Conduct Disorder in Children
Received: 01-Jul-2021 Accepted Date: Jul 20, 2021; Published: 28-Jul-2021
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Prime Focus
Conduct disorder (CD) is a childhood persistent psychiatric disorder. It is characterized by aggression, antisocial activities and animal cruelty.
It is comorbid with attention-deficit/hyperactivity disorder (ADHD) and depression.
Children with CD remain socially isolated. Face difficulty in interacting with other children and due to low integration with society tend to increased involvement in criminal acts and substance misuse.
The low levels of 5-Hydroxy Indole acetic acid in Cerebrospinal Fluid affect the neurological functions. High testosterone levels and low levels of plasma dopamine beta-hydroxylas are the reason for increased aggressive behavior. Heritability is also sometimes the biological factor for CD.
The risk factors include harsh parenting, poor infant nutrition, developmental delays, brain injury, seizures, exposure to violence in the community.
The family members or the caretakers are the first persons to identify about the disorder in the child based on his behavior.
Diagnosis of CD in children is conducted based on high degree of aggressive behavior compared to the age, damage to property, school truancy. The psychiatric condition, academics and family history of the child is accessed.
Compared to the risk factors involved, multi-modal treatment is most effective in treating CD. The multi-modal treatment involves a family based approach addressing the current social activity of the family and the residential area. The physician explains about the disease condition of CD and its effects in the long run in the family. Based on the severity of the condition the physician may opt for non-pharmacological treatment or in combination with interventional treatment.
Non pharmacological treatment involves the physician attending to the psychosocial causes of CD such as parent management training, anger management and community based treatment. In the parent management training, the parents or caretakers are made aware of the ongoing situation in the family that are affection the psychological condition of the child. The parents or caretakers are asked to avoid fighting in front of child, provide sufficient nutrition to the child. In the anger management training the child is exposed to peaceful areas, colourful play things and funny tours. During the community based treatment, the child is educated on how to co-live with the society, with other children and pets. The parent management training, anger management training and community based treatment should occur simultaneously.
Pharmacological or interventional treatment is preferred when CD exists with comorbidities such as aggression, depression, ADHD, bipolar disorder, seizers and any other neurodevelopmental disorders. Interventional therapy is suggested for children with psychiatric comorbidities such as ADHD, stimulant and non-stimulants are prescribed. Antidepressants are prescribed for treating depression. Mood stabilizers such as antiepileptic drugs and antipsychotic drugs are prescribed for reducing aggression and bipolar disorder.
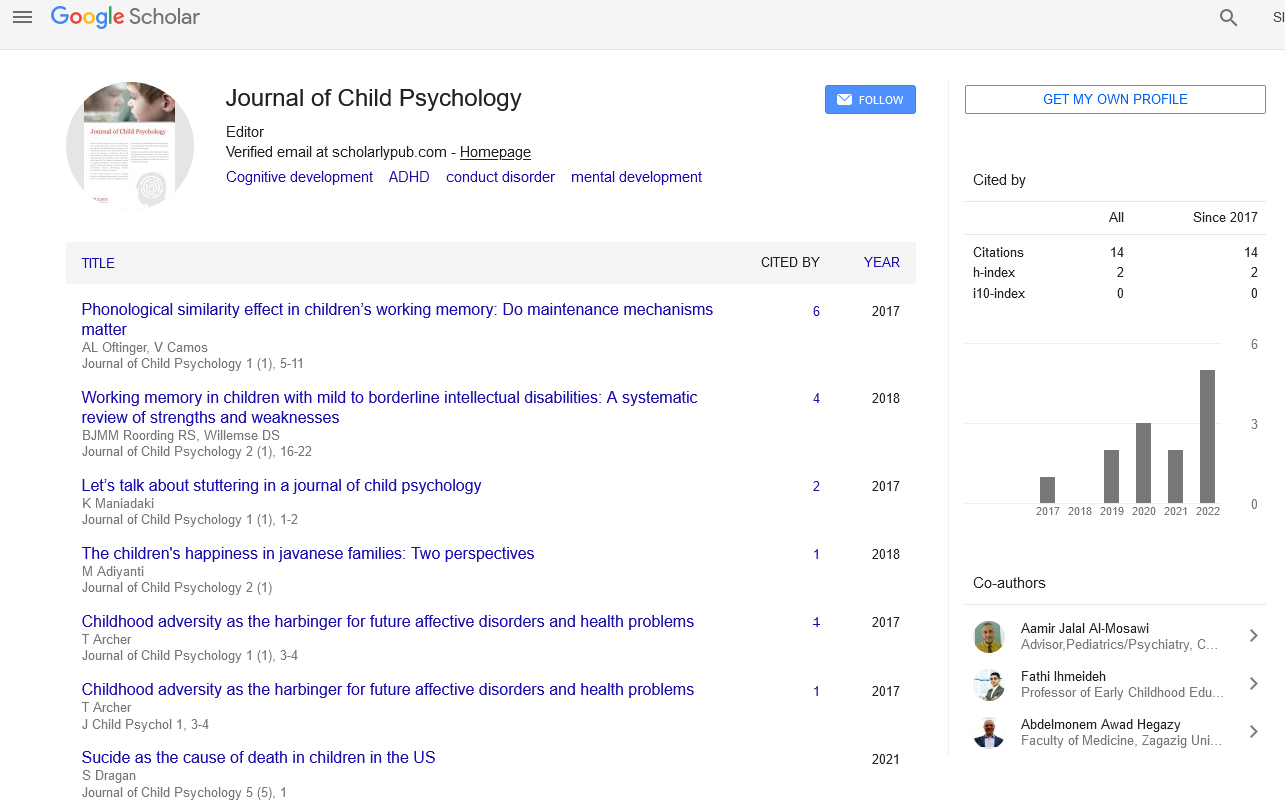
Journal of Child Psychology is a peer reviewed open access journal that aims to provide the most complete and reliable source of information on the cognitive and behavioural development of the infants at the formative years as they progress to adolescents. The journal thus publishes the cutting edge research outcome on topics including but not limited to Child Psychology, Infant Behaviour, IQ, Cognitive Development, ADHD, CD, depression, Speech & Language Development.