regression for the above variables was performed and the relationship described by the linear correlation model is as follows:
At=-7.198+1.004 a (R2=0.921 R=0.960)
Where at=the theoretical ablation thickness
a=the actual ablation thickness
The following Figure 3 graphically illustrates the linear relationship that connects them.
Continuing, we calculated the thickness of the residual stromal bed (RSB), whose value ranged from 308.14 μm to 490.28 μm with an average value of 374.84 μm ± SD 41.18 and median 374.10 μm.
The difference of the residual stromal bed (RSB), from the safety limit of 250 μm for avoiding ectasia after Lasik, ranged from 58.14 μm to 240.28 μm, with an average value of 124.84 μm ± SD 41.18 μm and median 124.10 μm.
The difference of RSB was also calculated with a safety thickness limit of 300 μm. Here the difference ranged from 8.14 μm to 190.28 μm, with an average value of 74.84 μm ± SD 41.18 μm and a median of 74.10 μm.
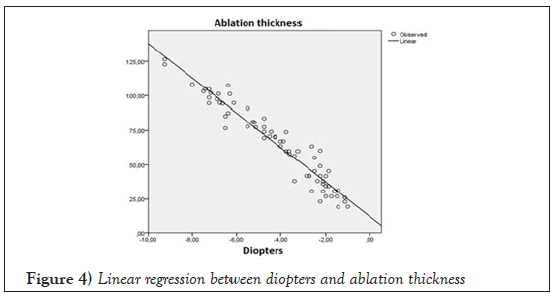
Regression was also performed for the amounts of diopters (spherical equivalent) corrected, with the thickness of the ablation (Figure 4), and the relationship described by the linear correlation model as follows:
a=12.312-12.558*D (R2=0.927, R=0.962)
Where a=actual ablation thickness in μm
D=diopters corrected (spherical equivalent)
Conclusion
Refractive surgery is very common in our time. But as their frequency increases, the need for safer results becomes more urgent. Advances in technology have helped a lot in this area, so that the forecast is very reliable and the results are safe.
Pachymetry in these operations is crucial for the decision and type of surgery as well as for the calculation of the corneal layer that remains intact after surgery to avoid ectasia. Ectasia is such a serious complication that it leads to severe vision loss that may require corneal transplantation to restore.
The most common and reliable method for performing pachymetry is ultrasound measurement. Of course, it has its drawbacks, as it is a contact method that requires anesthesia and there is always the risk of contamination from non-sterile materials used during the measurement. Pachymetry through topographic methods e.g. with the use of Pentacam® AXL, as in the present study, is gaining ground in recent years and is proving reliable.
The thickness of the flap ranged from 74 μm to 187 μm with an average value of 119.50 ± SD 19.50, which means that thinner flaps are preferred over older one’s techniques. For many years the flaps were 160 m thick, especially when made with a micro-keratome. Perhaps the use of femtosecond lasers has helped in this direction. Thinner flaps allow us to have more available layer thickness for ablation and are crucial, especially when large impeccability needs to be corrected.
Regarding the ablation thickness, there are ways to determine it computationally but also to measure it after the operation. We chose for its calculation the mathematical model of the Munnerlyn form. To calculate the thickness in this way we assume that a circular flap is made. We refer to myopic corrections only, because the small hyperopic corrections are made peripherally, where the cornea is thicker and is less prone to ectasia phenomena.
We compared the theoretical ablation thickness with the real one, and the correlation coefficient was 0.963, a value that shows a strong correlation, so our calculations give the ablation thickness quite accurately. It is clear that the Munnerlyn form underestimates the thickness as also reported in the 2003 study by Chang et al. The correlation of the two variables (theoretical ablation thickness with the real one) was strong.
As we have mentioned, one parameter to avoid area is the remaining corneal layer to be more than 250 m or 300 m. There are other factors that are responsible for ectasia phenomena that can be studied in other research. Regarding the calculation of the thickness that remains intact, after the corneal surgery, for all cases of our population, the safety limits were observed. In fact, in some cases, the prices allow re-intervention. Of course, the extent may appear several years after the operations, so that in borderline cases, the re-examination should be more frequent and thorough.
In summary, we can say with certainty that the reliability of thickness measurements using imaging through Pentacam® AXL topographic systems is scientifically proven and allows us to use in our daily practice a method of calculating thickness, intact fast and painless for the patient. Preoperative examination is the first and most important step towards safer operations and our research has added another element to the relationship between theoretical and actual resection thickness, in the field of initial data investigation. The limit of 250 m and 300 m for the remaining thickness (RSB) has been consolidated in the consciousness of surgeons and in their daily practice and as shown in our research is observed in all individuals of our population. Finally, the smallest possible thickness of the flap allows us to have larger ablations and to maintain a higher percentage of intact corneal layers.
REFERENCES
- Pallikaris IG, Siganos DS. Excimer laser in situ keratomileusis and photorefractive keratectomy for correction of high myopia. J Refract Corneal Surg. 1994; 10: 498-510.
- Kim T, Barrio JL, Wilkins M, et al. Refractive surgery. The Lancet. 2019; 393: 2085-2098.
- Fiander DC, Tayfour F. Excimer laser in situ keratomileusis in 124 myopic eyes. J Refract Surg. 1995; 11: S234–S238.
- Liang H, Yiqing H, Meng L. Excimer laser and femtosecond laser in ophthalmology. Richard Viskup. Intech Open 2016.
- Pidro A. Excimer lasers in refractive surgery. Acta Inform Med. 2019; 27: 278-283.
- Pajic B. Laser vision correction for regular myopia and supracor presbyopia: a comparison study. Appl Sci. 2020; 10: 873.
- Stonecipher K, Ignacio TS, Stonecipher M. Advances in refractive surgery: microkeratome and femtosecond laser flap creation in relation to safety, efficacy, predictability, and biomechanical stability. Curr Opin Ophthalmol. 2006; 17: 368-372.
- Pallikaris IG, Papatzanaki ME, Siganos DS, et al. A corneal flap technique for laser in situ keratomileusis. Human studies. Arch Ophthalmol. 1991; 109: 1699-1702.
- Sarhan AE, Abd Elaziz MS, Zaki MA, et al. Evaluation of corneal flap symmetry in the optical center by anterior segment optical coherence tomography: mechanical versus femtolaser flaps. Delta J Ophthalmol. 2019; 20: 100-106.
- Febbraro, Jean-Luc. Comparison of laser platform estimation and objective measurement of maximum ablation depth using scheimpflug pachymetry in myopic femtosecond laser in situ keratomileusis. Cornea. 2020; 39: 316-320.
- Huang J, Lu W, Savini G, et al. Evaluation of corneal thickness using a scheimpflug-placido disc corneal analyzer and comparison with ultra sound pachymetry in eyes after laser in situ keratomileusis. J Cataract and Refract Surg. 2013; 39: 1074-1080.
- Crispim J, Allemann N, Hallak J, et al. Direct and indirect flap measurements in femtosecond laser-assisted in situ keratomileusis. Cornea 2019; 38: 297-303.
- Parafita-Fernández A, García-Gonzalez M, Katsanos A, et al. Two femtosecond laser lasik platforms: comparison of evolution of visual acuity, flap thickness, and stromal optical density. Cornea 2019; 38: 98-104.
- Zhang XX, Zhong XW, Wu JS, et al. Corneal flap morphological analysis using anterior segment optical coherence tomography in laser in situ keratomileusis with femtosecond lasers versus mechanical microkeratome. Int J Ophthalmol. 2012; 5: 69-73.
- Mifflin MD, Mortensen XM. Intraoperative optical pachymetry in photorefractive keratectomy. J Cataract and Refract Surg. 2019; 45: 495-500.
- Munnerlyn CR, Koons SJ, Marshall J. Photorefractive keratecomy: a technique for laser refractive surgery. J Refratc Surg. 1988; 14: 46-52.
- Wa C, Tsang CA, Contreras EJ, et al. Corneal tissue ablation depth and the Munnerlyn formula. Journal Cataract and Refract Surg. 2003; 29: 1204-1210.
- Ou JR, Shew LE, Glasgon JB. Keratectasia after LASER in situ keratomileusis (LASIK): Evaluation of the calculated residual stromal bed. AMJ Ophthalmology. 2002; 134: 771-773.
- Santhiago M, Smadja D, Gomes B, et al. Association between the percent tissue altered and post-laser in situ keratomileusis ectasia in eyes with normal preoperative topography. Americ J Ophthalmology. 2014; 158: 87-95.
- Randleman JB, Woodward M, Lynn MJ, et al. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008; 115:37-50.