Computed tomography angiography findings of acute thrombotic occlusion of abdominal aorta: a case report
Hadi Sasani1*, Begum Ozuekren Kasapoglu2 and Mehdi Sasani3
1Department of Radiology, Near East University Faculty of Medicine, Nicosia, TRNC, Turkey
2Department of Cardiovascular Surgery, Istanbul Bilim University, Florence Nightingale Hospital, Istanbul, Turkey
3Trakya University, Medical Faculty, Department of Anatomy, Edirne, Turkey
- *Corresponding Author:
- Hadi Sasani, MD
Specialist, Department of Radiology, NEU Faculty of Medicine, Near East Boulevard, 99138, Nicosia, TRNC
Tel: +90(392) 675 10 00 /1132
E-mail: hadi.sasani@neu.edu.tr
Date of Received: November 7th, 2014
Date of Accepted: December 30th, 2016
Published Online: January 19th, 2017
© Int J Anat Var (IJAV). 2016; 9: 57–59.
[ft_below_content] =>Keywords
acute thrombotic occlusion, abdominal aorta, auricular thrombosis, computed tomography
Introduction
Acute aortic thrombotic occlusion (AATO) is a rare vascular condition which requires emergency surgery. Despite its proper management, the mortality and the morbidity rates are 35-52% and more than 75% respectively [1]. Occlusion may occur in any segment of the aorta, however, infrarenal abdominal aortic segment, particularly the iliac bifurcation is the most common site of the occlusion. Most large embolies which occlude the terminal aortic segments, arises from the heart, particularly from the left atrium, in the setting of atrial fibrillation. Other etiologic factors including atrial myxoma, vegetations in bacterial or fungal endocarditis, prosthetic valve thrombus may be infrequently seen [2-5] Its diagnosis depends on the clinical presentation including acute hypertension, abdominal symptoms, ischemic and neurologic symptoms of the lower extremities [5].
In this article, we present computed tomography angiography findings of a 87-old-years female patient with acute thrombotic occlusion of abdominal aorta.
Case Report
An 87-year-old female patient admitted to the hospital with complaints of pain and weakness in her lower extremities. 10 days ago, there was facial paralysis present in her history. On physical examination blood pressure was 130/80 mmHg, the heart rate was 140 bpm, it was evaluated as atrial fibrillation with rapid ventricular response, after application of 1 ampoule diltiazem, the heart rate was reduced to 82 bpm.
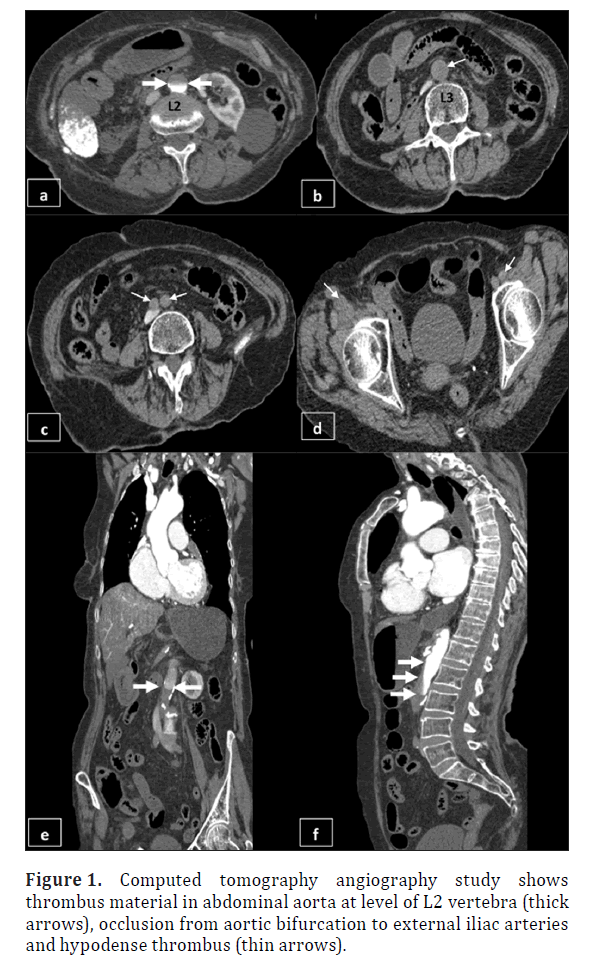
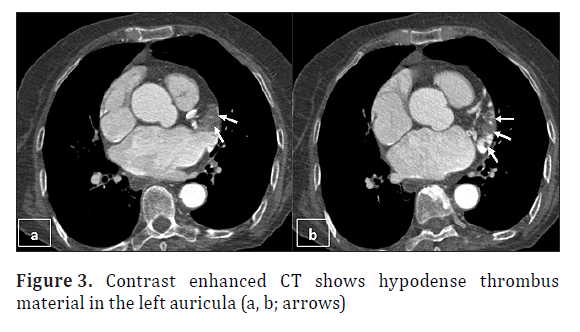
Beside this, coldness, paleness, bilateral femoral artery pulseless were present in her lower extremities. Sensory test was normal, muscle strength was evaluated as one positive. Due to the present findings, weak arterial flow and pulsus tardus pattern of both lower extremity from iliac artery to distal leg was detected in Doppler ultrasonography. Following, computed tomography angiography (CTA) showed abdominal aortic occlusion from L2 vertebral level to common femoral artery level (Figure 1). Left portal vein was partially thrombosed, main portal vein, splenic vein, celiac trunk and superior mesenteric artery were totally occluded. The liver parenchymal perfusion defect and due to right renal lower segmental artery occlusion, hypodense infarct region of right kidney was observed (Figure 2). Also, hypodense thrombus material was detected at cardiac apex and the left auricula (Figure 3). Imaging findings suggested the left heart originated thrombotic condition and secondarily developed acute thrombotic occlusion of abdominal aorta. During observation of the patient in emergency service, within a short time she had cardiac arrest, CPR was unresponsive and the patient passed away.
Figure 2. Contrast Enhanced CT shows partially thrombosed left portal vein and totally thrombosed main portal vein (a)(black thick arrows), totally occluded splenic vein, parenchymal perfusion defect in the liver (b)(thin black arrows); total occlusion in common hepatic artery (a)(White arrowheads), superior mesenteric artery (b, c) (black arrowheads). Hypodense infarction area due to occlusion of right inferior segmental renal artery (white arrows). Wide mural calcification of abdominal aorta is seen (d).
Discussion
AATO has high mortality and morbidity rates, may result from thrombus formation, saddle embolism, aortic aneurysm, aortic dissection, aortic trauma, arteriosclerosis, low flow states, hypercoagulability [5,6]. Major organ ischemia such as stroke, myocardial infarction, hepatic infarction, mesenteric ischemia, respiratory failure, fatal arrhythmia, renal failure secondary to myonecrosis may result in mortality [5]. Typically, patients with AATO have findings of acute limb ischemia, known as the “6 Ps” including pain, pallor, paresthesia, paralysis, poikilothermia, and pulselessness.
Radiological imaging is crucial in confirming the diagnosis. Magnetic resonance angiography (MRA), CTA and conventional angiography are the primary alternatives for diagnosis. Although conventional aortography is the gold standard test, however, it is invasive modality. Doppler ultrasonography, CTA and MRA are non-invasive imaging modalities. CTA is the most commonly preferred option for rapid imaging and confirming the diagnosis of AATO and detecting the concomitant intra-abdominal pathologies [8,9].
Conclusion
Due to high mortality and morbidity rates of AATO, its urgent diagnosis and treatments are most of value. Non-invasive and rapid imaging modalities such as Doppler ultrasonography, MRA and most commonly preferred CTA, provide saving time and additional information of the present condition.
References
- Kocabay G, Boztosun B, Karakaya S,Ergün S. Acute thrombotic occlusion of abdominal aorta: a case report. Turk Gogus Kalp Damar Cerrahisi Dergisi. 2013;21(1):183-186.
- Light JT Jr, Hendrickson M, Sholes WM, Portnoy DA, Bell WH 3rd, Kerstein MD. Acute aortic occlusion secondary to Aspergillus endocarditis in an intravenous drug abuser. Ann Vasc Surg. 1991;5:271-5.
- Lee WA. Acute aortic occlusion from a cardiac embolus. J Vasc Surg. 2003;38:197.
- Zhang J, Duan ZQ, Wang CJ, Song QB, Luo YW, Xin SJ. Acute aortic occlusion as an unusual embolic complication of cardiac myxoma. Chin Med J (Engl). 2006;119:342-4.
- Yamamoto H, Yamamoto F, Tanaka F, Motokawa M, Shiroto K, Yamaura G, Ishibashi K. Acute occlusion of the abdominal aorta with concomitant internal iliac artery occlusion. Ann Thorac Cardiovasc Surg. 2011; 17: 422-7.
- Dossa CD, Shepard AD, Reddy DJ, Jones CM, Elliott JP, Smith RF, Ernst CB. Acute aortic occlusion: a 40-year experience. Arch Surg. 1994;129:603-608.
- Babu SC, Shah PM, Nitahara J. Acute aortic occlusion—factors that influence outcome. J Vasc Surg. 1995;21:567-575.
- Bhalla S, Menias CO, Heiken JP. CT of acute abdominal disorders. Radiol Clin North Am. 2003;41:1153-1169.
- Bertucci B, Rotundo A, Perri G, Sessa E, Tamburrini O. Acute thrombotic occlusion of the infrarenal abdominal aorta. Its diagnosis with spiral computed tomography in a case. Radiol Med 1997;94:541-3.
Hadi Sasani1*, Begum Ozuekren Kasapoglu2 and Mehdi Sasani3
1Department of Radiology, Near East University Faculty of Medicine, Nicosia, TRNC, Turkey
2Department of Cardiovascular Surgery, Istanbul Bilim University, Florence Nightingale Hospital, Istanbul, Turkey
3Trakya University, Medical Faculty, Department of Anatomy, Edirne, Turkey
- *Corresponding Author:
- Hadi Sasani, MD
Specialist, Department of Radiology, NEU Faculty of Medicine, Near East Boulevard, 99138, Nicosia, TRNC
Tel: +90(392) 675 10 00 /1132
E-mail: hadi.sasani@neu.edu.tr
Date of Received: November 7th, 2014
Date of Accepted: December 30th, 2016
Published Online: January 19th, 2017
© Int J Anat Var (IJAV). 2016; 9: 57–59.
Abstract
Acute aortic thrombotic occlusion (AATO) is a rare vascular surgical condition which requires urgent interventional process. It has high mortality and morbidity rates. The diagnosis of AATO depends on clinical presentation including acute hypertension, abdominal symptoms, ischemic and neurologic symptoms of the lower extremities. Radiologic imaging is crucial in confirming the diagnosis.
In this article, we present computed tomography angiography findings of the patient with AATO.
-Keywords
acute thrombotic occlusion, abdominal aorta, auricular thrombosis, computed tomography
Introduction
Acute aortic thrombotic occlusion (AATO) is a rare vascular condition which requires emergency surgery. Despite its proper management, the mortality and the morbidity rates are 35-52% and more than 75% respectively [1]. Occlusion may occur in any segment of the aorta, however, infrarenal abdominal aortic segment, particularly the iliac bifurcation is the most common site of the occlusion. Most large embolies which occlude the terminal aortic segments, arises from the heart, particularly from the left atrium, in the setting of atrial fibrillation. Other etiologic factors including atrial myxoma, vegetations in bacterial or fungal endocarditis, prosthetic valve thrombus may be infrequently seen [2-5] Its diagnosis depends on the clinical presentation including acute hypertension, abdominal symptoms, ischemic and neurologic symptoms of the lower extremities [5].
In this article, we present computed tomography angiography findings of a 87-old-years female patient with acute thrombotic occlusion of abdominal aorta.
Case Report
An 87-year-old female patient admitted to the hospital with complaints of pain and weakness in her lower extremities. 10 days ago, there was facial paralysis present in her history. On physical examination blood pressure was 130/80 mmHg, the heart rate was 140 bpm, it was evaluated as atrial fibrillation with rapid ventricular response, after application of 1 ampoule diltiazem, the heart rate was reduced to 82 bpm.
Beside this, coldness, paleness, bilateral femoral artery pulseless were present in her lower extremities. Sensory test was normal, muscle strength was evaluated as one positive. Due to the present findings, weak arterial flow and pulsus tardus pattern of both lower extremity from iliac artery to distal leg was detected in Doppler ultrasonography. Following, computed tomography angiography (CTA) showed abdominal aortic occlusion from L2 vertebral level to common femoral artery level (Figure 1). Left portal vein was partially thrombosed, main portal vein, splenic vein, celiac trunk and superior mesenteric artery were totally occluded. The liver parenchymal perfusion defect and due to right renal lower segmental artery occlusion, hypodense infarct region of right kidney was observed (Figure 2). Also, hypodense thrombus material was detected at cardiac apex and the left auricula (Figure 3). Imaging findings suggested the left heart originated thrombotic condition and secondarily developed acute thrombotic occlusion of abdominal aorta. During observation of the patient in emergency service, within a short time she had cardiac arrest, CPR was unresponsive and the patient passed away.
Figure 1. Computed tomography angiography study shows thrombus material in abdominal aorta at level of L2 vertebra (thick arrows), occlusion from aortic bifurcation to external iliac arteries and hypodense thrombus (thin arrows).
Figure 2. Contrast Enhanced CT shows partially thrombosed left portal vein and totally thrombosed main portal vein (a)(black thick arrows), totally occluded splenic vein, parenchymal perfusion defect in the liver (b)(thin black arrows); total occlusion in common hepatic artery (a)(White arrowheads), superior mesenteric artery (b, c) (black arrowheads). Hypodense infarction area due to occlusion of right inferior segmental renal artery (white arrows). Wide mural calcification of abdominal aorta is seen (d).
Discussion
AATO has high mortality and morbidity rates, may result from thrombus formation, saddle embolism, aortic aneurysm, aortic dissection, aortic trauma, arteriosclerosis, low flow states, hypercoagulability [5,6]. Major organ ischemia such as stroke, myocardial infarction, hepatic infarction, mesenteric ischemia, respiratory failure, fatal arrhythmia, renal failure secondary to myonecrosis may result in mortality [5]. Typically, patients with AATO have findings of acute limb ischemia, known as the “6 Ps” including pain, pallor, paresthesia, paralysis, poikilothermia, and pulselessness.
Radiological imaging is crucial in confirming the diagnosis. Magnetic resonance angiography (MRA), CTA and conventional angiography are the primary alternatives for diagnosis. Although conventional aortography is the gold standard test, however, it is invasive modality. Doppler ultrasonography, CTA and MRA are non-invasive imaging modalities. CTA is the most commonly preferred option for rapid imaging and confirming the diagnosis of AATO and detecting the concomitant intra-abdominal pathologies [8,9].
Conclusion
Due to high mortality and morbidity rates of AATO, its urgent diagnosis and treatments are most of value. Non-invasive and rapid imaging modalities such as Doppler ultrasonography, MRA and most commonly preferred CTA, provide saving time and additional information of the present condition.
References
- Kocabay G, Boztosun B, Karakaya S,Ergün S. Acute thrombotic occlusion of abdominal aorta: a case report. Turk Gogus Kalp Damar Cerrahisi Dergisi. 2013;21(1):183-186.
- Light JT Jr, Hendrickson M, Sholes WM, Portnoy DA, Bell WH 3rd, Kerstein MD. Acute aortic occlusion secondary to Aspergillus endocarditis in an intravenous drug abuser. Ann Vasc Surg. 1991;5:271-5.
- Lee WA. Acute aortic occlusion from a cardiac embolus. J Vasc Surg. 2003;38:197.
- Zhang J, Duan ZQ, Wang CJ, Song QB, Luo YW, Xin SJ. Acute aortic occlusion as an unusual embolic complication of cardiac myxoma. Chin Med J (Engl). 2006;119:342-4.
- Yamamoto H, Yamamoto F, Tanaka F, Motokawa M, Shiroto K, Yamaura G, Ishibashi K. Acute occlusion of the abdominal aorta with concomitant internal iliac artery occlusion. Ann Thorac Cardiovasc Surg. 2011; 17: 422-7.
- Dossa CD, Shepard AD, Reddy DJ, Jones CM, Elliott JP, Smith RF, Ernst CB. Acute aortic occlusion: a 40-year experience. Arch Surg. 1994;129:603-608.
- Babu SC, Shah PM, Nitahara J. Acute aortic occlusion—factors that influence outcome. J Vasc Surg. 1995;21:567-575.
- Bhalla S, Menias CO, Heiken JP. CT of acute abdominal disorders. Radiol Clin North Am. 2003;41:1153-1169.
- Bertucci B, Rotundo A, Perri G, Sessa E, Tamburrini O. Acute thrombotic occlusion of the infrarenal abdominal aorta. Its diagnosis with spiral computed tomography in a case. Radiol Med 1997;94:541-3.