Conversion surgery for gastric cancer
Received: 04-Aug-2022, Manuscript No. pulcmr-22-5359; Editor assigned: 09-Aug-2022, Pre QC No. pulcmr-22-5359(PQ); Accepted Date: Aug 27, 2022; Reviewed: 20-Aug-2022 QC No. pulcmr-22-5359(Q); Revised: 24-Aug-2022, Manuscript No. pulcmr-22-5359(R); Published: 28-Aug-2022, DOI: 10.37532/ pulcmr-2022.4(4).59-61
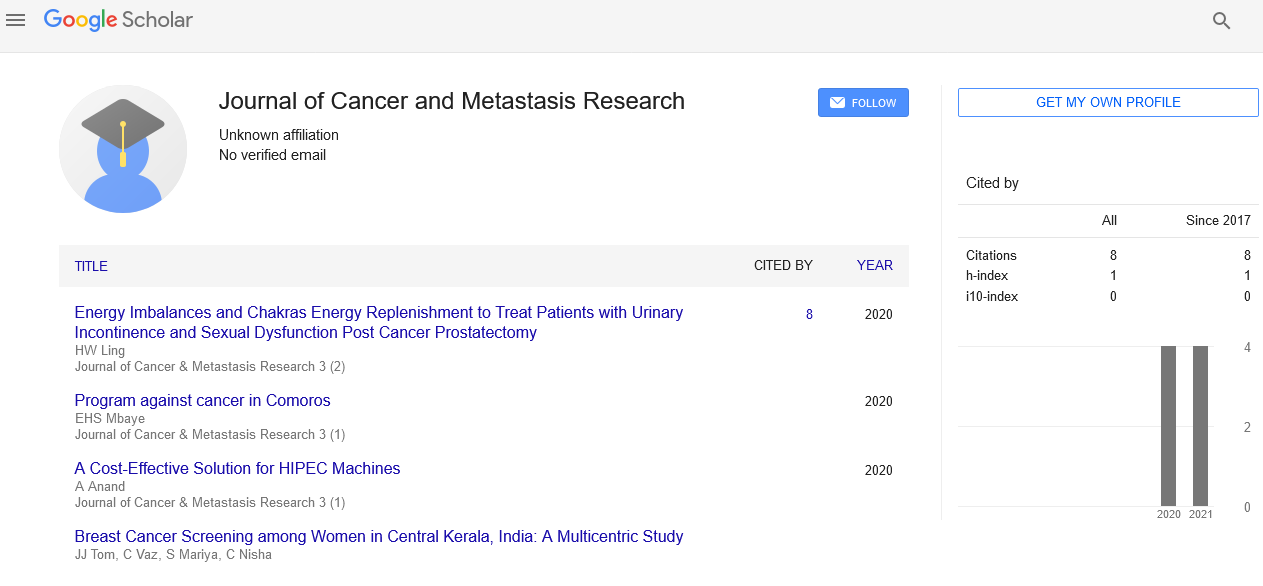
Citation: Dio M. Conversion surgery for gastric cancer. J Cancer Metastasis Res. 2022; 4(4):59-61
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Poor prognosis has been documented among patients with peritoneal spread of gastric cancer, despite chemotherapy being clinically advised as the initial treatment. The prognostic importance of conversion surgery following chemotherapy is still unknown, though. Therefore, the purpose of the current study was to evaluate the clinical effects of conversion surgery in patients with peritoneal spread of gastric cancer. Based on the tumour response to treatment, 93 patients with peritoneal spread of gastric cancer who had chemotherapy between February 2002 and October 2019 were retrospectively enrolled and split into progressing disease (PD) and non-PD groups.
Key Words
Prognosis; Gastrointestinal; Chemotherapy; Cancer; Tumors
Introduction
One of the most prevalent gastrointestinal malignancies in Asia and the third largest cause of cancer death globally is gastric cancer [1]. Studies have shown that patients with stage IV disease had a 5-year survival rate of 8.8%-14.9%, although recent advances in chemotherapy have significantly improved the prognosis for patients with unresectable advanced or recurrent gastric cancer [2, 3]. One prominent metastatic pattern among patients with advanced gastric cancer has been peritoneal dissemination, with big type-3 and type-4 tumors usually causing P1 (Peritoneal Dissemination) or CY1 (Positive Peritoneal Cytology). 53.4% of patients with big type-3 and type-4 gastric cancer develop P1 or CY1, according to retrospective research using staging laparoscopy [4]. According to reports, people with CY1 and P1 and the 5-year Overall Survival (OS) rates for patients with CY1 and P1 are 12.3% and 8.3%, respectively, according to reports [5]. Currently, CY1 and P1 are classified as distant Metastasis (M1) in both the Japanese classification of gastric cancer and the Tumor-Node-Metastasis (TNM) classification for gastric carcinoma developed by the International Union Against Cancer. As a result, stage IV is assigned to gastric cancer with CY1 or P1 [6, 7]. According to the aforementioned research, peritoneal dissemination is among the most crucial prognostic variables for people with gastric cancer.
Systemic chemotherapy is advised as the conventional first-line treatment for patients with M1 gastric cancer, including peritoneal dissemination, according to the Japanese Gastric Cancer Treatment Guidelines 2018 [8]. A new biological classification for the therapeutic direction of patients with stage IV gastric cancer. According to this new classification, stage IV gastric cancer patients are divided into four groups (categories 1-4), with those who have P1 falling into categories 3 or 4. Additionally, conversion therapy is a key component of the treatment plans for patients with a variety of malignancies, including gastric cancer [ 8]. This approach is founded on the idea that patients with category 3 and category 4 cancers can have curative resection (R0) after surgery. Several researchers have so far documented the therapeutic benefit of conversion surgery following chemotherapy in individual patients with colorectal, pancreatic, esophageal, and gastric cancer, conversion surgery following chemotherapy is clinically useful to several investigators. Conversion surgery among responders with P1 gastric cancer following chemotherapy has unfortunately only been the subject of a small number of research. Therefore, the clinical effects of conversion surgery in patients with peritoneal spread of gastric cancer are still unknown.
Surprisingly, the current investigation discovered that 94.7% of P1 patients had tumors of types 3 or 4. Additionally, all patients with type 3 and type 4 malignancies as well Surprisingly, the current investigation discovered that 94.7% of P1 patients had tumors of type 3 or type 4. Additionally, staging laparoscopy was performed on all patients who had type 3 and type 4 tumors but no clinical P1 was identified by imaging tests. Furthermore, staging laparoscopy or laparotomy was used to confirm P0 and CY0 in all patients undergoing conversion surgery. These findings suggested that in individuals with big type 3 and type 4 tumors, staging laparoscopy was clinically effective for detecting occult peritoneal spread. In the nottoo-distant future, staging laparoscopy might be a crucial tool for selecting treatment plans for individuals with P1 gastric cancer. Patients with P1 gastric cancer who participated in a randomized phase III trial comparing intraperitoneal and intravenous paclitaxel plus S-1 (IP) and S-1Pplus cisplatin (SP) demonstrated median survival durations of 17.7 months and 15.2 months and 3-year OS rates of 21.9% and 6.0%, respectively. These results suggested that intraperitoneal paclitaxel therapy was superior to S-1 plus cisplatin in controlling peritoneal spread in patients with advanced gastric cancer. As a result, intraperitoneal chemotherapy may be a useful treatment option for those with P1 stomach cancer.
The histological response of initial tumors is divided into four stages in the Japanese classification of gastric cancer, with grade 3 designating the lack of viable tumor cells [6]. According to Nakamura et al., 5.9% of patients with P1 or CY1 and 5.9% of patients with P1 or CY1 gastric cancer who had conversion surgery after chemotherapy showed a grade 3 response. Similar to this, according to Kinoshita et al., only 2 (5.9%) of 34 patients with stage IV gastric cancer who had conversion surgery after receiving docetaxel, cisplatin, and S-1 therapy showed a grade 3 histological response. But in the current investigation, no patient showed a grade 3 histological response. the findings mentioned chemotherapy. The clinical benefit of conversion surgery may be in its capacity to eradicate chemoresistant tumor cells given that it permits the removal of live tumor cells from primary sites and lymph nodes after treatment. chemotherapy. Considering that conversion surgery allows for the removal of live tumor cells in primary sites following chemotherapy. The clinical benefit of conversion surgery may be in its capacity to eradicate chemo-resistant tumor cells given that it permits the removal of live tumor cells from primary sites and lymph nodes after treatment implying that it is challenging to eradicate basic gastric tumor cells using Clinical justifications for conversion surgery following chemotherapy in P1 gastric cancer patients are still unknown. Recent research, however, has shown the therapeutic significance of R0 resection in conversion surgery. Patients with unresectable gastric cancer who underwent R0 and R1/R2 resections had 5-year OS rates of 49% and 15%. In addition, the same study's multivariate analysis revealed R0 resection to be an independent predictor of a good OS. Following multivariate analysis, an Italian retrospective cohort research similarly discovered residual tumor status (R0 vs. R1) following conversion surgery as an independent predictive factor for progression-free survival among patients with stage IV unresectable gastric cancer. The R0 resection rate in the current study was 94.7% (18/19). Hence, Therefore, those who responded to chemotherapy and were found to have P0 and CY0 after staging laparoscopy may at least be clinically suggested for conversion surgery. A close correlation between survival and lymph node status, the number of distant metastatic locations, or histological type was also revealed by univariate analysis among respondents.The aforementioned clinicopathological variables may serve as significant predictors for determining whether conversion surgery is necessary. Conversion surgery was also recognized by multivariate analysis as an independent prognostic factor among respondents. According to several studies conducted on patients with P0 and CY1 gastric cancer, those who underwent conversion surgery had a much better prognosis than those who did not. As a result, conversion surgery may be able to help patients with P1 gastric cancer who have had chemotherapy.
We looked back on 93 patients who received chemotherapy at Kagoshima University Hospital (Kagoshima, Japan) between February 2002 and October 2019 and had peritoneal spread of gastric cancer. These patients were 55 men and 38 women, ages 30-86, with a mean age of 64.2 years. Patients with disease recurrence and synchronous or metachronous malignancy in other organs were not included in this study. Before beginning chemotherapy, all patients had blood tests, esophagogastroduodenoscopies, endoscopic ultrasonography, fluoroscopy, and computed tomography. Based on the TNM classification for stomach cancer, patients were grouped and staged [7]. The clinic's pathological characteristics of the participants. Among the 93 patients found, 5 and 88, respectively, had T3 and T4 tumors. Clinically, 70 patients had lymph node metastases, while 18, 27, and 25 patients did not. whereas 18, 27, and 25 patients, respectively, had nodal statuses of N1, N2, and N3. In addition, 17 individuals had more than two distant metastatic sites, including peritoneal dissemination, while 76 patients had peritoneal dissemination alone. Five, twelve, one, and one of the 17 patients who had more than two distant metastatic sites each had metastases to the liver, distant lymph nodes, the ovary, and the bone, respectively. The first-line chemotherapy regimens for 56 and 37, respectively, of the 93 patients included in this study were taxane- and platinum-based, including intraperitoneal paclitaxel treatment. Trastuzumab was also given in conjunction with chemotherapy to 16 patients with gastric cancer that was human epidermal growth factor receptor 2 positive. Every three chemotherapy cycles, the tumor response was assessed using the Response Evaluation Criteria in Solid Tumors (RECIST). In the current investigation, tumor response was divided into two categories: Progressing Disease (PD) and non-PD. The length of time from the start of chemotherapy until death or the last follow-up was referred to as the "survival time." Patients having a performance status of at least 0-2, non-PD following chemotherapy, and tumors found to satisfy curative R0 resection were all candidates for conversion surgery. Therefore, before conversion surgery, patients underwent staging laparotomy or laparoscopy. Those who had to stage laparotomy or laparoscopy and had tumors with non-curative factors, such as P1 and CY1, were not candidates for conversion surgery.
Evaluation of pathological interventions
In Resected Samples following conversion surgery, tumor tissues were removed, and the proper therapy responses were evaluated using the Japanese categorization of stomach cancer. Given the significant advancements in cytotoxic medicines, molecular targeted therapies, and immune checkpoint inhibitors, chemotherapy has lately been suggested as the primary treatment for P1 gastric cancer patients even though they often undergo gastrectomy with lymphadenectomy [8]. Additionally, although conversion surgery has been put forth for chemotherapy responders, little is known regarding the clinical reasons and prognostic significance of surgical interventions among patients with P1 gastric cancer. Therefore, the current study looked back at the clinical information of P1 patients who had chemotherapy and evaluated the clinical importance of conversion surgery following chemotherapy.
References
- Colina, Prince V, Valettea PJ. Can mammographic assessments lead to considering density as a risk factor for breast cancer? European J Radiol. 82;2013;404–11.
- Kumar R. A Clinicopathologic Study of Breast Lumps in Bhairahwa, Nepal. Asi Pacific J Cancer Prevention, 11;2010.
- Mima B, Sangma M, Panda K, et al. A Clinico-Pathological Study on Benign Breast Diseases. J Clinical Diag Res. 2013;7(3): 503–6.
- Nassar, A, Visscher, DW, et al. Breast Cancer Res Treat (2015) 153: 397.
- Chopra B, Kaur V, Singh K, et al. Age shift: Breast cancer is occurring in younger age groups-Is it true? Clin Cancer Investig J. 2014 Nov 1;3(6):2278-0513.
- Maas P, Barrdahl M, Joshi AD, et al. Breast cancer risk from modifiable and nonmodifiable risk factors among white women in the United States. JAMA Oncology. 2016 Oct 1;2(10):1295-302.
- Leong, Zhen-Zhou S, Tse-Jia L, et al. Foulkes Is Breast Cancer the Same Disease in Asian and Western Countries?
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):359-86.